When you’re undergoing chemotherapy, every pill, supplement, or even bite of fruit can matter more than you think. It’s not just about the cancer drug working - it’s about making sure nothing else interferes with it. Drug interactions with chemotherapy aren’t rare. They’re common, dangerous, and often overlooked. About half of all outpatient cancer patients experience at least one potential drug interaction, and one in three of those could lead to serious harm - including hospitalization or death.
What Are Chemotherapy Drug Interactions?
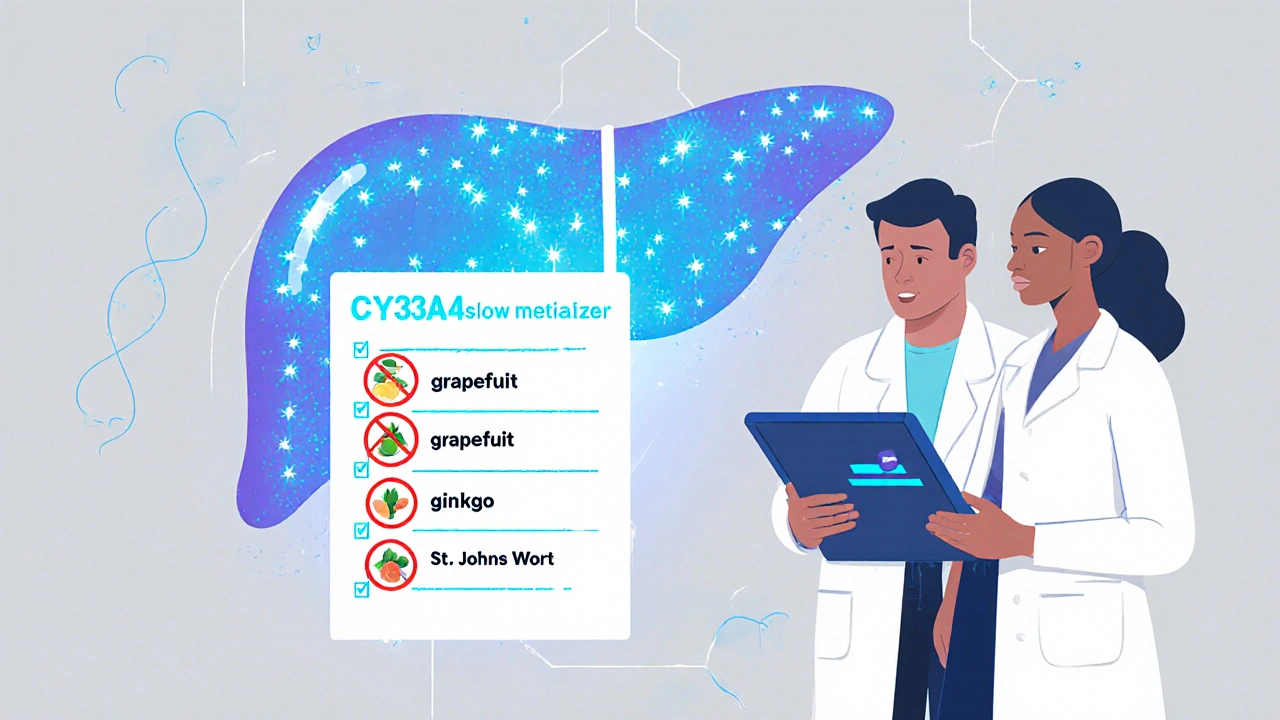
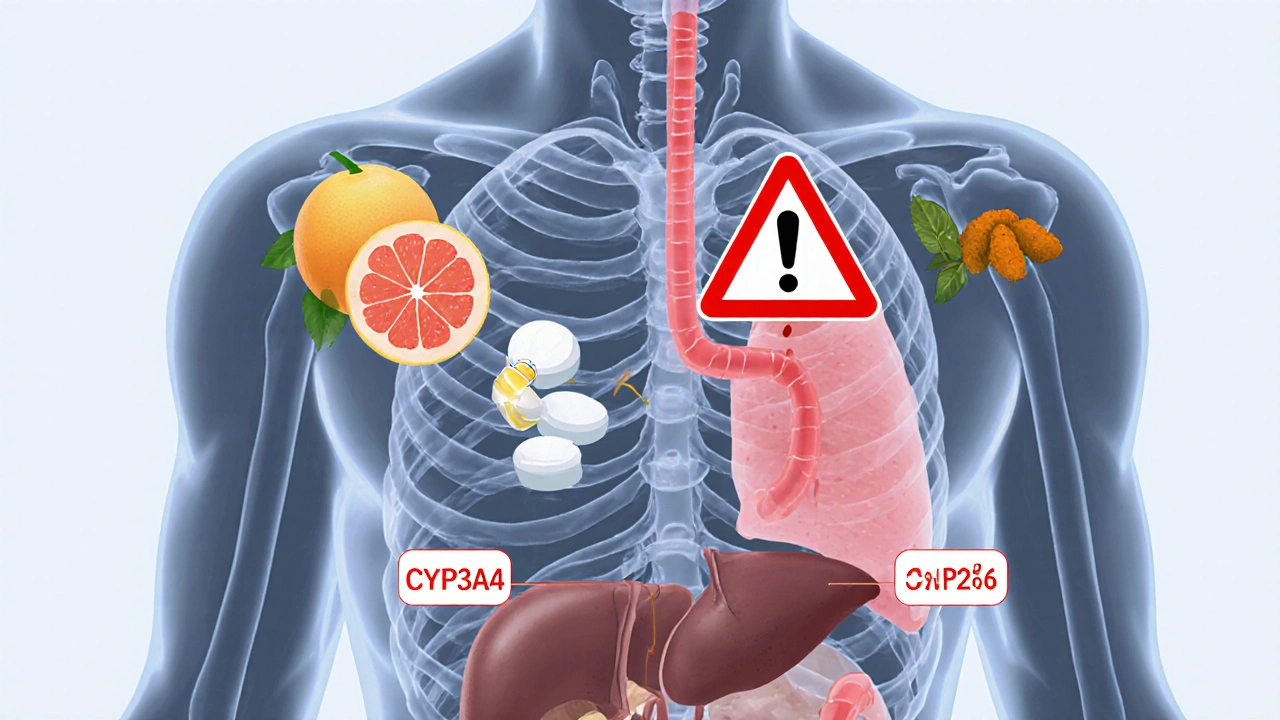
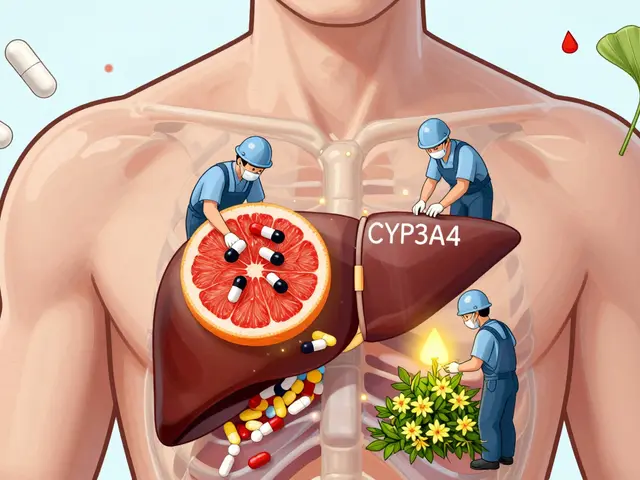
A drug interaction happens when one substance changes how another works in your body. With chemotherapy, this isn’t just about side effects adding up. It’s about your treatment losing power, becoming too toxic, or triggering entirely new dangers. There are three main types:- Pharmacokinetic: This is the most common. It’s about how your body absorbs, breaks down, or gets rid of the drug. Many chemotherapy drugs are processed by liver enzymes - especially the CYP3A4 system. If another drug or supplement blocks or speeds up these enzymes, your chemo levels can spike or crash.
- Pharmacodynamic: This is when two drugs affect the same part of your body, making their effects stronger or weaker. For example, combining two drugs that harm your kidneys can lead to kidney failure faster than either drug alone.
- Immunological: A newer and less understood type. Immune checkpoint inhibitors (like pembrolizumab or nivolumab) can change how your immune system reacts to other medications, sometimes causing severe skin reactions, liver damage, or even life-threatening inflammation.
