When your liver is struggling, food isn’t just fuel-it’s medicine. Too many people think liver damage is irreversible, or that only drugs can fix it. But decades of research show something simpler, and more powerful: what you eat every day can reduce liver fat, lower inflammation, and even reverse early-stage disease. This isn’t about fasting, detox teas, or expensive supplements. It’s about a clear, science-backed way of eating that’s been proven to work in real people with real liver conditions.
What a Liver-Healthy Diet Actually Looks Like
There’s no single “liver diet” you need to follow. Instead, there’s one pattern that keeps showing up in study after study: the Mediterranean diet. It’s not a trend. It’s not a fad. It’s what people in countries like Greece and Italy have eaten for generations-and it’s now the gold standard recommended by the American Association for the Study of Liver Diseases (AASLD) and the Mayo Clinic. This eating pattern isn’t about cutting out entire food groups. It’s about shifting what’s on your plate. Half your plate should be vegetables and fruits-aim for at least three servings of veggies and two of fruit daily. Think leafy greens, broccoli, carrots, berries, apples, and oranges. These aren’t just low-calorie fillers. They’re packed with antioxidants and phytonutrients that directly reduce liver inflammation. For example, blueberries and purple grapes contain anthocyanins, which clinical trials show can cut liver inflammation by up to 25%. One-quarter of your plate should be lean protein: chicken, fish, tofu, legumes, or eggs. Stick to about 3 ounces per meal-that’s the size of a deck of cards. Protein helps repair liver tissue and prevents muscle loss, which is critical if you have advanced liver disease. Contrary to old myths, you don’t need to limit protein unless you have severe cirrhosis and confusion (hepatic encephalopathy). Even then, recent studies suggest too little protein can make things worse. The last quarter? Whole grains. Brown rice, quinoa, oats, barley, and whole-wheat bread. These give you fiber, which helps your body clear toxins and lowers blood sugar spikes that feed fat buildup in the liver. Avoid white bread, white rice, and refined pasta-they’re just sugar in disguise.What to Cut Out-For Good
Some foods don’t just lack benefit-they actively harm your liver. The biggest offender? Added sugar, especially in liquid form. A single 12-ounce soda contains 39 grams of sugar-about 150 calories from pure fructose. That sugar doesn’t go to your muscles or brain. It goes straight to your liver, where it’s turned into fat. This is the main driver behind non-alcoholic fatty liver disease (NAFLD), now called MASLD. Studies show that cutting out sugary drinks alone can reduce liver fat by 30% in just six months, even without losing weight. Trans fats are another silent killer. Found in fried foods, packaged snacks, and margarine, they increase bad cholesterol and trigger liver inflammation. Look