Before you write a prescription, you need to know if the drug is covered-and how much the patient will actually pay. It’s not just about what’s clinically right. It’s about what’s covered, what requires prior authorization, and whether the patient can afford it. If you skip this step, you risk delayed treatment, patient non-adherence, or even an emergency visit because they couldn’t fill the script.
What Exactly Is a Formulary?
A formulary, also called a Preferred Drug List (PDL), is the official list of medications covered by a patient’s health plan. It’s not random. Every drug on it has been reviewed by a committee of doctors and pharmacists who look at safety, effectiveness, and cost. These lists are updated regularly-sometimes monthly-because new drugs hit the market, generics become available, or prices change. Medicare Part D plans, for example, must follow strict federal rules. They use a five-tier system:- Tier 1: Preferred generics-usually $1 to $5 per prescription
- Tier 2: Other generics-slightly higher cost
- Tier 3: Preferred brand-name drugs-clinically proven, but more expensive
- Tier 4: Non-preferred brands-often $50 or more per script
- Tier 5: Specialty drugs-costing over $950/month, paid as a percentage (coinsurance)
How to Find the Right Formulary
You can’t guess. You have to look it up-for each patient, each time. Start with the insurer’s website. Most have a drug search tool. For Aetna, you enter the patient’s county and plan name. For UnitedHealthcare, you pick the plan type (Medicare, Commercial, etc.) and search by drug name. You’ll see the tier, any restrictions (like prior authorization), and sometimes even estimated out-of-pocket costs. If the website is slow or confusing, download the full PDF formulary. Many insurers, like Excellus BCBS, offer downloadable PDFs that list every drug and its status. Bookmark the direct link to the current year’s formulary. Medicare plans for 2024 are effective January 1, 2024, through December 31, 2024-but they can change mid-year with 60 days’ notice. For Medicaid patients, it’s state-specific. Minnesota, for example, has a single PDL for all Medicaid members. California has a different one. You need to know which state’s program the patient is enrolled in. And don’t forget the CMS Plan Finder tool. It covers 99.8% of Medicare Part D plans. You can search by drug, zip code, and plan type. It’s free, official, and updated daily.Understanding the Codes: PA, ST, QL
