Many people with sleep apnea don’t realize their position at night could be making their condition worse. If you wake up gasping, your partner says you snore loudly, or you feel exhausted even after a full night’s rest, the problem might not just be your airway-it could be how you’re lying down. Sleeping on your back, known as supine sleeping, is one of the most common triggers for obstructive sleep apnea (OSA). Switching to side sleeping can cut your breathing interruptions in half-or even more. This isn’t just a tip from a sleep coach. It’s backed by clinical data, sleep studies, and real-world results from thousands of patients.
Why Supine Sleeping Makes Sleep Apnea Worse
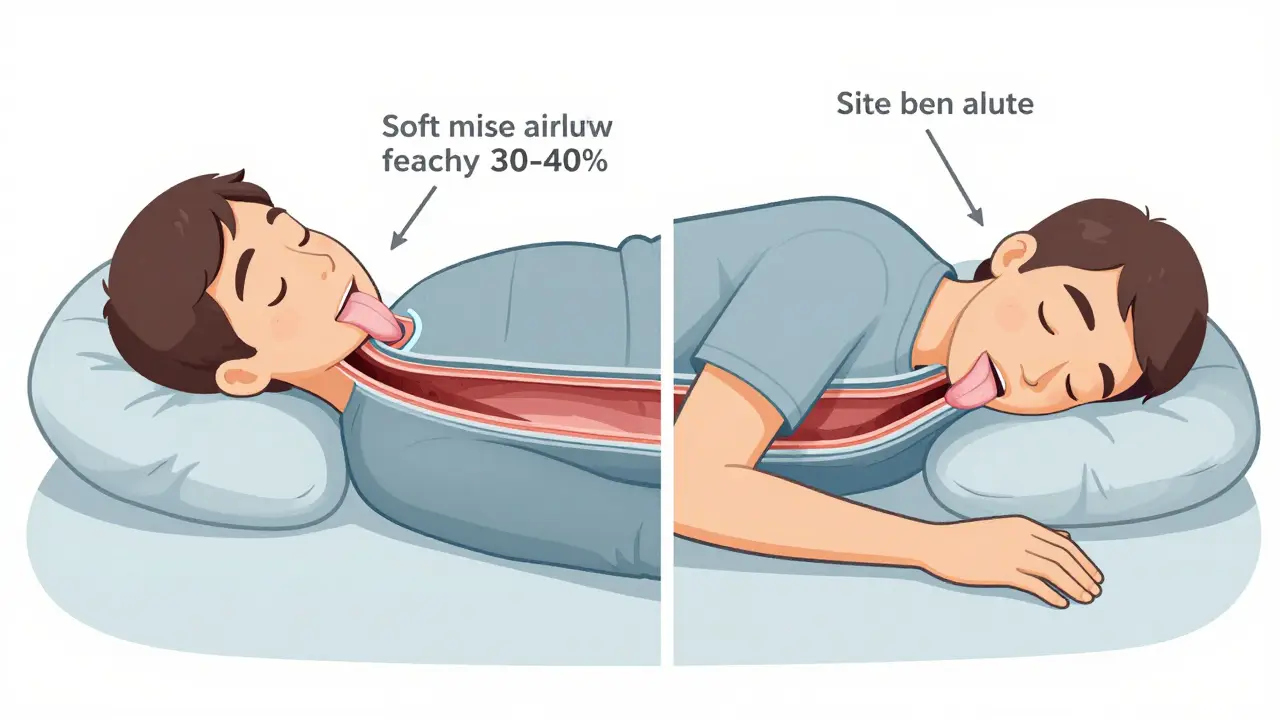
When you lie flat on your back, gravity pulls your tongue and soft tissues in your throat backward. This isn’t a minor inconvenience. Studies show this shift reduces the space in your upper airway by 30-40%. For someone with OSA, that small drop in space can turn a mild breathing issue into a full-blown obstruction. In fact, research from the Sleep Medicine Research journal (2023) found that for many patients, the number of breathing pauses per hour jumps from under 5 when sleeping on their side to over 30 when on their back. That’s not just snoring-it’s a serious drop in oxygen levels, repeated heart rate spikes, and frequent awakenings you may not even remember.It’s not just about frequency. The severity of each event worsens too. Apneas last longer, oxygen levels dip deeper, and the body’s stress response kicks in harder. This is why some people feel fine during the day but are diagnosed with severe OSA at night-because their sleep study only measured total events, not position-specific ones. A 2023 study by Eiseman et al. found that ignoring position data can lead to underestimating OSA severity by up to 30%. That’s why modern sleep labs now include positional analysis as part of the standard diagnostic process.
