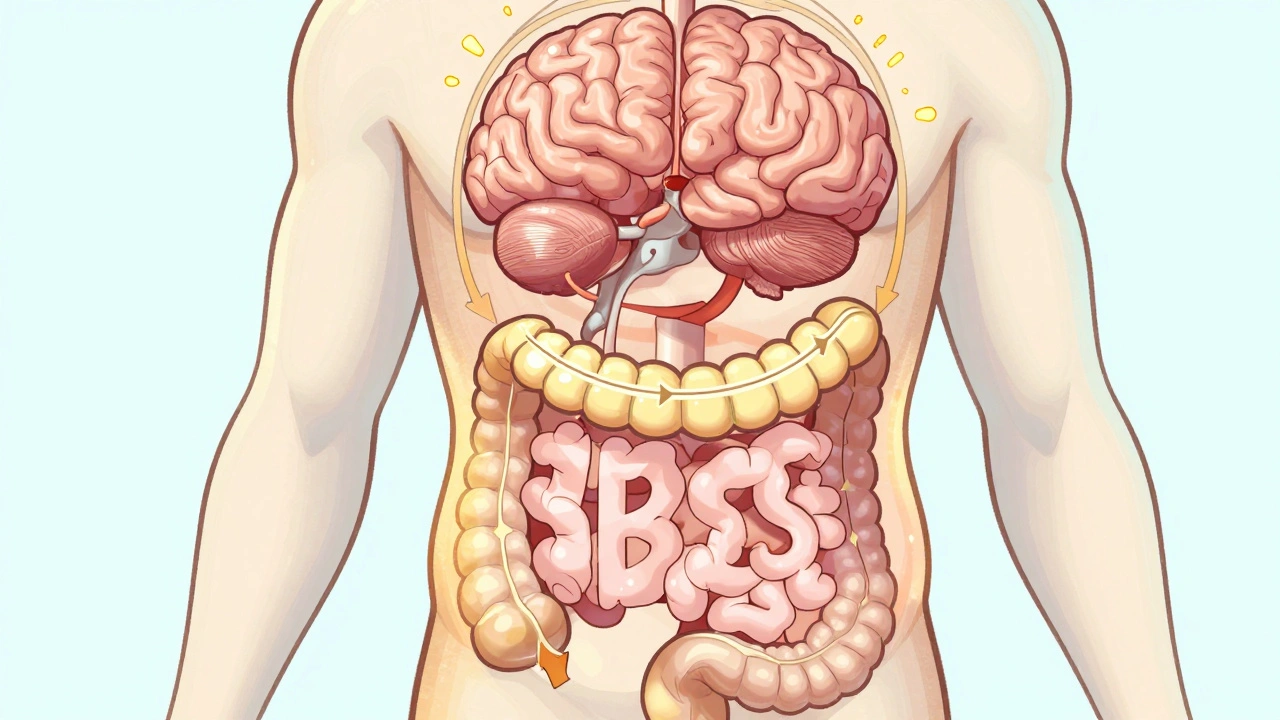
Living with irritable bowel syndrome (IBS) means dealing with more than just occasional stomach upset. For millions of people, it’s a constant balancing act between what you eat, how you feel, and whether you can leave the house without planning for an emergency bathroom stop. Unlike conditions like Crohn’s or colitis, IBS doesn’t show up on scans or blood tests. There’s no visible damage, no infection, no tumor. But the pain, bloating, and unpredictable bowel changes are very real-and they can wreck your daily life.
What Exactly Is IBS?
IBS isn’t a disease you catch or a glitch you fix. It’s a functional disorder, meaning your digestive system looks normal but doesn’t work right. The Rome IV criteria, used by doctors worldwide since 2016, define IBS as recurring abdominal pain at least one day a week over the last three months, linked to bowel movements. That pain often eases after going to the bathroom, and your stool might suddenly become looser or harder than usual.
It’s not rare. About 1 in 7 people globally have IBS. In Australia, that’s roughly 2.5 million people. Most are diagnosed before age 50, often in their 20s or 30s. Women are diagnosed more often than men-about 2 out of every 3 patients. That doesn’t mean men don’t get it; it just means women are more likely to seek help and be diagnosed.