Top Culprits: What You Must Avoid
Some interactions are well-known. Others catch even doctors off guard. Here’s what you need to watch out for:1. Grapefruit and Seville Oranges
Grapefruit juice isn’t just a breakfast staple - it’s a silent threat. It contains compounds called furanocoumarins that permanently disable the CYP3A4 enzyme in your gut. That enzyme breaks down many oral chemo drugs, including capecitabine, erlotinib, and sunitinib. If you drink grapefruit juice while taking these, your chemo levels can rise dangerously high - increasing side effects like nausea, low blood counts, or liver damage. One glass can affect you for days. Seville oranges (used in marmalade) do the same thing. Even grapefruit-flavored candies or supplements can trigger this.2. Herbal Supplements and Vitamins
People think ‘natural’ means safe. It doesn’t. A 2014 study of elderly cancer patients found that 75% were taking supplements that could interact with their chemo. Common offenders include:- Ginkgo biloba, garlic, ginger, ginseng: Increase bleeding risk - dangerous if you’re on blood thinners or having surgery.
- Turmeric (curcumin): May interfere with drugs like cyclophosphamide and doxorubicin by altering how they’re metabolized.
- St. John’s Wort: Speeds up liver metabolism, making many chemo drugs less effective. It’s been linked to treatment failure in breast cancer patients.
- Vitamin E, fish oil, flaxseed oil: Can thin the blood and raise bleeding risk during chemo or radiation.
- Bilberry, black cohosh, dong quai: May affect hormone-sensitive cancers or interact with tamoxifen.
Supplements aren’t tested like drugs. Labels often lie. A 2023 review found that nearly 1 in 4 supplements contained unlisted ingredients - sometimes steroids or stimulants. That’s why your oncologist needs to know everything you’re taking.
3. Over-the-Counter Pain Relievers
Ibuprofen, naproxen, and other NSAIDs seem harmless. But when combined with certain chemo drugs - especially those that affect the kidneys or blood - they can cause sudden kidney failure or dangerous bleeding. Acetaminophen (Tylenol) is usually safer, but even that can overload the liver if you’re on multiple drugs that stress it. Always check with your care team before taking any OTC painkiller.4. Antidepressants and Tamoxifen
About 1 in 8 women in the U.S. will get breast cancer. About 1 in 8 Americans take antidepressants. That’s a dangerous overlap. Tamoxifen, a common breast cancer drug, relies on the CYP2D6 enzyme to become active. Many antidepressants - like paroxetine (Paxil) and fluoxetine (Prozac) - block that enzyme. If you’re on tamoxifen and take one of these SSRIs, your cancer treatment becomes much less effective. Studies show this can raise the risk of recurrence. Your doctor needs to know your mental health history - and your medication list - to pick a safe antidepressant.Why Older Patients Are at Higher Risk
If you’re over 65, your risk of dangerous interactions jumps. Why? Your liver and kidneys don’t work as well. Your body holds onto drugs longer. You’re also more likely to be taking five or more medications - a condition called polypharmacy. One study of 244 cancer patients over 70 found that 75% had potential for serious drug interactions. That’s not a small number. It’s the norm.Age isn’t the only factor. If you have diabetes, heart disease, or kidney problems, your body handles drugs differently. Genetic differences also matter. Some people naturally have slower or faster versions of liver enzymes. That’s why two people on the same chemo can have completely different reactions to the same supplement.

Oral Chemo: The New Frontier of Risk
Twenty-five percent of chemotherapy drugs now come as pills - not IV bags. That’s a big shift. Oral chemo means you’re taking it at home, every day, often for months. It also means more chances for interactions - with food, supplements, even other prescriptions you pick up at the pharmacy.Unlike IV chemo, which is given in a controlled setting, oral chemo is easy to forget, skip, or accidentally double-dose. And if you take it with grapefruit juice or St. John’s Wort, you might not even know something’s wrong until it’s too late. That’s why pharmacists are now essential members of cancer care teams. They screen for interactions before you even leave the clinic.
How to Protect Yourself
You don’t have to live in fear. You just need to be smart. Here’s how:- Make a complete list. Write down every medication, supplement, vitamin, herb, and even over-the-counter product you take - including doses and how often. Don’t leave anything out. Not even the “tiny” ones.
- Bring it to every appointment. Give it to your oncologist, pharmacist, and nurse. Update it every time something changes.
- Ask before you take anything new. Even a new pain reliever, cold medicine, or probiotic. Say: “Is this safe with my chemo?”
- Avoid grapefruit and Seville oranges entirely. No juice, no fruit, no flavoring. It’s not worth the risk.
- Stop supplements before surgery. Most doctors recommend stopping anything that affects bleeding - like fish oil, garlic, or ginkgo - at least 10 days before any procedure.
- Use trusted resources. Ask your pharmacy if they use tools like Lexicomp or Micromedex - these have oncology-specific interaction checkers.
What Your Care Team Should Be Doing
You shouldn’t have to remember everything. Your team should be on guard for you. Here’s what good care looks like:- Pharmacists screen your entire medication list before you start chemo.
