Medication Risk Assessment Tool
Your Medication Profile
Risk Assessment
Your Medication Risk Score
Recommended Actions
Keep a detailed medication list and review with your doctor regularly.
When you take a new medication, your doctor doesn’t just look at your current symptoms. They’re also reading your past. Your medical history isn’t just a record-it’s a warning system. It tells them which drugs might hurt you, not help you. And the stakes are higher than most people realize. In the UK alone, over 200,000 hospital admissions each year are linked to preventable adverse drug reactions. A lot of those could have been avoided-if the full story of your health had been properly understood.
Why Your Past Medications Matter More Than You Think
It’s not enough to say you’ve taken a drug before. What matters is what happened when you took it. If you had a rash, dizziness, or nausea after taking penicillin ten years ago, that’s not just a memory. It’s a red flag. Studies show patients with a history of adverse reactions to one drug class are 30-40% more likely to react to another drug in the same family. That means if you had a bad reaction to amoxicillin, you’re at higher risk for a reaction to cefalexin-even if they’re different names. Cross-reactivity isn’t rare. It’s predictable. And it’s often missed.
That’s why pharmacists and doctors are trained to ask: “What happened the last time you took this?” Not just “Have you ever taken this?” The difference is life-changing. One wrong assumption can send someone to the ER.
Polypharmacy: The Silent Killer in Your Medicine Cabinet
Taking five or more medications at once isn’t uncommon, especially as you age. But it’s dangerous. According to the British Heart Foundation, people on five to nine drugs are twice as likely to have a bad reaction. Those on ten or more? Their risk triples. Each extra pill adds 7-10% more chance of something going wrong.
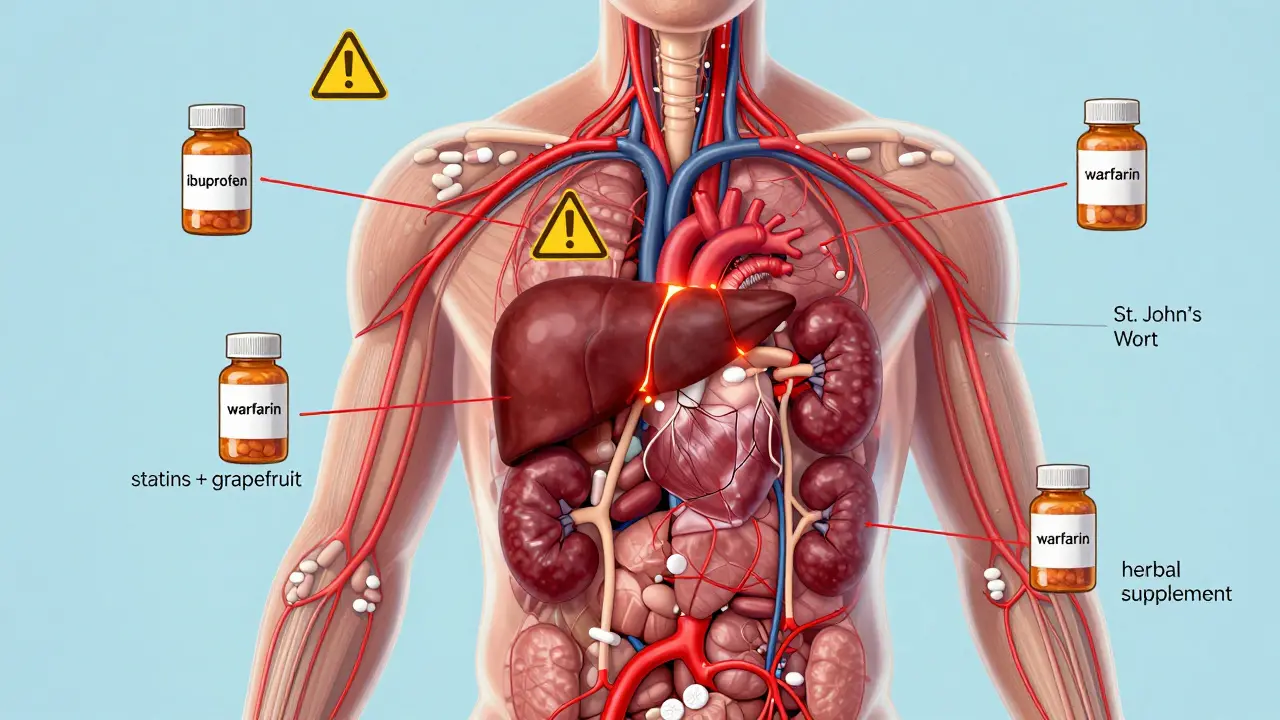
Why? Because drugs don’t just work on their own. They talk to each other. Warfarin and ibuprofen? Together, they can cause dangerous bleeding. Statins and grapefruit juice? That combo can fry your liver. And if your doctor doesn’t know you’re taking all of them-or if you forgot to mention the herbal supplement you started last month-the system doesn’t catch it.
