When someone is diagnosed with cancer, chemotherapy is often one of the first treatments discussed. It’s not magic - but it’s powerful. Chemotherapy drugs are designed to kill fast-growing cells, which includes cancer cells. But they don’t stop there. They also hit healthy cells that divide quickly - like those in your hair follicles, gut lining, and bone marrow. That’s why side effects like hair loss, nausea, and low blood counts happen. And here’s the part no one talks about enough: chemotherapy doesn’t just interact with your body. It interacts with everything else you’re taking.
How Chemotherapy Works - and Why It’s So Harsh
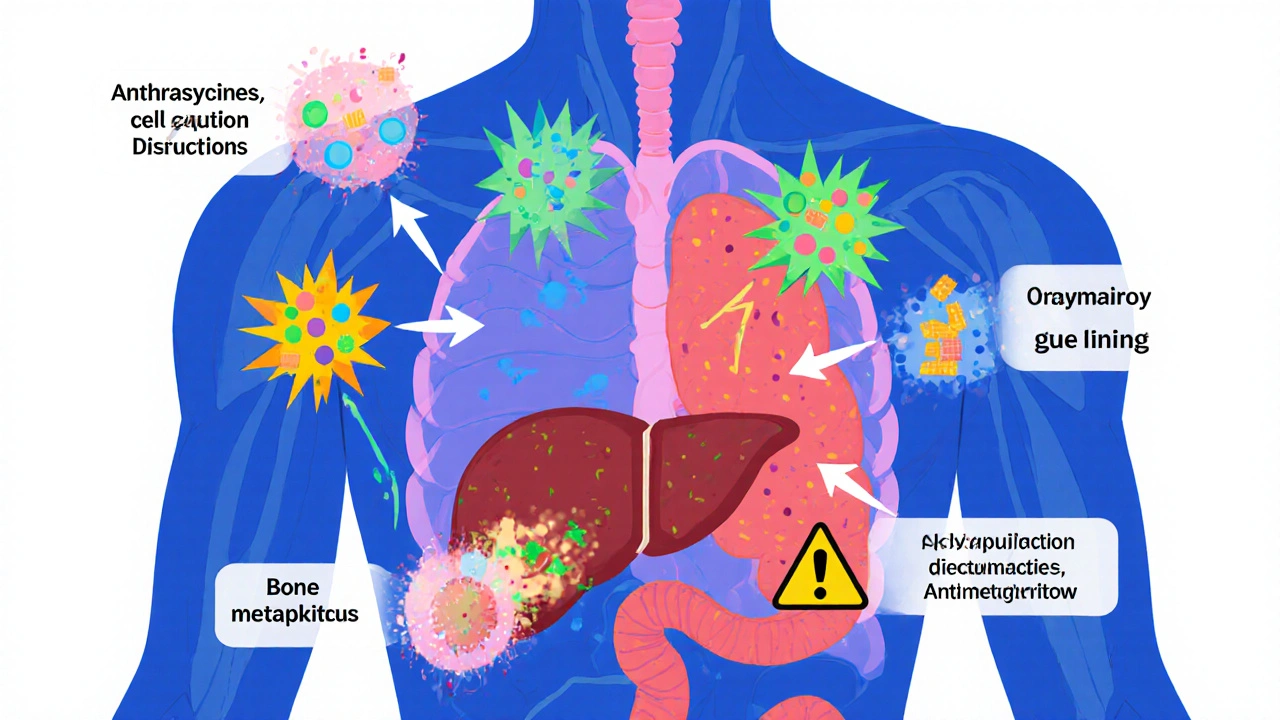
Chemotherapy isn’t one drug. It’s over 100 different compounds, grouped into classes based on how they attack cancer. Anthracyclines like doxorubicin tear apart DNA. Alkylating agents like cyclophosphamide mess with cell replication. Antimetabolites like methotrexate trick cells into using fake building blocks, so they can’t grow. Each class has its own risks, its own schedule, and its own list of dangerous interactions. Most chemo is given in cycles - every 2 to 4 weeks - because your body needs time to recover. The goal? Kill as many cancer cells as possible without killing the patient. That’s why dosing is precise. It’s calculated by body surface area (mg/m²), not just weight. A 5% error can mean the difference between effective treatment and life-threatening toxicity. The CDC estimates that 650,000 people in the U.S. get chemotherapy each year. More than half of all cancer patients will receive it at some point. And while newer treatments like immunotherapy and targeted drugs are rising, chemotherapy still forms the backbone of curative treatment for most solid tumors and blood cancers. In fact, the NCCN guidelines still list chemo as the top recommendation for early-stage breast cancer, reducing recurrence by 30-40%.Drug Interactions: The Silent Killer
Here’s where things get dangerous. Cancer patients aren’t just on chemo. They’re often taking pain meds, antibiotics, heart drugs, antidepressants, even over-the-counter supplements. And many of these can mess with how chemo works - sometimes in deadly ways. Take St. John’s wort. It’s a popular herbal remedy for mild depression. But it activates an enzyme in the liver called CYP3A4, which breaks down chemo drugs like docetaxel and etoposide. If you take St. John’s wort, your chemo gets cleared from your body too fast. It stops working. And you don’t even know it. Or consider grapefruit juice. It blocks another liver enzyme, CYP3A4, the opposite effect. This causes chemo drugs like paclitaxel and vinca alkaloids to build up in your blood. Toxic levels. You could end up in the ICU with nerve damage, low blood pressure, or organ failure. Even common antibiotics like erythromycin or antifungals like fluconazole can interfere. They slow down the same liver pathways that clear