- Doctors document all supplements and OTC drugs in your chart - not just prescriptions.
- You get a written list of what to avoid, with clear explanations.
- For immunotherapy patients, your team checks for new interaction risks - like liver inflammation from combined medications.
- Every treatment cycle includes a quick review: “Any new pills, herbs, or foods?”
If your team doesn’t do this, ask why. Drug interactions are preventable. They shouldn’t be an afterthought.
The Future: Personalized Safety
The next big step isn’t just avoiding bad interactions - it’s predicting them before they happen. Researchers are now using genetic testing to see how your body processes drugs. Are you a slow metabolizer of CYP3A4? That changes your chemo dose. Do you carry a gene variant that makes you extra sensitive to certain supplements? That changes your advice.Some hospitals are already testing these approaches. In the future, your cancer treatment plan might include a “drug interaction profile” - just like your blood type. It’ll tell your doctors exactly what to avoid, based on your genes, your liver function, and your current meds.
For now, the best tool you have is communication. Be honest. Be detailed. Be persistent. Your life depends on it.
Can I take vitamins while on chemotherapy?
Some vitamins are safe, but many can interfere with chemotherapy. High-dose antioxidants like vitamin C, E, or selenium may protect cancer cells from chemo damage, making treatment less effective. Others, like vitamin K, can affect blood thinners. Always talk to your oncology team before taking any supplement - even a daily multivitamin.
Does grapefruit affect all chemotherapy drugs?
No, but it affects many common ones - especially oral drugs like capecitabine, erlotinib, sunitinib, and pazopanib. It works by blocking the CYP3A4 enzyme, which breaks down these drugs. If your chemo is given intravenously, the risk is lower, but not zero. Since it’s hard to know which drugs are affected, the safest rule is to avoid grapefruit entirely during treatment.
Are herbal teas safe during chemotherapy?
Many herbal teas are risky. Green tea can interfere with bortezomib. Chamomile and peppermint may affect liver enzymes. Licorice root can raise blood pressure and lower potassium - dangerous if you’re on certain chemo drugs. Even ‘mild’ teas can interact. Stick to plain water, decaffeinated black or green tea (in moderation), and ask your pharmacist before drinking anything herbal.
Can I take ibuprofen for a headache during chemo?
It depends. Ibuprofen and other NSAIDs can increase bleeding risk and harm your kidneys - especially if you’re on chemo drugs like cisplatin or carboplatin. Acetaminophen (Tylenol) is usually the safer choice for pain or fever. But even Tylenol can be risky if you have liver problems or are on multiple liver-metabolized drugs. Always check with your care team before taking any pain reliever.
Why do some cancer drugs interact with antidepressants?
Some cancer drugs, like tamoxifen, need to be converted by liver enzymes to work. Certain antidepressants - especially paroxetine and fluoxetine - block those same enzymes. That means the cancer drug doesn’t activate properly, reducing its effectiveness. For breast cancer patients, this can mean a higher chance of the cancer coming back. Your doctor can choose an antidepressant that won’t interfere, like venlafaxine or citalopram.
Should I stop supplements before starting immunotherapy?
Yes - especially immune-boosting ones like echinacea, astragalus, or high-dose vitamin D. Immunotherapy already activates your immune system. Adding supplements can trigger severe inflammation in your lungs, liver, or skin. Even common ones like turmeric or fish oil can increase side effects. Your oncologist should review all supplements before you start immunotherapy and may ask you to stop them for weeks before and during treatment.
What to Do If You Think You’ve Had an Interaction
If you notice sudden nausea, unusual bruising, severe fatigue, skin rash, or yellowing of your skin or eyes - don’t wait. Call your oncology team immediately. These could be signs of a drug interaction. Keep a symptom diary: what you took, when, and what happened. This helps your team figure out what caused it.Don’t assume it’s just “chemo side effects.” Interactions can mimic them - but they’re often more sudden and more dangerous. If you’re unsure, it’s better to call and get it checked.

9 Comments
Joe Durham
I never realized how many everyday things could mess with chemo. I thought grapefruit was just bad for statins, but learning it can tank your treatment? That’s wild. My aunt’s oncologist never mentioned it - she drank grapefruit juice daily for years. Glad I know now.
Also, the part about supplements being unregulated? Yeah, I’ve seen people on Facebook selling ‘miracle cancer cures’ made from ‘pure herbs.’ It’s terrifying how easy it is to get misled when you’re desperate.