There’s no cure. But that doesn’t mean you’re stuck suffering. With the right approach, most people find significant relief. The goal isn’t to eliminate IBS-it’s to manage it so it doesn’t control your life.
Common Symptoms and Subtypes
IBS doesn’t look the same for everyone. Doctors classify it into three main types based on your most common bowel pattern:
- IBS-D (diarrhea-predominant): About 40% of people. You might have sudden urges, watery stools, and feel like you can’t make it to the bathroom in time.
- IBS-C (constipation-predominant): Around 35%. You struggle to pass stool, feel bloated, and still feel like you haven’t fully emptied even after going.
- IBS-M (mixed): Roughly 25%. You alternate between diarrhea and constipation, sometimes within the same day.
Beyond bowel changes, many people deal with:
- Abdominal cramping that improves after a bowel movement
- Bloating and visible swelling in the stomach
- Excess gas and frequent burping
- Mucus in the stool
- Sensation of incomplete evacuation
And it’s not just your gut. Up to 70% of people with IBS also report symptoms outside the digestive system: a lump in the throat (globus), heartburn, nausea, chest pain that feels like a heart issue, or even unexplained fatigue. These aren’t in your head-they’re part of how your gut and brain talk to each other.
What Triggers IBS Flare-Ups?
IBS doesn’t flare up randomly. There are clear triggers, and knowing yours is half the battle.
Diet is the biggest one. About 70% of people find that certain foods make their symptoms worse. The biggest culprits? High-FODMAP foods. That’s a mouthful, but it just means certain carbs that ferment in your gut-like onions, garlic, wheat, dairy, apples, and artificial sweeteners. A low-FODMAP diet, guided by a dietitian, helps 50-75% of people cut symptoms dramatically.
Stress and emotions are just as powerful. If you’ve ever had a stomachache before a big presentation or noticed your IBS flares during a tough week, you’re not alone. Around 60-80% of people link symptom severity to stress levels. It’s not psychological-it’s biological. Your gut has its own nervous system, and it reacts strongly to anxiety, depression, or even chronic pressure.
Hormones play a role too, especially for women. About two-thirds of female patients report worse symptoms around their period. Estrogen and progesterone affect gut motility, and when those levels shift, so do your bowels.
Antibiotics can trigger IBS in about 1 in 4 people. They wipe out good bacteria along with the bad, and sometimes your gut doesn’t bounce back. That’s why some people develop IBS after a course of antibiotics for a simple infection.
How Is IBS Diagnosed?
There’s no single test for IBS. Diagnosis is about ruling out other things. Your doctor will start with your symptoms, medical history, and a physical exam. Then they’ll look for red flags that mean something else is going on:
- Onset after age 50
- Unexplained weight loss
- Bloody stools
- Anemia (low iron)
- Family history of colon cancer or IBD
- Diarrhea that wakes you up at night
If any of these are present, you’ll likely need tests: blood work for celiac disease, stool tests for inflammation, a hydrogen breath test for bacterial overgrowth, or a colonoscopy if you’re over 45.
For most people without red flags, diagnosis comes from symptom patterns alone. It can take years-on average, 6.2 years from first symptom to diagnosis-because many people assume it’s just "a sensitive stomach." Don’t wait. If your symptoms are recurring and affecting your life, get it checked.
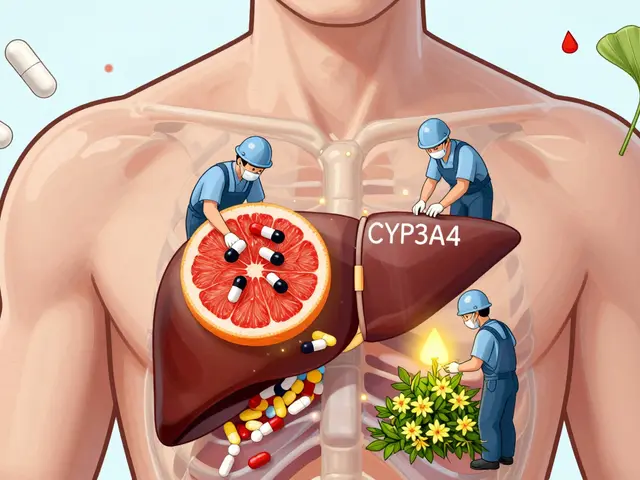
Medications for IBS: What Actually Works?