Worse, electronic health records only flag 35% of these risks properly. That means in nearly two out of three cases, the computer doesn’t even warn the doctor. You’re left relying on human memory. And memory is flawed. Especially when you’re juggling eight prescriptions, two inhalers, and a handful of vitamins.
Your Organs Are Talking-Are You Listening?
Your kidneys and liver don’t just filter toxins. They filter your medicines. And if they’re not working right, drugs build up in your body like traffic on a highway with no exits.
Chronic kidney disease? That cuts your body’s ability to clear drugs by 50-75%. For common medications like metformin or certain antibiotics, that means even a normal dose can become toxic. Yet a 2021 audit found that 45% of prescriptions for older adults didn’t adjust for kidney function-even though 15% of adults over 60 have reduced kidney function.
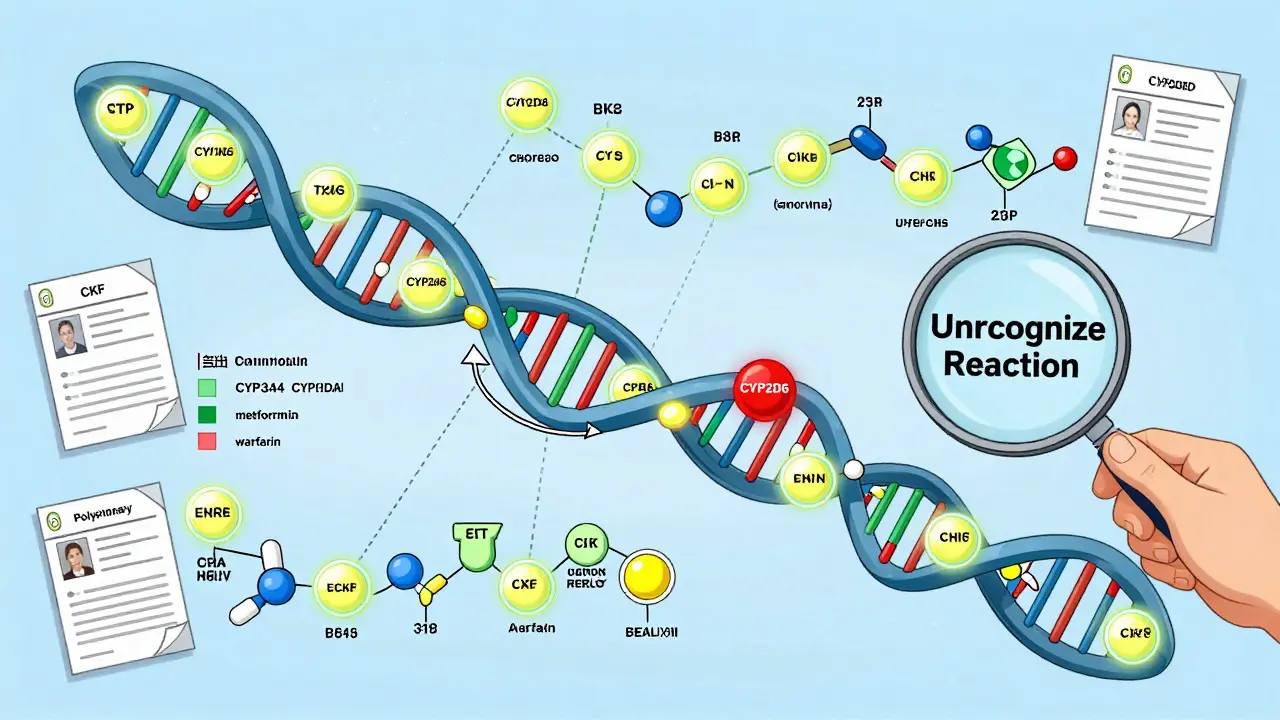
Liver problems? Same story. If your liver can’t break down drugs properly, levels in your blood can spike by 30% to 500%. That’s not a typo. Some people with genetic variations in liver enzymes (CYP450 system) process drugs so slowly that a standard dose becomes an overdose. And most doctors don’t test for this. They assume everyone metabolizes drugs the same way.