How Side Sleeping Helps
Sleeping on your side-whether left or right-keeps your airway more open. Without gravity pulling your tongue backward, the muscles in your throat stay in a more neutral position. The Sleep Foundation confirms side sleeping is the best position for OSA patients, and it’s not just anecdotal. Multiple studies show a consistent drop in the apnea-hypopnea index (AHI) when patients shift from supine to lateral positions. In one trial, patients with positional OSA saw their AHI drop from 28 to 6 after adopting side sleeping. For some, it was enough to move from severe to mild, or even normal, OSA.Side sleeping also reduces snoring. That’s because snoring happens when airflow vibrates loose tissues. With a more open airway, airflow becomes smoother. Many bed partners report that snoring stops almost instantly when the sleeper rolls onto their side. It’s not just about quiet nights-it’s about better sleep quality for both people in the bed.
What Is Positional Therapy?
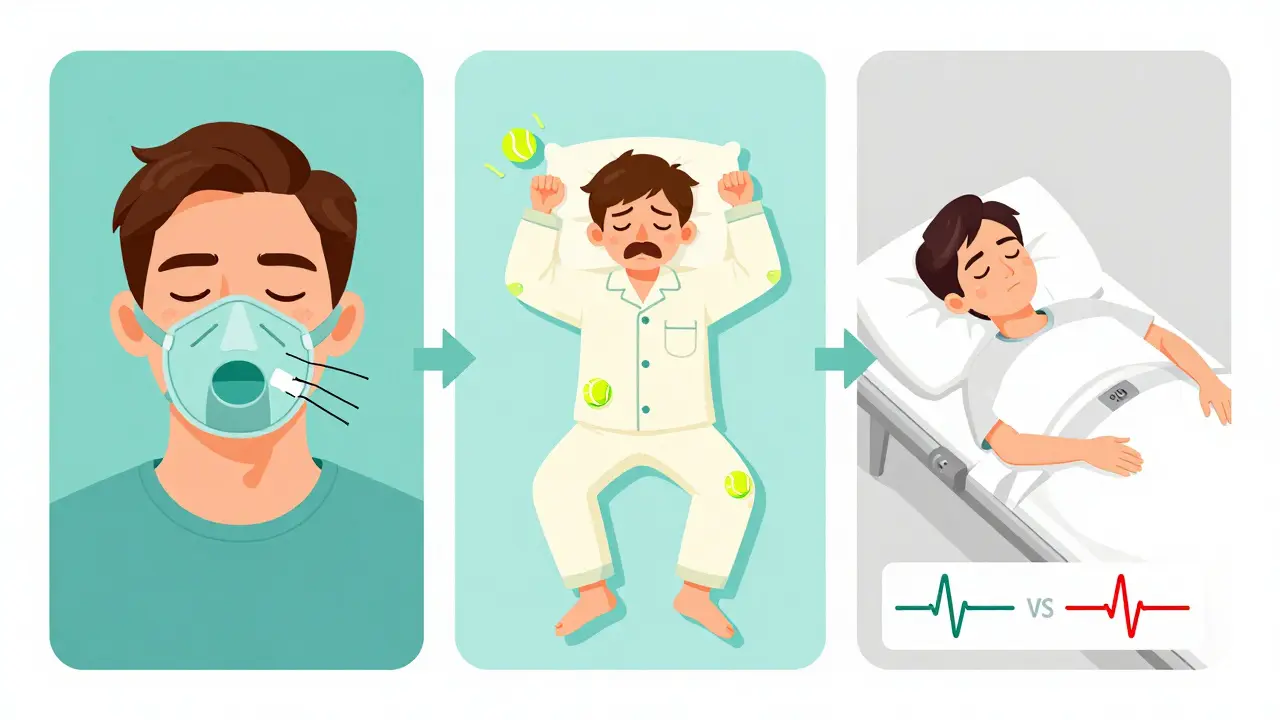
Positional therapy isn’t just about telling yourself to sleep on your side. It’s a structured approach to prevent you from rolling onto your back. The goal is simple: keep you in a lateral position all night, so your airway stays open without needing a machine or surgery.There are two main categories of positional therapy: low-tech and high-tech. The most well-known low-tech method is the tennis ball technique (TBT). You sew a tennis ball into the back of your pajamas or sleep shirt. If you roll onto your back, the ball digs into your spine, waking you up just enough to roll back over. It’s cheap, easy, and surprisingly effective for some. But it’s not comfortable. A 2023 survey from Sleep and Sinus Centers found that nearly 45% of users quit this method within three months because it disrupted their sleep too much.
High-tech solutions are designed to be less disruptive. The Sleep Position Trainer (SPT), like the NightBalance device, uses gentle vibrations when it detects you’re lying on your back. It doesn’t wake you fully-it nudges you. A 2015 study in the Journal of Clinical Sleep Medicine found that SPT users reduced their supine sleep time to a median of 0%, compared to 12.5% for TBT users. More importantly, 68% of SPT users reached treatment success (AHI under 5), while only 43% of TBT users did. SPT users also reported better quality of life scores and higher satisfaction ratings.