Medication isn’t a magic bullet, but it can help when used correctly for your subtype.
For IBS-D (diarrhea):
- Loperamide (Imodium): Over-the-counter. Helps slow diarrhea in about 60% of people, but doesn’t touch pain or bloating.
- Rifaximin (Xifaxan): A non-absorbed antibiotic. Taken for 14 days, it reduces bloating and diarrhea in 40-50% of people. Works by calming gut bacteria.
- Eluxadoline (Viberzi): FDA-approved for IBS-D. Reduces both pain and diarrhea, but carries a small risk of pancreatitis. Not for people without a gallbladder.
For IBS-C (constipation):
- Linaclotide (Linzess): Taken daily. Draws water into the gut, softens stool, and reduces pain. About 30-40% of people hit the target of three full bowel movements per week.
- Plecanatide (Trulance): Similar to linzess, but often better tolerated. Also increases bowel movements and eases discomfort.
- Lubiprostone (Amitiza): A chloride channel activator. Helps with constipation and bloating in about 25-30% of users.
For pain and overall symptoms:
- Antispasmodics (hyoscine, dicyclomine): These relax gut muscles. They help with cramping in about 55% of people, but can cause dry mouth or dizziness.
- Low-dose antidepressants (amitriptyline, nortriptyline): Not for depression. At doses of 10-30 mg at night, they calm nerve signals between gut and brain. Studies show 40-50% improvement in pain and overall symptoms. Takes 4-8 weeks to work.
Probiotics? Only one strain has solid proof: Bifidobacterium infantis 35624. It improved symptoms in 35% of people in trials-better than placebo, but not a miracle. Most store-bought probiotics don’t help.
Non-Medication Treatments That Work
Medication isn’t the only path. Some of the most effective tools don’t come in a pill bottle.
Low-FODMAP diet: This isn’t a fad. It’s a three-phase process: eliminate, reintroduce, personalize. Done right-with a dietitian-it works for 70% of people. You don’t stay on it forever. You learn which foods trigger you.
Gut-directed hypnotherapy: Sounds strange, but it’s backed by science. In clinical trials, 40-60% of people saw major symptom improvement. It retrains how your brain responds to gut signals.
Cognitive behavioral therapy (CBT): Helps manage stress, anxiety, and the fear of flare-ups. It doesn’t change your gut-it changes how you react to it.
Exercise: Regular movement-walking, yoga, swimming-improves gut motility and reduces stress. Even 30 minutes a day makes a difference.

What About the Future?
Research is moving fast. Scientists are now mapping the gut microbiome to find specific bacterial patterns linked to IBS-D versus IBS-C. A new drug called ibodutant, targeting nerve receptors in the gut, showed 45% symptom improvement in early trials-nearly double placebo. Fecal microbiota transplants (FMT), once used for C. diff, are being tested for IBS. One study found 35% of patients went into remission after FMT, compared to just 15% in the control group.
But the biggest takeaway? No single treatment works for everyone. The most successful plans combine diet, stress management, and targeted meds. It’s personalized medicine at its most practical.
Real-Life Impact
IBS doesn’t just hurt your stomach-it hurts your life. A 2022 survey of over 1,200 IBS patients found that nearly 7 out of 10 missed work or school because of symptoms. On average, they lost 13 days a year. People on Reddit talk about canceling trips, avoiding social events, or hiding in the bathroom during meetings.
But there’s hope. In the same survey, 62% said dietary changes improved their symptoms. After six months on the right treatment plan, 55% said they felt "much better" or "very much better."
You’re not broken. You’re not imagining it. And you’re not alone. With the right tools, IBS can go from ruling your life to just being a part of it.
Can IBS turn into Crohn’s disease or colon cancer?
No. IBS is a functional disorder, not an inflammatory or structural disease. It doesn’t cause damage to the intestines, increase cancer risk, or progress into Crohn’s or ulcerative colitis. However, symptoms can overlap, which is why doctors rule out those conditions before diagnosing IBS-especially if you have red flags like weight loss, bleeding, or a family history.
How long does it take for IBS medication to work?
