Understanding the Connection between Diabetes and Osteoporosis
As a person who is always keen on learning about health-related topics, I recently came across some surprising information about the relationship between diabetes and osteoporosis. I was astonished to find out that these two seemingly unrelated conditions are closely connected. In this article, I will discuss the connection between diabetes and osteoporosis, and how the two can impact each other.
But first, let's understand the basics of these two conditions. Diabetes is a chronic disease that affects the way our bodies process sugar. There are two types of diabetes: Type 1, which is usually diagnosed in childhood, and Type 2, which typically develops in adulthood. On the other hand, osteoporosis is a condition that weakens our bones, making them more susceptible to fractures and breaks.
How Diabetes Affects Bone Health
Diabetes can have a significant impact on our bone health. High blood sugar levels can lead to inflammation, which in turn can weaken the bones. Moreover, diabetes can also affect the blood vessels, reducing the blood supply to the bones. This can result in a decrease in bone density and an increased risk of fractures.
Furthermore, people with diabetes often have lower levels of insulin, a hormone that plays a crucial role in bone formation. Insulin helps in the absorption of calcium, which is essential for strong bones. When there is a lack of insulin, our bones may not get the required amount of calcium, leading to weaker bones and an increased risk of osteoporosis.
Diabetes Medications and Their Impact on Bone Health
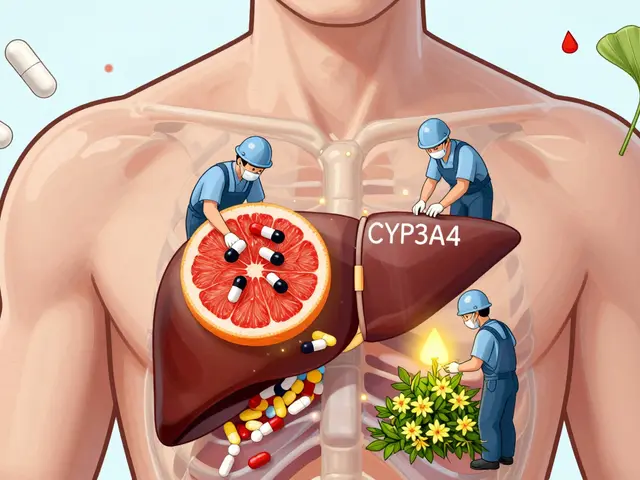
Some medications used to treat diabetes can also have an impact on our bone health. For instance, thiazolidinediones, a class of drugs used to treat type 2 diabetes, have been associated with an increased risk of bone fractures. These medications can cause a decrease in bone density, thus making our bones more susceptible to fractures.
However, it is important to note that not all diabetes medications have negative effects on bone health. Some medications, such as metformin, have been shown to have a protective effect on the bones. Therefore, it is essential to consult with your healthcare provider to choose the right medication for your specific needs.
Preventing Osteoporosis in Diabetic Patients
Given the connection between diabetes and osteoporosis, it is essential for people with diabetes to take steps to protect their bone health. One of the most important measures is to maintain good blood sugar control. Keeping blood sugar levels within the target range can help reduce inflammation and prevent damage to the blood vessels, thus promoting bone health.
Additionally, adopting a healthy lifestyle can also help in preventing osteoporosis. This includes consuming a balanced diet rich in calcium and vitamin D, engaging in regular weight-bearing exercises, and avoiding smoking and excessive alcohol consumption. It is also essential to have regular check-ups with your healthcare provider to monitor your bone health and make any necessary adjustments to your treatment plan.
Recognizing the Signs of Osteoporosis in Diabetic Patients
It is crucial for people with diabetes to be aware of the signs and symptoms of osteoporosis. This is because early detection can help in the implementation of appropriate interventions to prevent further bone loss. Some common symptoms of osteoporosis include back pain, loss of height, stooped posture, and frequent fractures.
If you suspect that you may have osteoporosis, it is important to consult with your healthcare provider. They can perform tests to assess your bone density and determine the best course of action for your specific situation. Remember, taking care of your bone health is just as important as managing your diabetes, and being proactive can help prevent complications down the line.