chemo. One study found that patients on fluconazole while receiving paclitaxel had 40% higher drug levels in their blood - enough to double the risk of severe neuropathy. And it’s not just prescription drugs. Anti-nausea meds like ondansetron can prolong the QT interval on your heart’s ECG. Combine that with certain chemo drugs like doxorubicin or cisplatin - both of which also affect heart rhythm - and you’re playing Russian roulette with your heartbeat.What You’re Not Told About Oral Chemo
More and more chemo is now given as pills - like capecitabine, temozolomide, or lenalidomide. It sounds easier. No IVs. No clinic visits. But it’s riskier. Why? Because patients forget. Or skip doses because they feel sick. Or take it with food when they’re supposed to take it on an empty stomach. Non-adherence rates for oral chemo? Between 20% and 30%. That’s not just poor compliance - it’s treatment failure. And here’s the kicker: oral chemo interacts with food just like drugs. Capecitabine must be taken within 30 minutes after eating. If you take it on an empty stomach, you get severe diarrhea. If you take it with a high-fat meal, you absorb too much - and risk hand-foot syndrome, a painful, blistering reaction. A 2023 study in the Journal of Oncology Pharmacy Practice found that patients who received pharmacist-led counseling on oral chemo adherence had 40% fewer treatment interruptions and 30% fewer hospitalizations.
What’s Really in Your Medicine Cabinet?
Most patients don’t think to tell their oncologist about their vitamins. But here’s the truth: vitamin C in high doses can protect cancer cells from radiation and some chemo drugs. Antioxidants like vitamin E and selenium might reduce the effectiveness of treatment. Even something as simple as aspirin can be dangerous. It increases bleeding risk when combined with drugs like cisplatin or carboplatin, which already lower platelet counts. And if you’re on blood thinners like warfarin? Chemo can make your INR spike or crash unpredictably. The American Society of Health-System Pharmacists says 98% of U.S. cancer centers now use board-certified oncology pharmacists to screen for interactions. But outside major hospitals? Many community clinics still rely on doctors who aren’t trained in oncology pharmacology.How to Protect Yourself
You don’t need to be a scientist to stay safe. Here’s what actually works:- Make a complete list of everything you take - prescription, OTC, supplements, herbs, even CBD oil. Bring it to every appointment.
- Ask your oncologist or pharmacist: “Could this interact with my chemo?” Don’t assume they know. Many don’t.
- Never start or stop anything without telling your cancer team - not even a daily multivitamin.
- If you’re on oral chemo, take it exactly as directed. No exceptions. No “I’ll take it later.”
- Keep a symptom journal. Note when nausea, fatigue, or numbness starts. That helps your team adjust dosing before it’s too late.