Don’t just look at the tier. Look at the codes next to the drug:- PA (Prior Authorization): You must submit paperwork before the plan will approve the drug. This can take 24-72 hours. For cancer drugs, delays over 48 hours happen in 32% of cases.
- ST (Step Therapy): The patient must try and fail on a cheaper drug first. Example: You want to prescribe a new diabetes drug, but the plan requires the patient to try metformin first-even if they’ve already tried it and it didn’t work.
- QL (Quantity Limit): The plan limits how much you can prescribe in a month. Example: Only 30 tablets of a painkiller per 30 days, even if the patient needs more.
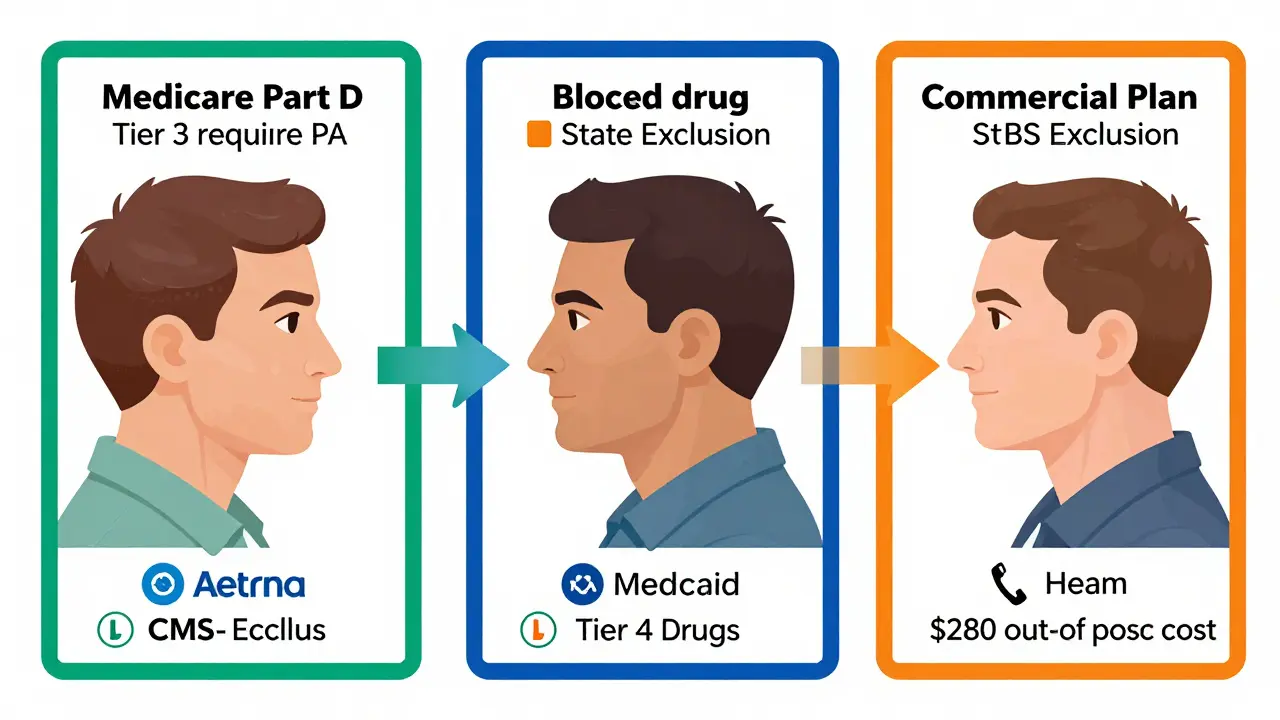
Medicare vs. Medicaid vs. Commercial Plans
Not all formularies are built the same. Medicare Part D plans are standardized across the country. They must cover at least two drugs per therapeutic class and offer exceptions. They use the five-tier model. They’re required to respond to prior authorization requests in 72 hours (24 for urgent cases). Medicaid programs are run by states. 42 states use closed formularies-meaning if a drug isn’t on the list, it’s blocked unless you get an exception. That’s harder than it sounds. The process can take days or weeks. Commercial plans (like those from UnitedHealthcare or Aetna for employer coverage) are all over the map. Some use four tiers. Others have six. Some don’t even publish their formularies publicly. You might need to call the provider line. The bottom line: you can’t use the same checklist for every patient. A drug that’s Tier 1 in one plan might be Tier 4-or not covered at all-in another.How to Save Time: Tools That Actually Work
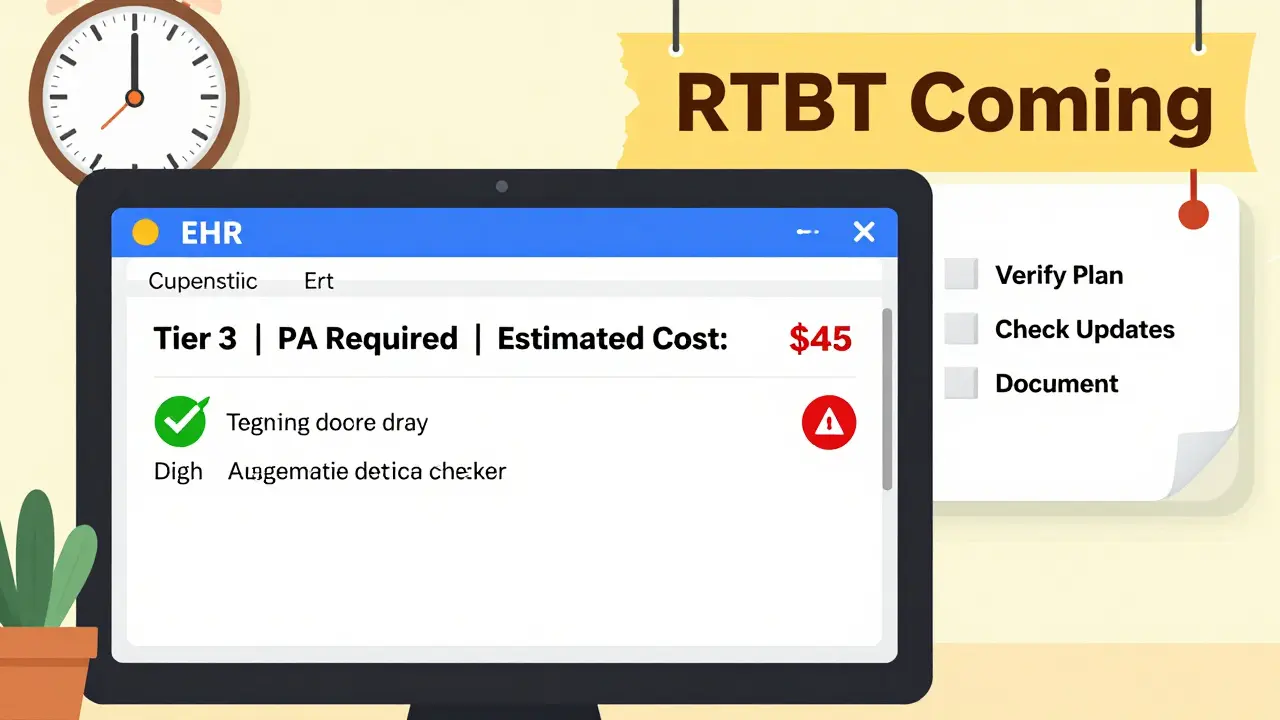
Checking formularies manually for every patient takes time. A 2023 Sermo survey found primary care physicians spend nearly 19 minutes per patient just verifying coverage. The good news? There are tools that cut that time in half. EHR-integrated formulary checkers are the most effective. Northwestern Medicine reduced prescription abandonment by 42% after adding Epic’s Formulary Check module. It shows tier level, PA requirements, and cost estimates right in the prescription screen. If