for “partially hydrogenated oils” on ingredient lists-and avoid them completely. Sodium is also a problem, especially if you have cirrhosis. Too much salt leads to fluid retention, swelling, and higher blood pressure. Keep daily sodium under 2,000 mg. That means skipping processed soups, canned vegetables, deli meats, and salty snacks. Flavor food with herbs, garlic, lemon juice, or vinegar instead.Why the Mediterranean Diet Wins Over Other Trends
You’ve probably heard of keto, low-fat diets, or intermittent fasting for liver health. But here’s what the data says: - Low-fat diets often replace fat with sugar and refined carbs. That’s a recipe for more liver fat. A 2021 meta-analysis found the Mediterranean diet reduced liver fat 32% more than low-fat diets. - Keto diets can help with weight loss, but they’re high in saturated fats and low in fiber. Long-term, they may increase liver inflammation and raise cholesterol. One study showed they improved liver fat less than Mediterranean eating after 12 months. - Detox diets and juice cleanses have zero scientific backing. The American Liver Foundation says outright: “There is no such thing as a liver detox.” Your liver detoxifies itself-just give it the right tools. The Mediterranean diet works because it’s balanced. It’s rich in monounsaturated fats (like olive oil and avocados), which lower bad cholesterol and reduce fat buildup in the liver. It’s high in fiber, which stabilizes blood sugar. And it’s full of anti-inflammatory compounds from plants, nuts, and fish. Plus, it’s good for your heart. The PREDIMED trial showed it cuts heart disease risk by 30%. That’s important-because people with fatty liver disease are far more likely to die from heart problems than liver failure.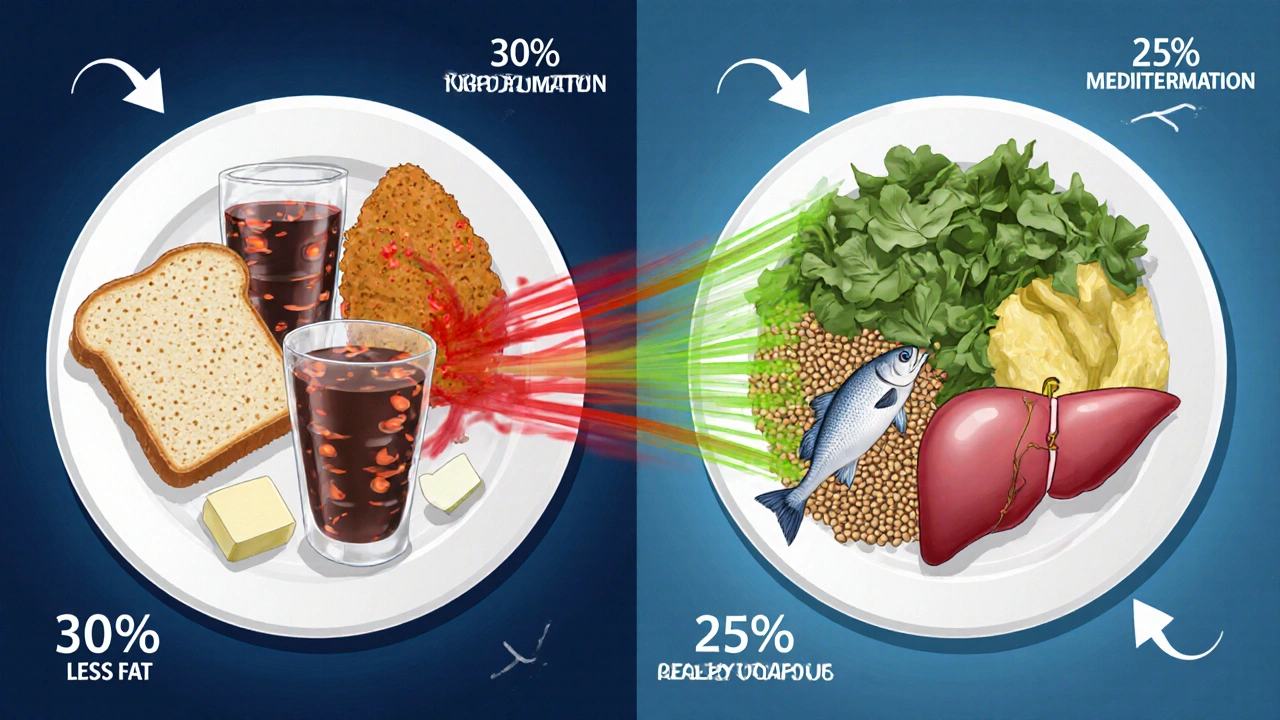
Real People, Real Results
John, a 58-year-old from Ohio, was diagnosed with stage 2 liver fibrosis. His FibroScan reading was 12.5 kPa (a sign of scarring), and his ALT liver enzyme was 112 U/L (normal is under 40). He started eating a Mediterranean-style diet-more veggies, no soda, olive oil instead of butter, and walking 30 minutes daily. After nine months, his FibroScan dropped to 6.2 kPa. His ALT fell to 45. He didn’t take a single pill. On Reddit’s r/FattyLiver community, 68% of over 1,200 people reported better energy within three months of changing their diet. But 42% said it was hard because healthy food felt more expensive. That’s true-meals can cost about $1.50 more per serving. But there are ways around it. Use frozen vegetables-they’re just as nutritious, cheaper, and last longer. Buy beans and lentils in bulk. Cook in batches on Sundays. Swap out one meal a day at first, then build up. One user said, “I started with just one Mediterranean dinner a week. Now I eat like that every day.”Practical Tips to Get Started
You don’t need to overhaul your life overnight. Start small:- Replace soda with sparkling water and lemon.
- Swap white rice for brown rice or quinoa.
