Cancer Medication Safety: What You Need to Know About Risks, Interactions, and Safe Use
When you're taking cancer medication, drugs designed to kill fast-growing cells, including both cancerous and healthy ones. Also known as chemotherapy, these treatments are powerful but come with serious risks if not managed carefully. Cancer medication safety isn’t about avoiding side effects entirely—it’s about recognizing the warning signs before they become emergencies.
Many cancer drugs, like chemotherapy, strong drugs that target rapidly dividing cells, can weaken your immune system, cause dangerous bleeding, or crash your blood pressure when mixed with other meds. For example, taking a blood thinner like apixaban with certain cancer drugs can turn a minor bruise into a life-threatening bleed. Or mixing a PDE5 inhibitor like Cialis with nitroglycerin—common for heart issues—can cause your blood pressure to drop so fast you pass out. These aren’t hypothetical risks. They show up in real patients every day.
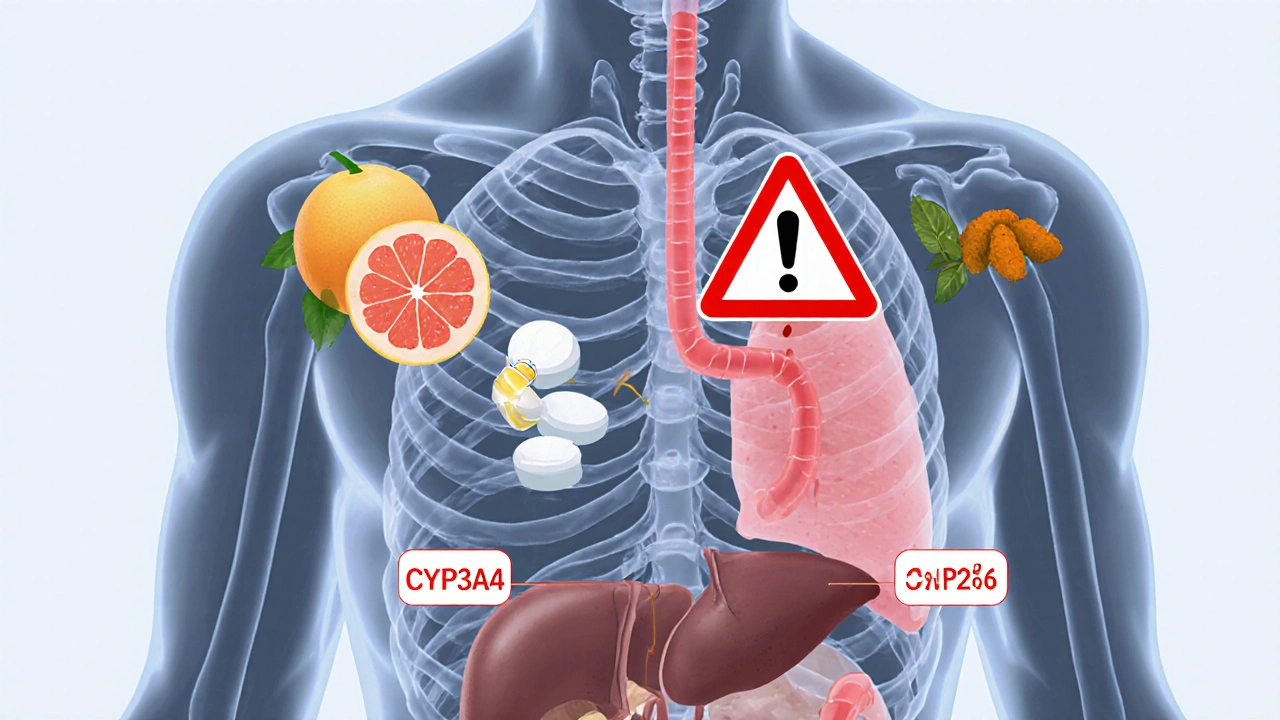
Drug interactions, when two or more medications change how each other works in your body are one of the biggest hidden dangers in cancer care. A common painkiller like ibuprofen might seem harmless, but it can make your kidneys struggle when you’re on cisplatin. Even something as simple as grapefruit juice can stop your body from breaking down certain chemo drugs, making side effects worse. And don’t assume generics are always safe swaps—bioequivalence studies prove most work the same, but some cancer meds need exact formulations to stay effective.
Safe use means knowing your meds inside out. Are you on a steroid like prednisone? Then watch for swelling, mood swings, or sudden infections. Taking a diuretic like furosemide? Keep track of how often you pee and if you feel dizzy. These aren’t just side effects—they’re signals your body gives you when something’s off. Most patients don’t realize that stopping a cancer drug on their own because of a side effect is often more dangerous than the side effect itself.
There’s no one-size-fits-all answer. What’s safe for someone with breast cancer might be deadly for someone with leukemia. Your treatment plan depends on the type of cancer, your other health issues, and even what other meds you take for high blood pressure or diabetes. That’s why checking in with your oncology team isn’t optional—it’s your lifeline.
Below, you’ll find real-world guides on what to watch for, how to spot dangerous interactions, and how to manage side effects without panicking. These aren’t theory pages—they’re from people who’ve been through it, and they tell you exactly what to do when things go wrong.