the drug isn’t covered, it suggests alternatives. Real-time benefit tools (RTBT) are coming fast. By January 1, 2026, Medicare Part D plans must integrate RTBT into EHRs. That means when you click “prescribe,” the system will pull live data from the patient’s plan-cost, tier, restrictions-all in seconds. If your clinic doesn’t have this yet, use these workarounds:- Bookmark the top 5 insurer formulary pages you use most
- Set calendar reminders for quarterly updates (HealthPartners, for example, updates in January, April, July, October)
- Keep a printed copy of your most common formularies in your exam room
- Use the insurer’s 24/7 provider hotline-98% of Medicare plans offer this
What Happens When You Don’t Check
I’ve seen it too many times. A patient comes in with a new script. They’re excited. They leave the office thinking they’re getting a great new drug. Then they get to the pharmacy and are told, “It’s not covered.” Or, “You need to try something else first.” Or, “That’s $280 out of pocket.” They don’t fill it. They don’t call back. They stop taking their meds. Their blood pressure spikes. Their diabetes gets worse. A few months later, they’re back in the ER. This isn’t rare. A 2024 study showed that 28% of Medicare beneficiaries experience formulary changes mid-year. Patients get confused. Providers get blamed. The fix? Make formulary checks part of your routine-like checking allergies.What’s Changing in 2025 and Beyond
The Inflation Reduction Act’s $2,000 annual cap on out-of-pocket drug costs for Medicare starts in 2025. That’s forcing insurers to shift drugs to lower tiers. More generics. Fewer specialty drugs in Tier 5. More drugs in Tier 1. AI tools are also entering the space. Epic’s FormularyAI, launched in August 2024, predicts coverage likelihood with 87% accuracy by analyzing 10 million past prior authorization decisions. It doesn’t replace you-it helps you decide faster. But challenges remain. Therapeutic interchange programs (where pharmacists swap a prescribed drug for a cheaper one on the formulary) are growing. Some say it saves money. Others say it undermines patient trust. There’s no national standard yet.Final Checklist Before Prescribing
Before you hit “submit,” run through this:- Confirm the patient’s exact insurance plan (Medicare Part D? Medicaid? Employer plan?)