It varies. Over-the-counter meds like loperamide work within hours. Prescription drugs like linaclotide or eluxadoline usually show results in 2-4 weeks. Low-dose antidepressants take longer-often 4 to 8 weeks at full dose-because they work on nerve signaling, not just bowel movement. Don’t give up if you don’t see results right away.
Is the low-FODMAP diet safe long-term?
It’s not meant to be permanent. The elimination phase lasts 2-6 weeks. Then you slowly reintroduce foods to find your triggers. Staying on a strict low-FODMAP diet too long can reduce good gut bacteria and lead to nutrient gaps. Always work with a dietitian to personalize your plan and avoid unnecessary restrictions.
Can stress cause IBS, or just make it worse?
Stress doesn’t cause IBS, but it can trigger it in people who are genetically or biologically predisposed. Many people report their first major flare after a traumatic event, major life change, or prolonged stress. Once IBS is established, stress makes symptoms worse by amplifying gut-brain signals. Managing stress isn’t optional-it’s part of treatment.
Are there any natural remedies that help IBS?
Some show promise, but evidence is mixed. Peppermint oil capsules (enteric-coated) can relax gut muscles and reduce pain in about 40% of users. Ginger may help with nausea and bloating. Fiber supplements like psyllium can ease constipation, but not diarrhea. Avoid unproven supplements like colostrum, aloe vera, or herbal blends-they’re not regulated and can make symptoms worse.
Next Steps: What to Do Now
If you think you have IBS, start with your doctor. Write down your symptoms: when they happen, what you ate, how stressed you felt, and how your stool looked. Bring this to your appointment.
If you’re already diagnosed, don’t accept constant discomfort. Try one change at a time: track your food with an app like FODMAP Tracker, start walking 20 minutes a day, or ask your doctor about a referral to a dietitian or therapist trained in gut-brain therapies.
IBS is complex, but it’s manageable. You don’t need to live in fear of your next meal or bathroom break. With the right combination of tools, you can take back control.

10 Comments
Norene Fulwiler
I spent years thinking I was just "sensitive" until I found out I had IBS-D. The low-FODMAP diet was a game-changer - not because it’s perfect, but because it gave me back my weekends. I used to cancel plans constantly. Now I can eat at a taco truck without panic. It’s not a cure, but it’s freedom.
Also, gut hypnotherapy? I was skeptical. But after 12 sessions, my stomach stopped screaming every time I walked into a crowded room. Worth every penny.
And yes, stress makes it worse. But so does pretending you’re fine when you’re not. You’re not weak for needing help.
William Chin
While I appreciate the clinical precision of this article, I must emphasize that the over-medicalization of IBS reflects a systemic failure in modern healthcare. The pharmaceutical industry profits from chronic symptom management rather than root-cause resolution. One cannot simply prescribe a pill for a disorder rooted in lifestyle, environmental toxicity, and the erosion of traditional dietary patterns. The low-FODMAP diet, while empirically validated, is merely a bandage on a bullet wound.
Furthermore, the emphasis on psychological interventions such as CBT and hypnotherapy suggests a troubling conflation of somatic and psychiatric domains - a dangerous precedent that risks pathologizing normal human stress responses. One must ask: are we treating the gut, or are we silencing the body’s legitimate cry for change?
Ada Maklagina
IBS is the worst roommate ever. No warning. No apology. Just chaos.
Harry Nguyen
Of course it’s all about diet and stress. Because nothing says "science" like blaming your gut on garlic and your boss. Meanwhile, the real issue is that people these days have zero discipline. Back in my day, we ate what we were given, didn’t whine about bloating, and didn’t need a 17-step app to figure out why our stomachs acted up.
And now we’re giving out prescriptions for antidepressants to treat constipation? Next they’ll be prescribing yoga for broken legs. This isn’t medicine. It’s wellness theater.
Also, probiotics? The only thing that works is a good old-fashioned enema. But I guess that’s too barbaric for the Instagram generation.
Katie Allan
Reading this felt like someone finally held up a mirror to my life. I’ve spent 15 years feeling like I was broken because I couldn’t eat a salad without a 3-hour bathroom emergency. But here’s the truth: IBS doesn’t make you weak. It makes you resilient.
What helped me most wasn’t the meds or even the diet - it was finding a community. People who get it. People who don’t tell you to "just relax."