Positional Therapy vs. CPAP
Continuous Positive Airway Pressure (CPAP) is still the gold standard for treating OSA. It works by blowing air through a mask to keep your airway open. But here’s the catch: about half of people who start CPAP quit within a year. Why? The mask is uncomfortable, it leaks, it’s noisy, and it feels claustrophobic.Positional therapy doesn’t have those problems. The AAFP’s 2020 clinical review found that adherence to positional therapy is 35-40% higher than CPAP. That’s huge. A treatment that works 90% of the time but is only used 40% of the time is worse than a treatment that works 60% of the time but is used 90% of the time. For people with true positional OSA-where supine AHI is at least double the side AHI-positional therapy can be just as effective as CPAP, without the bulk, noise, or hassle.
That’s why major sleep organizations, including the American Academy of Sleep Medicine, now recommend positional therapy as a first-line treatment for mild to moderate positional OSA. It’s not a backup. It’s a primary option.
Who Is a Good Candidate?
Not everyone with sleep apnea benefits from positional therapy. You need to have positional OSA. That means your breathing problems are much worse when you’re on your back. How do you know? A sleep study must analyze your AHI by position. If your supine AHI is more than twice your non-supine AHI, you’re a candidate.For example: If your AHI is 8 when sleeping on your side and 24 when on your back, you have positional OSA. That’s a 3x difference. You’re a perfect fit. But if your AHI is 20 on your side and 22 on your back, positional therapy won’t help much. You need something stronger.
Also, positional therapy works best for mild to moderate OSA (AHI 5-30). For severe cases (AHI over 30), CPAP or other treatments are still recommended. But even in severe cases, if positional dependence is strong, combining positional therapy with a lower-pressure CPAP can improve comfort and adherence.
Devices on the Market
The market for positional therapy devices has grown fast. Here’s what’s available as of 2026:- DIY Solutions: Tennis ball technique, specialized wedge pillows ($20-$50). These are low-cost but often ineffective long-term.
- Wearable Vibration Devices: NightBalance, Smart Nora, and similar SPTs. These use sensors and gentle feedback. Cost: $300-$500. Most have mobile apps to track progress.