- Search the insurer’s official formulary website or use CMS Plan Finder
- Check the tier level-this tells you the cost
- Look for PA, ST, or QL codes-these are red flags
- Verify the formulary is current (effective Jan 1-Dec 31, 2024, unless updated)
- If unsure, call the insurer’s provider line-don’t guess
- Document your check in the patient’s chart: “Formulary verified per Aetna 2024 PDL, Tier 3, no restrictions”
Do all insurance plans use the same formulary?
No. Each insurer creates its own formulary based on negotiations, clinical guidelines, and cost. Medicare Part D plans follow federal rules but vary by company. Medicaid formularies are state-specific. Commercial plans vary even more. Always check the patient’s exact plan.
What does PA, ST, and QL mean on a formulary?
PA means Prior Authorization-you must get approval before the plan covers the drug. ST means Step Therapy-the patient must try a cheaper drug first. QL means Quantity Limit-the plan only covers a certain amount per month. These restrictions can delay treatment, so always check them before prescribing.
How often are formularies updated?
Most insurers update formularies quarterly-January, April, July, and October. Medicare Part D plans must give 60 days’ notice before removing or restricting a drug. Some plans update monthly. Always verify you’re using the current version.
Can I prescribe a drug not on the formulary?
Yes, but the patient will likely pay full price unless you get an exception. Medicare and Medicaid require formal prior authorization requests for non-formulary drugs. The process can take days. In emergencies, some plans allow expedited requests with a 24-hour turnaround.
Is there a free tool to check Medicare formularies?
Yes. The Centers for Medicare & Medicaid Services (CMS) offers the Plan Finder tool at Medicare.gov. It covers 99.8% of Medicare Part D plans and lets you search by drug name, zip code, and plan type. It’s free, official, and updated daily.
Why do some drugs cost so much more on Tier 4?
Tier 4 drugs are non-preferred brand-name medications. Insurers put them there because they’re more expensive and have cheaper alternatives on lower tiers. Patients pay a higher coinsurance-often 30-50%-instead of a flat copay. The goal is to encourage use of lower-cost options that work just as well.
How can I reduce formulary-related delays in my practice?
Use EHR-integrated formulary checkers like Epic’s Formulary Check. Bookmark your most-used insurer links. Set reminders for quarterly updates. Train your staff to verify coverage during check-in. And always document your checks. This cuts down on last-minute surprises at the pharmacy.







14 Comments
Michael Burgess
Man, I wish I had this guide when I started. I once prescribed a $300/month drug only to find out the patient’s plan didn’t cover it-and they had to choose between rent and insulin. Now I check formularies before I even open the chart. It’s not extra work-it’s basic care.
And yeah, RTBT is coming in 2026. Thank God. I’m tired of playing phone tag with insurance reps at 4:55 PM on a Friday.
Pro tip: Bookmark the CMS Plan Finder. It’s the only thing that doesn’t make you want to scream into a pillow.
Also-why do some insurers still use PDFs from 2021? That’s not a formulary. That’s a museum exhibit.
veronica guillen giles
Oh sweet mercy. So you’re telling me we’re still forcing doctors to be insurance clerks? How about we just make drugs affordable instead of turning every prescription into a scavenger hunt?
Also, ‘prior authorization’ is just corporate gaslighting dressed up as bureaucracy. ‘Sorry, your diabetic patient needs the drug that works-but first, prove they’re suffering enough.’
Meanwhile, the CEO of Aetna bought a third yacht last quarter. Just sayin’.
Ian Ring
Thank you for this comprehensive, deeply necessary overview. I’ve been practicing for 17 years, and I still find myself stunned by the sheer absurdity of formulary complexity.
It’s not just inefficient-it’s ethically corrosive. We’re trained to heal, yet forced to navigate labyrinthine, profit-driven gatekeeping systems.
And yes, the RTBT integration by 2026? Long overdue. But let’s not pretend tech will fix the root problem: healthcare as a commodity.