Age Isn’t Just a Number-It’s a Risk Factor
People over 65 are 3 to 5 times more likely to have a bad reaction to medication than younger adults. Why? Because aging changes how your body handles drugs. Your kidneys slow down. Your liver shrinks. Your body holds onto fat differently. Your brain becomes more sensitive to sedatives.
That’s why a sleeping pill that’s fine for a 40-year-old can leave an 80-year-old confused, dizzy, and falling. And falls in older adults? One in three leads to hospitalization. And many of those falls are caused by medication side effects that were never anticipated.
Here’s the kicker: older women are hit even harder. They experience ADRs at least 50% more often than men. Why? Because most drug trials until recently were done mostly on men. Between 2010 and 2020, women made up only 22% of participants in heart drug studies. So the doses were calibrated for male bodies. Women metabolize drugs differently. Their body weight, hormone levels, and fat distribution all change how drugs act. And we’re still paying the price.
Chronic Conditions Multiply the Risk
Having one chronic disease? Risk goes up. Having three or more? Risk explodes. The data is clear: patients with multiple conditions have 2.6 times higher odds of a medication error. Why? Because each condition adds another layer of complexity.
Diabetes? You’re on insulin, metformin, maybe a statin. Heart disease? Add beta-blockers, aspirin, ACE inhibitors. Arthritis? NSAIDs. Depression? Antidepressants. All these drugs interact. And they mask symptoms. Beta-blockers can hide the fast heartbeat of a bleeding ulcer. Steroids can dull the pain of a ruptured appendix. If your doctor doesn’t know your full history, they might think you’re getting worse from your disease-not from your meds.
The Charlson Comorbidity Index is a tool doctors use to measure this risk. It scores conditions like heart failure, liver disease, and cancer to predict how likely you are to have a bad reaction. The higher the score, the more careful you need to be. Yet most patients never even hear about it.
What You’re Not Telling Your Doctor Could Kill You
It’s not just about what’s in your chart. It’s about what’s missing.
One in four patients skip doses because they can’t afford their meds. Then they restart them later without telling anyone. That’s a recipe for disaster. Studies show this pattern increases side effects by 28%. Your body forgets how to handle the drug after a break. The dose that was safe before now feels too strong.
And then there’s the herbal stuff. Turmeric. Ginseng. St. John’s Wort. People think these are “natural,” so they’re safe. But St. John’s Wort can make birth control fail. Turmeric can thin your blood like aspirin. And if you’re on warfarin? That’s a dangerous mix. Yet most patients don’t mention these to their doctors-because they don’t think it counts.
PatientsLikeMe, a health forum with over a million users, found that 62% of people with multiple chronic conditions had side effects their doctors didn’t recognize as drug-related. Why? Because the history wasn’t connected. The doctor saw the dizziness. Didn’t see the new blood pressure pill. Didn’t see the herbal tea. Didn’t see the missed doses last month.