- Smart Bedding: Newer systems adjust your body position automatically using air cushions or gentle tilting. Still emerging, but promising for users who need hands-off solutions.
Market data shows adoption of advanced devices has grown 25% annually since 2020. Why? Better design, quieter feedback, and more proof they work. Insurance doesn’t cover them yet in most cases, but many patients find the cost worth it compared to years of failed CPAP use.
How to Start
If you suspect positional OSA, here’s what to do:- Get a sleep study that includes positional analysis. Ask your sleep doctor to review your AHI by position-not just total AHI.
- If your supine AHI is at least double your side AHI, you’re a candidate.
- Try the tennis ball technique for 1-2 weeks. If it works but is uncomfortable, consider upgrading to a vibration device.
- Combine positional therapy with head elevation. Raising your upper body by 30 degrees (using an adjustable bed or wedge pillow) helps keep your airway open even more.
- Track your progress. Use a sleep tracker or journal to note how many times you wake up, how you feel in the morning, and whether your partner notices less snoring.
Success isn’t overnight. It takes 2-4 weeks to train your body to stay on its side. But for many, the payoff is immediate: deeper sleep, fewer awakenings, and energy returning to your days.
What About Central Sleep Apnea?
Positional therapy is designed for obstructive sleep apnea, where the airway collapses. It’s less effective for central sleep apnea (CSA), where the brain doesn’t send the right signal to breathe. That said, some CSA patients still benefit from side sleeping. Research suggests it may improve lung volume and breathing signal stability. But if you have CSA, don’t rely on positional therapy alone. Talk to your sleep specialist about other treatments like adaptive servo-ventilation (ASV) or oxygen therapy.The Bigger Picture
Sleep apnea isn’t just about snoring. It’s linked to heart disease, stroke, high blood pressure, and type 2 diabetes. Every breathing pause stresses your cardiovascular system. Positional therapy doesn’t just improve sleep-it may reduce long-term health risks. Early data from 2023 suggests that reducing supine sleep time may lower nighttime blood pressure spikes and improve heart rate variability. But more studies are needed.For now, the evidence is clear: if you have positional OSA, sleeping on your side isn’t just a comfort tip-it’s medical treatment. And it’s one of the few therapies that works better the more you use it.
Can sleeping on my back cause sleep apnea?
No, sleeping on your back doesn’t cause sleep apnea. But if you already have it, supine sleeping makes it much worse. Gravity pulls your tongue and soft tissues backward, narrowing your airway and increasing the number and severity of breathing pauses. For people with positional OSA, this can turn mild symptoms into severe ones.
Is side sleeping better than CPAP for sleep apnea?
It depends. CPAP is more effective at reducing overall breathing events. But positional therapy has far better adherence. For patients with clear positional OSA-where apnea events are mostly when lying on the back-positional therapy can reduce AHI to normal levels. Many people who can’t tolerate CPAP find positional therapy a life-changing alternative. It’s not a replacement for everyone, but for the right person, it’s just as effective.
How do I know if I have positional sleep apnea?
You need a sleep study that breaks down your apnea-hypopnea index (AHI) by position. If your AHI while sleeping on your back is at least double your AHI while sleeping on your side, you have positional OSA. Many sleep labs now include this analysis automatically, but you should ask your doctor to review the positional data specifically.
Do positional therapy devices really work?
Yes, if you have positional OSA. A 2015 study in the Journal of Clinical Sleep Medicine showed that wearable vibration devices (like NightBalance) reduced supine sleep time to 0% in most users and achieved treatment success (AHI < 5) in 68% of cases. Compliance was over 30% higher than with the tennis ball technique. These devices work by gently nudging you to roll onto your side-not waking you, just guiding you.
Can I just use a pillow to stay on my side?
Body pillows or wedge pillows can help, but they’re not reliable. Most people still roll onto their back during deep sleep. These pillows work best as a supplement-not a standalone solution. For real results, you need active feedback, like vibration or physical discomfort, to prevent supine positioning. That’s why devices with sensors and feedback outperform passive aids.