When women go through menopause, their bodies stop making estrogen and progesterone. For many, this brings hot flashes, night sweats, trouble sleeping, and mood swings that can make daily life harder. Hormone therapy (HRT) helps with these symptoms by replacing what the body no longer makes. But not all HRT is the same. The right combination depends on your body, your history, and your goals. And when you’re looking at generic options, the differences matter more than ever.
Why Combination Therapy Matters
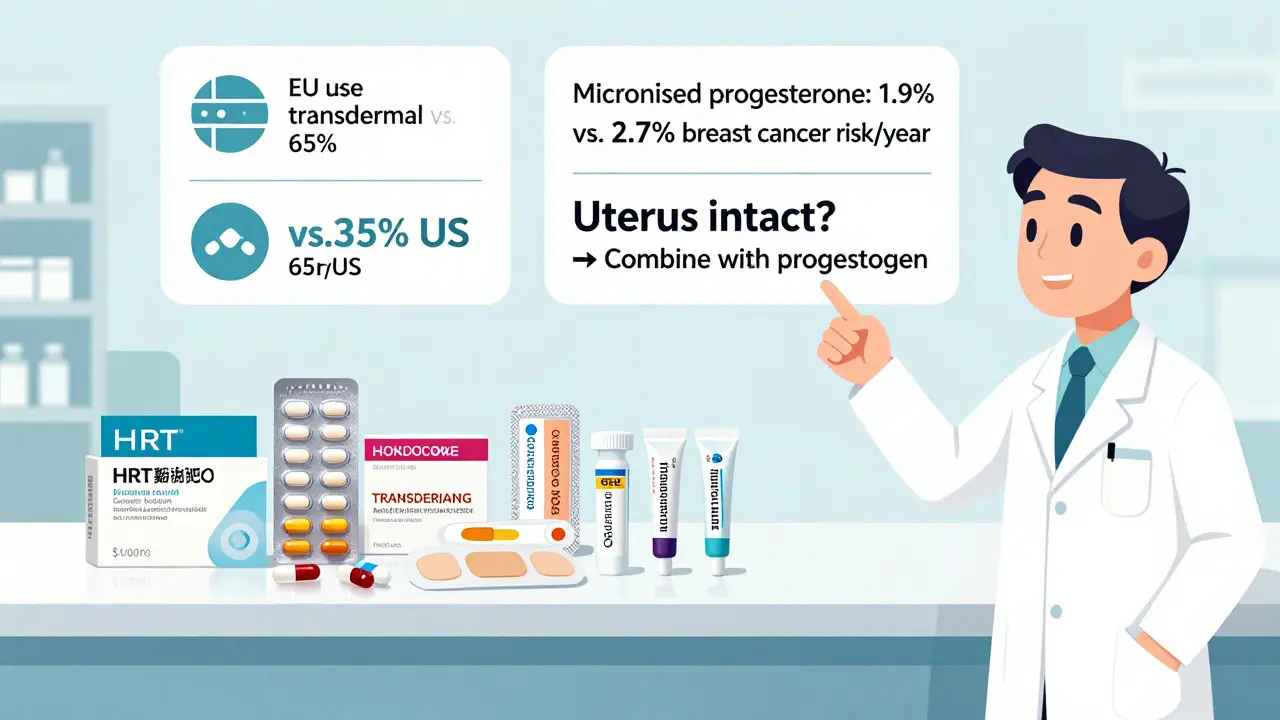
If you still have your uterus, you can’t take estrogen alone. It will cause the lining of your uterus to thicken. Over time, that increases your risk of uterine cancer. That’s why combination therapy-estrogen plus progestogen-is the standard for women with a uterus. For women who’ve had a hysterectomy, estrogen-only therapy is safe and often more effective. The goal isn’t just to relieve symptoms. It’s to do it safely. Research from the Women’s Health Initiative (WHI) changed how doctors think about HRT. Long-term use of certain combinations raised risks for blood clots, stroke, and breast cancer. But newer data shows those risks aren’t the same for everyone. For healthy women under 60 or within 10 years of menopause onset, the benefits often outweigh the risks-especially when you choose the right type and delivery method.Types of Combination Therapy: Sequential vs. Continuous
There are two main ways to combine estrogen and progestogen: sequential and continuous. Sequential combined HRT is for women who are still having periods or are in the early stages of menopause. You take estrogen every day, then add progestogen for the last 10 to 14 days of each month. This mimics a natural cycle and often causes a monthly bleed. Some women prefer