When Chemo Isn’t Enough - And What Comes Next
Chemotherapy isn’t perfect. It works brilliantly in some cancers - like acute lymphoblastic leukemia, where remission rates exceed 80%. But in others - like pancreatic cancer - single-agent gemcitabine only helps 10-20% of patients. That’s why combination therapy is standard. The BEP regimen for testicular cancer (bleomycin, vinblastine, cisplatin) cures over 90% of early-stage cases. Why? Because each drug attacks cancer in a different way. Resistance has a harder time developing. But even then, resistance happens. About 30% of patients develop chemo resistance within the first treatment cycle. That’s why new tools are emerging. Antibody-drug conjugates like sacituzumab govitecan deliver chemo directly to cancer cells, reducing side effects by targeting only the tumor. Circulating tumor DNA testing now helps doctors stop chemo early if the cancer is gone - avoiding months of unnecessary toxicity.Quality of Life: The Real Cost
Let’s be honest. Chemo is brutal. A 2022 analysis of over 1,200 patients found:- 68% had severe fatigue
- 52% still got nausea despite anti-nausea drugs
- 41% developed nerve damage from taxanes - sometimes permanent
Final Thoughts: You’re Not Alone
Chemotherapy is complex. It’s powerful. It’s dangerous. But it’s also one of the most effective tools we have against cancer. The key isn’t avoiding it. It’s managing it - smartly, safely, with full awareness of what’s in your body and what it’s doing to you. Talk to your pharmacist. Ask questions. Write things down. Bring someone with you to appointments. Your life depends on it - not just the chemo, but how you take it, what you take with it, and whether your team knows everything you’re using. This isn’t just medicine. It’s teamwork. And you’re a vital part of it.Can I take over-the-counter painkillers while on chemotherapy?
Some are safe, others aren’t. Acetaminophen (Tylenol) is generally okay for mild pain. But NSAIDs like ibuprofen or naproxen can increase bleeding risk, especially with chemo drugs that lower platelets. Always check with your oncology team before taking anything - even a simple aspirin.
Does grapefruit juice really interfere with chemo?
Yes. Grapefruit and its juice block enzymes in your liver that break down many chemotherapy drugs, including paclitaxel, docetaxel, and vinca alkaloids. This causes drug levels to rise dangerously high, increasing side effects like nerve damage, low blood pressure, or even organ toxicity. Avoid grapefruit entirely during chemo unless your doctor says otherwise.
Why do I need to take chemo on an empty stomach sometimes?
Some oral chemo drugs, like capecitabine, are absorbed differently based on food. Taking them with a high-fat meal can cause too much absorption, leading to severe side effects like hand-foot syndrome. Others need food to reduce stomach upset. Your prescription instructions are specific for a reason - follow them exactly.
Can herbal supplements like turmeric or CBD help with chemo side effects?
There’s no solid evidence that herbs like turmeric or CBD improve chemo outcomes - and they might interfere. Turmeric can affect liver enzymes that process chemo. CBD can interact with drugs metabolized by CYP3A4, potentially raising chemo levels. Always tell your oncologist if you’re using any supplement. Don’t assume it’s safe just because it’s natural.
What should I do if I miss a dose of oral chemotherapy?
Don’t double up. Call your oncology team immediately. Missing a dose can reduce effectiveness and increase resistance. But taking extra can cause dangerous toxicity. Your provider will tell you whether to skip, adjust, or resume on schedule - based on the specific drug and timing.
How do I know if my chemo is working?
You won’t feel it. Chemo doesn’t always cause immediate side effects - and side effects don’t mean it’s working. Response is measured through scans, blood tests, and tumor markers. Circulating tumor DNA testing is now used in some cases to detect if cancer cells are still present after treatment. Always rely on your doctor’s tests, not how you feel.
Are there long-term risks from chemotherapy?
Yes. Some chemo drugs can damage the heart (anthracyclines), lungs (bleomycin), kidneys (cisplatin), or nerves (taxanes). There’s also a small risk of developing a second cancer later in life. That’s why lifetime dose limits exist - like the 550 mg/m² cap for doxorubicin. Regular follow-up care is critical, even years after treatment ends.
Next Steps: What to Do Today
If you or someone you love is starting chemotherapy:- Make a complete list of every medication, supplement, and herb you take - including doses and frequencies.
- Bring that list to your oncologist and ask: “Which of these could interact with my chemo?”
- Ask for a consultation with an oncology pharmacist - they specialize in these interactions.
- If you’re on oral chemo, set phone alarms to take it on time. Don’t rely on memory.