What You Can Do Right Now
You don’t need to be a doctor to protect yourself. Here’s what works:
- Keep a real-time list of every pill, patch, injection, and supplement you take. Include dosage and when you take it. Update it every time something changes.
- Bring that list to every appointment-even if you think it’s the same doctor. Don’t assume they remember.
- Ask: “Could this be causing my symptoms?” If you’re feeling off, say it outright. Don’t wait for them to ask.
- Request a medication review every year if you’re on five or more drugs. This is called deprescribing. It cuts side effects by 22%. Yet only 18% of eligible patients get it.
- Ask about genetic testing if you’ve had unexplained reactions. Tests like YouScript look at 27 genes that affect how you process drugs. They’re not perfect, but they’re getting better. And they can prevent serious harm.
There’s no magic bullet. But knowledge is power. And your medical history? That’s your most powerful tool.
What’s Next? The Future Is Personalized
Pharmacogenomics-the science of how your genes affect your response to drugs-isn’t science fiction anymore. The FDA approved platforms like YouScript in 2023 that can predict how you’ll react to 27 different drugs based on your DNA. Early results show a 34% drop in side effects for people who use it.
But here’s the problem: only 5.7% of U.S. healthcare systems use it. In the UK, it’s even lower. Cost, lack of training, and slow adoption are holding it back.
Still, the writing is on the wall. In five years, your genetic profile may be part of your medical record-just like your blood type. Until then, the best thing you can do is make sure your history is complete, accurate, and loud.
Because the next time you take a pill, it’s not just the drug that matters. It’s your past. Your body. Your story. And if you don’t tell it, someone else might get it wrong.
Can my medical history really cause me to react badly to a drug I’ve taken before?
Yes. Even if you took a drug safely in the past, changes in your health-like kidney decline, liver damage, or starting new medications-can make your body respond differently. A dose that was safe last year might be toxic now. Also, if you had a reaction to one drug in a class (like penicillin), you’re at higher risk for reactions to similar ones (like cephalosporins).
Why do older adults have more side effects from medications?
As we age, our kidneys and liver don’t work as well, so drugs stay in our system longer. We also have less muscle and more fat, which changes how drugs are absorbed and stored. Plus, older adults often take multiple medications, which increases the chance of dangerous interactions. Studies show people over 65 have 3-5 times more adverse reactions than younger adults.
Is it safe to stop a medication if I think it’s causing side effects?
Never stop a prescribed medication on your own. Some drugs, like blood pressure or antidepressant medications, can cause dangerous withdrawal symptoms if stopped suddenly. Instead, write down your symptoms and bring them to your doctor. They can help you taper off safely or switch to a better option.
How can I make sure my doctor knows all the medications I’m taking?
Keep a written or digital list updated with every pill, patch, injection, and supplement-including over-the-counter drugs and herbal remedies. Bring it to every appointment. Don’t assume your doctor remembers or can access your full history. Many electronic systems miss key details. Your list is your best defense.
What’s the most common mistake people make with their medication history?
The biggest mistake is leaving out supplements, vitamins, and herbal products. People think these aren’t “real” medicine, but they can interact just like prescription drugs. St. John’s Wort, for example, can make birth control fail or reduce the effect of antidepressants. Always include everything.






12 Comments
Jenci Spradlin
man i had this crazy reaction to amoxicillin back in 2018-hives, swelling, the whole deal. thought it was just a one-off till my pharmacist pulled up my file and said 'yo, you’re 3x more likely to react to cephalosporins now.' scared the shit outta me. now i keep a printed list in my wallet. never trust memory.
Gregory Clayton
oh here we go again with the medical fear porn. your body isn't a fragile snowflake. people took penicillin in the 50s with no records, no apps, no 'medication reviews'-and they lived. stop treating every pill like a grenade. you're just making people paranoid.