this because it feels more familiar. Others find the monthly bleeding inconvenient. Continuous combined HRT is for women who haven’t had a period for a full year. You take both hormones every single day. No breaks. This usually stops bleeding after a few months. It’s simpler, and studies show it may lower your risk of colon cancer by about 18% and type 2 diabetes by 21%. The choice between them isn’t just about preference. It’s about your body’s stage. Starting continuous therapy too early can lead to unpredictable bleeding. Waiting too long to switch from sequential can mean unnecessary discomfort.Generic Hormones: What’s Actually in Your Prescription
Most HRT prescriptions today are generic. They’re cheaper, just as effective, and just as safe as brand-name versions. But not all generics are created equal. For estrogen, the most common generic forms are:- Conjugated estrogens (0.3mg, 0.45mg, 0.625mg tablets)
- Estradiol (0.5mg, 1mg tablets)
- Medroxyprogesterone acetate (2.5mg, 5mg, 10mg tablets)
- Micronized progesterone (100mg, 200mg capsules)
Delivery Methods: Pills vs. Patches vs. Gels
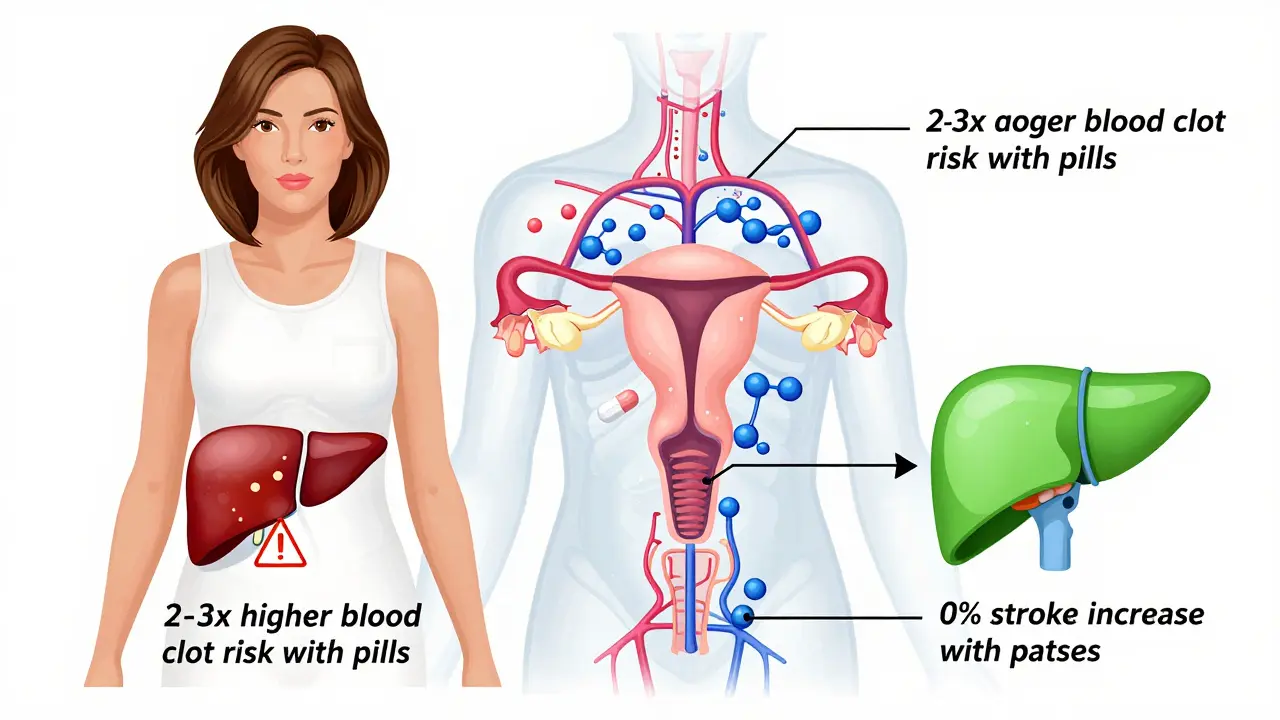
How you take your hormones affects your risk profile more than you might think. Oral tablets are the most common. But they pass through your liver first. That stresses your liver and increases clotting factors. Oral estrogen raises the risk of venous thromboembolism (VTE)-blood clots in the legs or lungs-by 2 to 3 times compared to non-oral methods. It also increases stroke risk by about 39% in women over 60. Transdermal options (patches, gels, sprays) go straight into your bloodstream through the skin. They skip the liver. That means:- Lower risk of blood clots
- No increase in stroke risk
- More stable hormone levels
Who Should Avoid HRT? What’s Risky?