Still-this checklist? Print it. Laminate it. Tape it to your monitor. 🙏
Tru Vista
Formularies are a mess. Tier 5 drugs are just $$$ traps. PA = paperwork prison. ST = step therapy = stupid. QL = quantity limit = why even prescribe?
Also, Epic’s FormularyAI? 87% accurate? Lol. I’ve seen it suggest generics that are contraindicated. Don’t trust bots. Check manually. Always. #YMMV
JUNE OHM
They don’t want you to know this… but the real reason they make formularies so confusing? So you’ll prescribe the drugs they’re paid to push. Big Pharma owns these plans. The ‘committee reviews’? Just PR theater. They don’t care about outcomes-they care about stock prices.
And now they’re using AI to hide it better? 😒
Wake up, people. This isn’t healthcare. It’s a casino. 🎰💊
Philip Leth
As a med student from the Midwest, I just wanna say: this post saved my butt. I was about to prescribe a drug that had a PA and a QL and I didn’t even know what those letters meant.
Now I have a sticky note on my laptop that says ‘CHECK BEFORE YOU CLICK.’
Also, the CMS Plan Finder? Absolute legend. Free. Official. No ads. Rare in this world.
Thanks for keeping it real, doc.
Liam Tanner
There’s a quiet epidemic here: patients who stop meds because they can’t afford them-and then get blamed for ‘non-compliance.’
We’re not just prescribing pills. We’re prescribing access. And if the system blocks access, we’re complicit.
Check the formulary. Document it. Advocate. It’s part of the job now. No shame in that.
Palesa Makuru
How quaint. You treat this like it’s a professional inconvenience. In my clinic, we have patients who drive 90 miles just to get a $5 generic because their local pharmacy won’t fill it without PA-and their Medicaid plan changed the formulary last Tuesday without telling anyone.
You think this is about ‘best practices’? No. It’s about who gets to live and who gets to suffer quietly.
And you’re still using PDFs? How 2012.
Hank Pannell
There’s a philosophical layer here that no one talks about: if prescribing a drug requires navigating a corporate labyrinth, are we still practicing medicine-or acting as administrative intermediaries for a market-driven system?
The formulary isn’t just a list-it’s a moral code written by actuaries, not physicians.
And yet we’re the ones held accountable when patients don’t get better.
Is this healing? Or is this compliance theater dressed in white coats?
Lori Jackson
It’s not just formularies. It’s the entire structure. Why should a patient’s access to life-saving medication depend on whether their employer chose UnitedHealthcare over Kaiser? This isn’t healthcare-it’s a lottery.
And you call it ‘professional responsibility’ to check tiers? No. It’s a scandal. A moral failure. And you’re all just complicit by following the rules.
Stop normalizing this. Start protesting it.
Wren Hamley
Biggest win? When you prescribe a Tier 1 generic and the patient says, ‘I didn’t know I could get this for $3.’ That moment? Pure gold.
Also, I just found out my clinic’s ‘2024 formulary’ was actually from 2022. No one updated it. We’ve been prescribing based on ghosts.
So yeah. Check. Then check again. Then check with a coworker. Then call the insurer. Then cry a little. Then do it again tomorrow.
Sarah Little
Just a note: if you’re using the CMS Plan Finder, make sure you’re using the patient’s exact zip code. One digit off and you get a different plan. Happened to me last week. Prescribed a drug that was covered… for someone in the next county. Oops.
Also, don’t trust the ‘estimated cost’-it’s often wrong. Call. Always call.
innocent massawe
Coming from Nigeria, I can’t believe how much effort goes into something so basic. Here, if you have the money, you get the drug. If not, you don’t. No tiers. No PA. No forms.
But I see your point-this system is designed to confuse, not to care.
Still, your checklist? Useful. I’ll share it with my med school friends. 🙏
erica yabut
Let’s be real: if you’re not using AI tools to predict coverage by now, you’re not just behind-you’re negligent. The fact that you’re still scrolling through PDFs like it’s 2010 is embarrassing.
And if you think step therapy is ‘standard practice,’ you’ve never met a patient who’s been on metformin for 12 years and still has an A1c of 11.
This isn’t medicine. It’s medieval.