You’re not alone. And you don’t have to live in fear. One small step at a time - a walk, a food journal, a therapist who gets the gut-brain connection - that’s how you rebuild your life. Not in a day. But day by day.
Deborah Jacobs
God, I love how this post doesn’t sugarcoat it. IBS is like having a tiny, grumpy gremlin living in your colon who only speaks in cramps and sudden urges. One minute you’re fine, next you’re sprinting to a gas station bathroom like your life depends on it - because, honestly, it kind of does.
I tried everything. Probiotics that did nothing. Fiber that turned me into a balloon. Then I found a dietitian who didn’t just hand me a list but actually listened. Turns out, I’m not allergic to onions - I’m allergic to *bad* onions. Like, the ones soaked in garlic butter at Olive Garden. Who knew?
And the antidepressants? Yeah, they’re weird. But taking 10mg of amitriptyline at night didn’t make me feel like a zombie - it made me feel like I could sleep without bracing for a gut earthquake. That’s worth it.
Also, IBS doesn’t care if you’re a CEO, a mom, or a 22-year-old who thinks they’re invincible. It shows up for everyone. And that’s the weirdly beautiful part - we’re all in this weird, stinky, messy club together.
James Moore
It is, of course, imperative - nay, non-negotiable - to recognize that the etiology of IBS, as presented herein, remains fundamentally incomplete, and that the reductionist paradigm of FODMAPs, while statistically significant in controlled trials, fails to account for the profound epigenetic, microbiotic, and neuro-immunological interplay that undergirds the entire spectrum of functional gastrointestinal disorders. One cannot, in good conscience, reduce a multi-system dysregulation - a condition wherein the enteric nervous system, the hypothalamic-pituitary-adrenal axis, and the gut microbiota are in perpetual, cascading discord - to a mere dietary protocol.
Moreover, the suggestion that stress "exacerbates" symptoms is a gross understatement. Stress is not a trigger - it is the architect. The gut is not malfunctioning - it is communicating. And we, as a society, have deafened ourselves with pharmaceutical noise and behavioral distractions, mistaking symptom suppression for healing.
Furthermore, the normalization of antidepressants at sub-therapeutic doses for IBS - while pragmatic - reflects a troubling capitulation to the pharmacological-industrial complex, which thrives on chronicity. We must ask: is the goal to manage IBS - or to ensure that IBS endures, so that the market for Linzess, Viberzi, and gut-directed hypnotherapy apps remains perpetually lucrative?
Let us not forget: the body does not lie. It screams. And we, in our arrogance, have mistaken its screams for noise.
Manish Shankar
This is one of the most balanced and well-researched explanations of IBS I have read in a long time. As a medical professional from India, I have seen many patients dismissed as "anxious" or "overreacting." The truth is far more complex, and this article captures it with both scientific rigor and human compassion.
One point I would add: in many cultures, including mine, dietary triggers are often tied to traditional foods - lentils, spices, dairy-based desserts - and patients are reluctant to give them up. A gentle, culturally sensitive approach from dietitians is crucial. The low-FODMAP diet must be adapted, not imposed.
Also, the role of gut-brain axis is deeply understood in Ayurveda, where stress and digestion are inseparable. Modern science is finally catching up. Thank you for this.
luke newton
You people are so weak. IBS? That’s what happens when you eat gluten-free muffins and cry about your feelings. My grandpa worked 12-hour shifts in a steel mill and ate beans for dinner every night. He never once missed a day because his stomach "felt weird."
Now you’re paying $200 for a hypnotherapist to tell you to breathe? Just toughen up. Stop treating your gut like a fragile doll. Eat real food. Stop being a baby.
And don’t even get me started on probiotics. You think a little pill is going to fix what your lazy lifestyle broke? Pathetic.
Ali Bradshaw
Hey - I see you. The one scrolling through this at 2 a.m. because you’re hunched over the toilet again.
You’re not broken. You’re not lazy. And you don’t need to be fixed - you just need the right tools.
Start small. One change. One day. Maybe it’s writing down what you ate before the crash. Maybe it’s walking around the block. Maybe it’s telling your partner, "I’m not fine, but I’m trying."
It’s not about being perfect. It’s about being persistent. And you’re already doing better than you think.
I’ve been there. You’re not alone.