HRT isn’t for everyone. You should avoid it if you have:- A history of blood clots or stroke
- Unexplained vaginal bleeding
- Active breast cancer or estrogen-sensitive cancer
- Severe liver disease
- History of heart attack or heart failure
Common Challenges and How to Handle Them
Many women stop HRT because of side effects. But most side effects are temporary. Breakthrough bleeding happens in 15-20% of women during the first 6 months. It’s usually not dangerous. But if it continues past 6 months, you need to see your doctor. It could mean your dose is too low, your progestogen isn’t right, or there’s another issue like polyps or fibroids. Mood changes can occur. Estrogen affects serotonin. Some women feel better. Others feel more anxious. If mood swings get worse, talk to your provider about switching estrogen types or delivery methods. Breast tenderness is common in the first few weeks. It often fades. If it doesn’t, your progestogen dose may be too high. Micronized progesterone tends to cause less tenderness than synthetic versions. Weight gain isn’t caused by HRT itself. But fluid retention and changes in metabolism can make it feel that way. Diet and movement matter more than the hormones.What’s New in 2025? The Future of HRT
The field is evolving. In 2023, the FDA approved a new transdermal patch that combines estrogen and progesterone in one patch. Early data from the TWIRP study suggests it may lower breast cancer risk compared to older oral combinations. The North American Menopause Society now recommends annual check-ins after 3-5 years of HRT. That means you’re not on it forever-you reassess every year. Research from the KEEPS study shows that starting transdermal estradiol within three years of menopause may actually protect your heart. It doesn’t speed up artery hardening like older studies feared. This is a big shift. New drugs are in the works. Tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs) aim to give symptom relief without raising cancer risk. They’re still in trials, but they represent the next step beyond estrogen and progestogen.How to Find the Right Fit
There’s no perfect HRT. There’s only the one that works best for you. Here’s how to find it:- Start with the lowest dose that controls your symptoms.
- Use transdermal estrogen if you have any risk of blood clots, stroke, or heart disease.
- Choose micronized progesterone over synthetic progestins if possible.
- Give it 3-6 months to settle. Don’t quit too soon.
- Reassess yearly. Your needs change.
Can I take generic hormone therapy instead of brand-name?
Yes. Generic hormone therapies are just as effective and safe as brand-name versions. They contain the same active ingredients in the same amounts. The only differences are in inactive ingredients like fillers or coatings, which rarely affect how the drug works. Most prescriptions today are generic because they cost far less-often 70-90% cheaper. Insurance usually prefers them too.
Is transdermal HRT safer than pills?
Yes, for most women. Transdermal estrogen (patches, gels, sprays) doesn’t pass through the liver first, so it doesn’t increase clotting factors like oral pills do. This means a much lower risk of blood clots, stroke, and heart attack. The NIH says oral HRT increases venous thromboembolism risk by 2-3 times compared to transdermal. If you have a history of clots, high blood pressure, or are over 60, transdermal is usually the safer choice.
Why do I need progestogen if I still have my uterus?
Estrogen alone causes the lining of your uterus to grow. Over time, that can lead to endometrial hyperplasia and eventually uterine cancer. Progestogen prevents this by regularly shedding the lining. Without it, estrogen therapy in women with a uterus is not safe. The NHS and FDA both require this warning on all estrogen products. The type and dose of progestogen depend on whether you’re still having periods or not.
How long should I stay on hormone therapy?
There’s no set time limit. Most women take HRT for 2-5 years to get through the worst symptoms. But some need it longer. The key is to reassess every year. If your hot flashes are gone and your bone density is stable, you might be able to stop. If symptoms return, you can restart at the lowest effective dose. The goal isn’t lifelong use-it’s using it only as long as the benefits outweigh the risks.
Does HRT cause breast cancer?
Combined HRT (estrogen + progestogen) slightly increases breast cancer risk, but only after 5+ years of continuous use. The Cleveland Clinic estimates less than 1 in 1,000 women will develop breast cancer because of HRT. Risk is higher with synthetic progestins than with micronized progesterone. Estrogen-only therapy doesn’t raise breast cancer risk. The increase is small compared to other factors like age, weight, and family history. If you’re concerned, talk to your doctor about using the lowest dose for the shortest time needed.
What should I do if I have breakthrough bleeding?
Breakthrough bleeding is common in the first 6 months, especially with sequential therapy. It often resolves on its own. But if it lasts longer than 6 months, or if it’s heavy, frequent, or after sex, see your doctor. It could mean your dose is too low, your progestogen isn’t right, or there’s another issue like polyps, fibroids, or infection. A pelvic ultrasound or endometrial biopsy may be needed to rule out serious causes.