Thanks for laying this out so clearly. I’m sharing this with my whole family.
Nick Lesieur
so like… if i eat a grapefruit and take chemo, i just… die? lol. jk. kinda. but seriously, why do doctors not just tell you this before you leave the clinic? like, is this on a ‘you figure it out’ checklist? 🤡
also, ‘natural’ doesn’t mean safe? who knew. next you’ll tell me breathing oxygen can be dangerous if you’re on certain meds.
Angela Gutschwager
St. John’s Wort = treatment failure. 💔
That’s it. That’s the tweet.
Andy Feltus
It’s funny how we treat medicine like a vending machine - insert pill, get cure. But the body isn’t a machine. It’s a living, breathing, enzyme-heavy ecosystem where one wrong nut in the gears can turn a lifesaver into a landmine.
Chemo isn’t just poison. It’s a precision instrument. And we hand it to people and say, ‘Go home, take this, and don’t forget to avoid grapefruit.’
Meanwhile, the system doesn’t even screen for supplements. That’s not negligence. That’s a structural failure. We’ve outsourced safety to the patient - and patients aren’t pharmacists. We’re just scared humans trying not to die.
Maybe the real question isn’t ‘what’s dangerous?’ - it’s ‘why aren’t we protecting people better?’
Dion Hetemi
Let me get this straight - you’re telling me that people are popping turmeric capsules like they’re M&Ms while getting chemo? And nobody’s stopping them?
Bro, I’ve seen people on Reddit bragging about their ‘anti-inflammatory smoothies’ while their loved ones are in hospice. This isn’t wellness. This is self-sabotage wrapped in a yoga mat.
And don’t even get me started on the ‘I’m taking vitamin C to boost my immune system’ crowd. You’re not boosting your immune system - you’re shielding cancer cells. Congrats, you just turned your chemo into a placebo.
Stop being a wellness influencer and start being a patient.
Kara Binning
I can’t believe this country lets people walk into a pharmacy and buy ‘immune boosters’ that could kill someone on chemo. This is why America is falling apart - no regulation, no accountability, just profit-driven nonsense.
My cousin died because her ‘natural healer’ told her to stop her meds and drink ‘cancer-fighting tea.’ She was 42.
Someone needs to sue every supplement company. Someone needs to jail the influencers. This isn’t healthcare - it’s a horror show.
river weiss
It is imperative that patients maintain a comprehensive, up-to-date, and accurately documented medication and supplement list. This list should include exact dosages, frequencies, and sources (e.g., brand name, manufacturer).
Pharmacists are underutilized resources in oncology care; they are trained to identify clinically significant drug-drug and drug-supplement interactions using validated databases such as Lexicomp, Micromedex, and Clinical Pharmacology.
Patients should request a formal medication reconciliation at every visit. If their oncology team does not initiate this, they should explicitly request it. Documentation should be shared with all providers involved in care.
Additionally, the use of oral chemotherapy demands even greater vigilance, as self-administration increases the risk of non-adherence and unintentional interactions. A daily pill organizer with a logbook is strongly recommended.
Finally, while genetic testing for CYP450 variants is not yet universal, patients should inquire whether such testing is available through their institution - especially if they have experienced unexplained toxicity or treatment failure in the past.
Brian Rono
Oh wow, grapefruit is bad? Shocking. Next you’ll tell me water is dangerous if you’re on lithium.
Let’s be real - if your chemo is so fragile that a grapefruit can ruin it, maybe the drug itself is poorly designed. Why not make a version that doesn’t rely on a single enzyme that’s easily blocked by breakfast? That’s not patient safety - that’s lazy pharmacology.
And let’s talk about ‘natural’ supplements. You know what’s natural? Snake venom. And yet we use it to make blood pressure meds. So ‘natural’ is just a marketing term for ‘unregulated and unproven.’
But hey, if you want to believe that turmeric is a cancer cure, go ahead. Just don’t blame the system when your treatment fails. You picked the placebo over the science.
Andrew Baggley
This is the kind of info that saves lives. Seriously. I was scared to even take a vitamin while on treatment - but now I know exactly what’s dangerous and what’s not.
My mom’s oncologist didn’t mention any of this until she got hospitalized from a bad interaction. Don’t wait for that. Print this out. Bring it to your next appointment.
You’re not being paranoid - you’re being smart. And if your doctor rolls their eyes? Find a new one. Your life isn’t a suggestion box.
Stay strong. Stay informed. You’ve got this.