Copper Accumulation: Causes, Risks, and What You Need to Know
When your body holds onto too much copper accumulation, the abnormal build-up of copper in tissues, especially the liver and brain. Also known as copper toxicity, it doesn’t happen from eating too many nuts or shellfish—it’s usually caused by genetic issues, liver disease, or long-term exposure to copper-rich environments. Most people absorb only what they need and flush out the rest. But when that system breaks down, copper starts sticking where it shouldn’t.
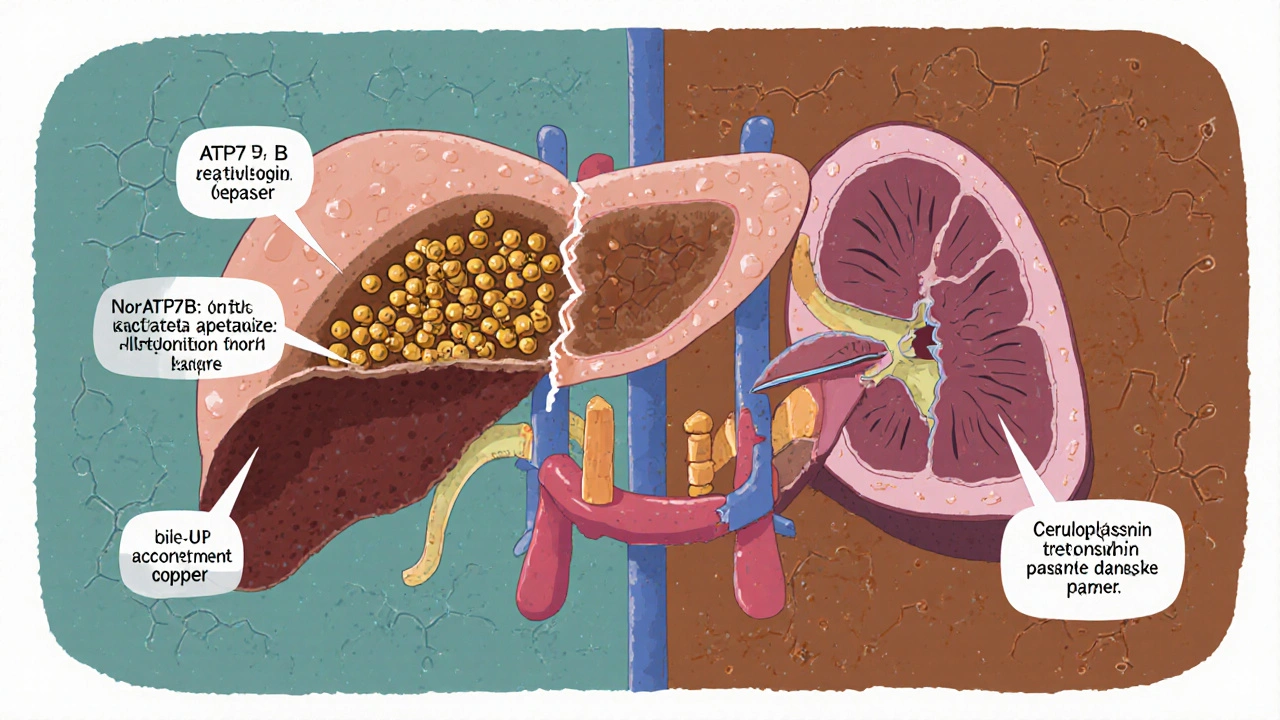
Wilson disease, a rare inherited disorder that prevents the liver from releasing copper into bile is the most common cause of dangerous copper buildup. People with Wilson disease start accumulating copper from childhood, and without treatment, it damages the liver, brain, and eyes. Liver damage, often the first sign of copper overload can look like hepatitis—fatigue, jaundice, belly pain—but it gets worse over time. In advanced cases, copper spills into the bloodstream and affects the brain, causing tremors, trouble speaking, or even psychiatric symptoms that mimic depression or schizophrenia.
Copper accumulation isn’t always genetic. Long-term use of copper IUDs, drinking water from old copper pipes, or working in metal refining can add up over decades. People with chronic liver disease—like cirrhosis from alcohol or hepatitis—often can’t process copper properly either. Even some supplements and multivitamins contain copper, and taking them daily without knowing your levels can tip the balance.
Doctors test for copper buildup with blood tests, urine tests, and sometimes a liver biopsy. An eye exam can spot the telltale Kayser-Fleischer ring—a brownish halo around the iris—that’s a classic sign of Wilson disease. The good news? If caught early, copper accumulation can be managed. Medications like penicillamine or zinc help your body get rid of the excess. Diet changes matter too—cutting back on organ meats, shellfish, nuts, and chocolate helps.
What you won’t find in most online guides is how often copper issues are missed. Symptoms show up slowly, and many doctors don’t think to test for it unless someone is young and has unexplained liver or neurological problems. That’s why awareness matters. If you’ve been told your liver enzymes are high for no clear reason, or if you have a family history of liver disease or unexplained neurological symptoms, ask about copper.
Below, you’ll find real-world guides on how copper interacts with medications, how it affects liver health, and what conditions are linked to metal imbalances. These aren’t theory pieces—they’re practical, patient-tested insights from people who’ve dealt with this firsthand.