16 Comments
Scott Ring
Hey everyone, great info on the diabetes‑osteoporosis link. I’ve seen a few patients where tighter sugar control really helped their bone density. Keep sharing these insights, they’re super helpful for folks trying to stay on top of both conditions.
Shubhi Sahni
Wow, this article really opened my eyes, the connection between high glucose levels and bone health is profound, isn’t it?, and the role of insulin in calcium absorption is fascinating, too! It’s essential to monitor both blood sugar and bone density, especially for those on long‑term medication, and to discuss preventive strategies with healthcare providers, now more than ever!
Danielle St. Marie
Honestly, most laypeople have no clue how diabetes can sabotage their skeleton – it’s a textbook case of systemic neglect 😒. In the US we have the resources to get DEXA scans, yet many still ignore the guidelines 🇺🇸. If you’re not taking metformin, you’re missing out on its bone‑protective benefits – shame on you! 💪
keerthi yeligay
Diabetes hurt bones cause inflammation. Insulin low = less calcium absorbtion. Exercise helps, so do vitamin D. Nice article, but watch for typos.
Peter Richmond
The interplay between hyperglycemia and osteoclastic activity is well documented. Maintaining euglycemia therefore constitutes a primary preventive measure against osteoporotic fractures. I appreciate the thorough overview provided herein.
Bonnie Lin
Great summary of the risks. Simple steps like diet and weight‑bearing exercise can make a difference.
sara fanisha
Hey folks! Loving the practical tips – especially the reminder to get some sunshine for vitamin D. Stay positive and keep moving, your bones will thank you!
Tristram Torres
Diabetes can hurt your bones. Keep blood sugar low and do some walking. It helps.
Jinny Shin
While your enthusiasm is noted, the gravity of metabolic bone disease demands a more scholarly discourse. One cannot simply “share insights” without delving into the molecular pathways that govern osteoblast differentiation.
deepak tanwar
Although the article emphasizes monitoring, I must point out that excessive screening can lead to unnecessary anxiety and healthcare costs. It would be prudent to balance vigilance with clinical judgment.
Abhishek Kumar
Sounds like a lot of hype.
hema khatri
Wow!! This is such an important reminder!! Make sure you get your calcium, vitamin D, and check your blood sugar regularly!! Stay healthy!!
Jennell Vandermolen
Agreed the link is clear – keeping glucose stable really does protect bone health. Good reminder to talk to doctors about bone density tests.
Mike Peuerböck
The nexus between glycemic control and skeletal integrity is a cornerstone of contemporary endocrinology.
The patients who achieve sustained euglycemia often exhibit markedly higher bone mineral density values.
Conversely chronic hyperglycemia accelerates collagen cross‑linking abnormalities that compromise bone resilience.
Insulin beyond its metabolic actions serves as an anabolic agent stimulating osteoblast proliferation.
Deficiencies in insulin signaling thus translate into diminished calcium incorporation within the hydroxyapatite lattice.
Certain thiazolidinediones impair the differentiation of mesenchymal stem cells toward the osteoblastic lineage.
This pharmacologic effect predisposes susceptible individuals to vertebral compression fractures.
Metformin however appears to bolster mitochondrial function within bone cells and may confer a protective advantage.
Lifestyle interventions such as resistance training amplify mechanical loading and fortify trabecular architecture.
Adequate intake of calcium‑rich foods synergizes with vitamin D synthesis to enhance mineralization.
Regular assessment using dual‑energy X‑ray absorptiometry provides quantitative insight into bone health trends.
Clinicians should integrate bone health metrics into the comprehensive management plan for diabetic patients.
Patient education regarding fall prevention strategies further mitigates fracture risk.
Emerging research into sclerostin inhibitors holds promise for targeted therapeutic advances.
Ultimately a multidisciplinary approach unites endocrinology nutrition and physiotherapy to safeguard the skeletal system.
Simon Waters
Some pharma companies push meds that actually weaken bones while hiding the data – keep an eye on what they’re not telling you.
Vikas Kumar
Our nation’s health policies often ignore the silent threat of diabetic bone loss – it’s time to demand better screening.