12 Comments
steve sunio
lol so now we got a 10-page essay on HRT like it's a NASA mission. just take the damn pill or don't. why does everyone turn menopause into a biochemistry thesis? my aunt took generics for 3 years and said it felt like she got her life back. no need to overthink it.
Robert Petersen
This is actually one of the clearest breakdowns I’ve read on HRT. I’ve been helping my mom navigate this and I kept getting conflicting advice from different docs. The part about transdermal vs oral? Game changer. She switched to a patch last month and her night sweats are basically gone. Also, micronized progesterone is a vibe-way less bloating than the synthetic stuff. Seriously, thank you for this.
Luke Trouten
The distinction between sequential and continuous combined HRT is critical, yet frequently misunderstood. Sequential therapy mimics the endogenous ovarian cycle, inducing withdrawal bleeds that, while psychologically reassuring to some, are physiologically unnecessary after menopausal transition. Continuous combined regimens, by contrast, suppress endometrial proliferation more effectively and reduce long-term endometrial hyperplasia risk. The clinical data from the WHI and subsequent meta-analyses support this paradigm shift, particularly in women over 55 with stable symptomatology.
Gabriella Adams
I’m a nurse practitioner and I see this every day. Women are terrified of HRT because of headlines from 2002. But the science has evolved. Transdermal estrogen? Low risk. Micronized progesterone? Safer than synthetic. Starting within 10 years of menopause? Benefits outweigh risks for most. The real tragedy is how many women suffer in silence because they think HRT = cancer. It’s not. It’s medicine. And it’s okay to need it.
Jonathan Noe
You guys are overcomplicating this. The answer is simple: if you have a uterus, you need progestogen. Period. No exceptions. And if you’re over 60 or have a clotting history, skip the pills. Go transdermal. Generic? Totally fine. I’ve prescribed hundreds of these. The only difference between brand and generic is the color of the pill. Literally. Don’t let the marketing scare you.
christian jon
I can’t believe people are still taking HRT like it’s a magic wand. You’re basically flooding your body with hormones and hoping for the best? What about the 18% rise in breast cancer risk? And don’t even get me started on the liver damage from oral pills-your liver is NOT a filter for your bad life choices! I’ve seen women turn into emotional volcanoes on HRT. And now you’re telling me to just ‘reassess yearly’? That’s not a plan-that’s a gamble with your body!
Steve DESTIVELLE
The question is not whether hormone therapy works but whether the human body was ever meant to be artificially prolonged beyond its natural rhythm. Evolution did not design us to live 30 years past menopause. The modern obsession with symptom suppression is a symptom of a culture that fears aging more than death itself. The bleeding, the mood swings, the hot flashes-they are not malfunctions. They are signals. To silence them with chemistry is to silence the voice of biology. Perhaps we should listen instead of replace.
Stephon Devereux
I’ve been on transdermal estradiol and micronized progesterone for 4 years. Started at 52. My hot flashes vanished in 2 weeks. My sleep improved. My anxiety? Gone. I tried the pill first-got dizzy and bloated. Switched to the patch and it was like a new person. The monthly bleed? Minimal. The cost? $12/month with insurance. I wish I’d done this 10 years ago. If you’re hesitating, just try it for 3 months. Worst case? You stop. Best case? You feel human again.
Alyssa Williams
I switched to micronized progesterone after my dr suggested it and my breast tenderness disappeared. Also, the patch doesn’t stick? Use a little medical tape. It’s not rocket science. And yes, generics are fine. My pharmacy gave me a different brand each time and I didn’t notice a difference. Stop overthinking. Your body knows what it needs.
Ojus Save
I read this and thought ok but then i forgot what i read because my phone died and i was too lazy to charge it. but the part about transdermal being better than pills makes sense. my mom had a clot and they switched her and she said it was like night and day. also why do we even have brand names if the active stuff is the same? capitalism is weird.
Jason Pascoe
I appreciate the nuance here. A lot of online advice is either fearmongering or oversimplifying. The fact that transdermal estrogen reduces stroke risk by eliminating first-pass liver metabolism is clinically significant. And the 18% reduction in colon cancer risk with continuous therapy? That’s not a side effect-that’s a therapeutic bonus. We need more of this balanced, evidence-based talk.
Annie Joyce
Just want to say-breakthrough bleeding isn’t ‘weird.’ It’s normal. I had it for 5 months. Thought I was dying. Went to my doc, they tweaked my dose, and now I’m fine. Also, if you’re using gel, don’t wear a tank top right after. My husband got a little hormone transfer and he was weirdly emotional for 3 hours. True story. Wash hands. Wait 60 mins. Don’t be that person.