Aron Veldhuizen
What you're describing isn't medical history-it's a narrative of vulnerability constructed by a system that profits from fear. The real issue isn't that we don't know our past; it's that we've outsourced our bodily autonomy to algorithms and overworked physicians who don't have time to listen. Your 'warning system' is a liability management tool disguised as care. The data you cite? It's not about safety-it's about liability avoidance. And yet, we're told to be grateful.
Micheal Murdoch
Let me tell you something real: your body remembers everything. That rash you had ten years ago? It’s still in your cells. The liver enzyme that barely worked then? It’s still sluggish. You don’t need a fancy genetic test to know this-you just need to pay attention. I’ve seen people on eight meds who swear they’re fine until they stop one and realize their brain fog lifted. That’s not coincidence. That’s biology whispering. Most of us just ignore the whispers till they scream.
And yeah, supplements matter. I had a friend who took turmeric for 'inflammation' and ended up in the ER because she was on warfarin. She didn’t think it counted. Turns out, 'natural' doesn’t mean 'harmless.'
Keep a list. Talk to your pharmacist. Ask 'what if this isn’t helping?'-not just 'is this working?' That shift changes everything. You’re not just a patient. You’re the only one who lives in your body every day. Listen to it.
Jeffrey Hu
Actually, the 30-40% cross-reactivity stat is misleading. That’s based on IgE-mediated allergies, which only apply to a subset of reactions. Most adverse drug reactions are type B-idiosyncratic, unpredictable, and not cross-reactive. You’re conflating hypersensitivity with metabolic interactions. Also, YouScript’s 34% reduction? That’s in a controlled cohort. Real-world adherence is under 40%. And the CYP450 testing? Only relevant for 12% of commonly prescribed drugs. Most of this is overhyped by pharma-adjacent influencers.
RAJAT KD
My uncle died from a bleeding ulcer caused by ibuprofen and aspirin combo. Doctor never asked about OTC meds. Never. He was 72. Took 7 pills. Didn't know grapefruit juice was in his smoothie. This isn't theory. It's family history.
Matthew Maxwell
It’s appalling how many people treat their health like a casual hobby. You wouldn’t drive a car without checking the oil. Why do you treat your body like a disposable appliance? The fact that people still think herbal supplements are 'safe' because they’re 'natural' is a sign of societal collapse. If you’re not taking responsibility for your own health, you’re not just endangering yourself-you’re burdening everyone else.
Jacob Paterson
Oh wow, so now we need a DNA test before we can take Tylenol? Next you’ll be asking for a background check on my liver. Look, I’ve been on 5 meds for 15 years. I’ve never had a problem. Maybe the problem isn’t the drugs-it’s the people who turn every pill into a horror movie.
Johanna Baxter
i just started a new antidepressant and now i feel like i’m floating in a vat of molasses. my doctor says it’s 'normal adjustment' but i’ve been on this for 6 weeks and i’m crying in the shower again. i didn’t tell him about the ashwagandha i’ve been taking because i thought it was 'just chill vibes.' now i’m scared to even drink coffee. why does no one warn you about this stuff before you start?
Patty Walters
same. i took St. John’s Wort for anxiety and didn’t realize it killed my birth control. ended up pregnant at 40 when i swore i was done. now i keep a google doc with every pill, dose, and date. even the gummy vitamins. my dr actually thanked me for it last visit. small win.
Phil Kemling
What if the real tragedy isn’t the adverse reactions-but the fact that we’ve normalized the idea that our bodies are broken machines needing constant correction? We treat medication like a cure-all, not a temporary bridge. We don’t ask: why do I need this many drugs? Why is my body this fragile? Maybe the system isn’t broken. Maybe it’s designed to keep us dependent. Your history isn’t just a warning. It’s a mirror.
Micheal Murdoch
And that’s why I always say: don’t just track your meds. Track how you feel. Write it down. Not just 'headache'-write 'headache after 3pm, worse when I eat gluten, better after walking.' That’s the real data. That’s what turns a doctor from a prescriber into a partner. Your body talks. You just have to learn its language.