- Keep a symptom journal. Note fatigue, nausea, numbness, or rashes. Bring it to every visit.






15 Comments
Katy Bell
I had chemo for breast cancer last year. The worst part wasn't the nausea-it was realizing I'd been taking turmeric capsules 'for inflammation' and had no idea they could mess with my drugs. My oncology pharmacist nearly had a heart attack when I mentioned it. Don't be like me. Write everything down. Even the 'harmless' stuff.
Ragini Sharma
grapefruit juice = bad. got it. but can i still have orange juice? or is that also a trap? also why does everyone act like st. johns wort is some secret weapon when its basically herbal weed?
Linda Rosie
Adherence to oral chemotherapy protocols significantly impacts treatment efficacy and toxicity profiles. Pharmacists are essential in this process.
Vivian C Martinez
You’ve got this. Every time you write down your meds, every time you ask that question, you’re fighting harder than most people realize. Keep going. Your team needs you to be this detailed. It matters.
Ross Ruprecht
Wow. So basically, if you're not a pharmacist or a doctor, you shouldn't be allowed to take pills? This post feels like a 10-page warning label for people who can't read.
Bryson Carroll
Chemo is just glorified poison and everyone acts like it's a miracle cure. You're just trading one set of problems for another. The real question is why we still use this 1950s tech when we have targeted therapies. Also, your 'symptom journal' is cute. It won't stop your kidneys from failing
Jennifer Shannon
Let me tell you something about cultural attitudes toward medicine-back in my village in Nigeria, we used to say, 'If it's not in the earth, it's not medicine.' Now I sit here in Ohio, surrounded by pills, supplements, and IV bags, wondering if we lost something when we stopped listening to the body and started trusting the lab report. I’m not saying go back to roots-no, no-but I do think we’ve forgotten that healing isn’t just chemistry. It’s rhythm. It’s timing. It’s knowing when to stop. And no algorithm can tell you that.
Suzan Wanjiru
Oral chemo is a nightmare if you're on a tight schedule. I missed a dose because I was at work and didn't realize it needed to be taken 30 mins after food. Ended up in the ER with diarrhea and dehydration. Now I have alarms for everything. And yes I told my doc about my CBD oil. He didn't blink. Just said 'okay, stop.'
Kezia Katherine Lewis
Drug-drug interactions mediated by CYP450 isoenzymes, particularly CYP3A4 and CYP2C8, are clinically significant in oncology pharmacokinetics. Concurrent administration of CYP3A4 inducers (e.g., St. John’s wort) or inhibitors (e.g., fluconazole) can alter the AUC and Cmax of taxanes and anthracyclines, necessitating dose adjustments or avoidance strategies.
Henrik Stacke
Remarkable how such a complex, life-saving intervention remains so poorly understood by the general public. The responsibility lies not only with patients but with healthcare systems to provide accessible, clear, and consistent education. A simple pharmacist consultation should be mandatory-not optional.
Manjistha Roy
My aunt took chemo and didn't tell her doctor about the ashwagandha she was using for stress. Three weeks later she had liver enzyme spikes. She’s fine now, but it scared us all. Please, if you're taking anything-even a tea-say something. Your doctor isn't judging. They're trying to keep you alive.
Jennifer Skolney
Just had my first chemo session. I’m scared but also weirdly calm? I made a color-coded spreadsheet of all my meds and set reminders for everything. I even printed out the chemo schedule and taped it to my fridge. If I can do this, anyone can. 💪
JD Mette
I’m not sure I’ve ever seen a post this thorough. I’ve been through this twice. The part about the pharmacist consultation? That’s the one thing I wish I’d done earlier. It’s not about being smart. It’s about being safe.
Olanrewaju Jeph
As a nurse in Lagos, I’ve seen patients stop chemo because they heard 'herbs heal better.' I’ve also seen them die because they took something that made their drugs toxic. This post is a lifeline. Share it. Translate it. Make sure everyone knows.
Dalton Adams
Oh wow, so the real issue isn't cancer-it's that people can't read a label? You need a PhD just to take a pill now? And why are you praising pharmacists like they're wizards? I've seen oncologists who don't know the difference between CYP3A4 and a coffee maker. This whole thing is a circus. Also, I take CBD for sleep and my chemo is fine. So there.