- Use olive oil instead of butter or margarine.
- Have a handful of walnuts (30g) as a snack-they’ve been shown to lower LDL cholesterol by 15% in NAFLD patients.
- Include cruciferous veggies like broccoli, Brussels sprouts, or kale at least three times a week. They contain indole-3-carbinol, which reduces liver fat by up to 18% in six months.
What About Supplements and Special Diets?
Vitamin E has been studied for NAFLD and showed modest benefit in non-diabetic patients-but only at high doses (800 IU/day), and only under medical supervision. Don’t self-prescribe. Omega-3 supplements (fish oil) can help lower liver fat and triglycerides. But they’re not a substitute for real food. Eating fatty fish like salmon, mackerel, or sardines twice a week gives you the same benefit, plus protein and other nutrients. Coffee? Yes. Two to three cups a day (black or with a splash of milk) are linked to lower liver fibrosis and reduced cancer risk. It’s one of the few things that’s consistently protective. Avoid herbal “liver cleanses.” Milk thistle? Some studies show mild benefit, but nothing strong enough to recommend as treatment. And some supplements can actually harm the liver.When You Need More Support
If you’re struggling, you’re not alone. Only 12% of Americans meet the full Mediterranean diet criteria. That’s why programs like the VA Health System’s 12-week telehealth nutrition coaching have an 87% satisfaction rate. They teach you how to shop, cook, and plan meals on a budget. UnitedHealthcare now covers liver-specific nutrition counseling for over 2 million people in 12 states. Ask your doctor if you qualify. Many hospitals have dietitians who specialize in liver disease. If you work nights or have irregular hours, meal timing matters. Eating within a 10-hour window (like 8 a.m. to 6 p.m.) is being tested in a major new trial. Early results show it boosts fat loss from the liver beyond diet alone.It’s Not Just About the Liver
A liver-healthy diet doesn’t just fix your liver. It lowers your risk of type 2 diabetes, heart disease, stroke, and even some cancers. It gives you more energy, better sleep, and clearer thinking. It’s not a punishment. It’s a gift to your whole body. You don’t need to be perfect. Miss a meal? Have a slice of pizza? That’s okay. What matters is the pattern over weeks and months. The liver is one of the few organs that can regenerate-if you give it the chance. Start today. Swap one sugary drink for water. Add a serving of broccoli to dinner. Choose olive oil over butter. These small steps add up. And in six months, you might look back and realize: you didn’t just change your diet. You changed your future.Can a liver-healthy diet reverse fatty liver disease?
Yes, especially in early stages. Studies show that following a Mediterranean-style diet can reduce liver fat by 25-40% within 6-12 months, even without weight loss. In patients with non-alcoholic fatty liver disease (NAFLD), this often leads to improved liver enzyme levels and reduced fibrosis. The key is consistency-not perfection.
Is the keto diet good for liver health?
Keto may help with short-term weight loss, but it’s not ideal for long-term liver health. Many keto diets are high in saturated fats and low in fiber, which can increase inflammation and cholesterol. A 2021 study found the Mediterranean diet improved liver fat and fibrosis more than keto after 12 months. If you choose keto, focus on healthy fats like avocado and olive oil, not bacon and butter.
Are liver detox supplements effective?
No. There is zero scientific evidence that detox teas, powders, or cleanses improve liver function. Your liver naturally detoxifies your body. These products often contain herbs or ingredients that can actually harm the liver. The American Liver Foundation explicitly warns against them. Real healing comes from food, not pills.
How much protein should someone with liver disease eat?
Most people with early or moderate liver disease need 15-20% of daily calories from protein. That’s about 3 ounces per meal-like a deck-of-cards-sized portion of chicken, fish, tofu, or beans. Only in advanced cirrhosis with confusion (hepatic encephalopathy) might protein be temporarily limited-but even then, too little protein can cause muscle wasting, which worsens outcomes. Always work with a dietitian.
Can I still eat fruit on a liver-healthy diet?
Yes, absolutely. Whole fruit is fine-even for people with fatty liver. The fiber in fruit slows sugar absorption, preventing liver fat spikes. Avoid fruit juices and dried fruits, which are concentrated sources of sugar. Stick to whole berries, apples, oranges, and pears. Aim for two servings daily. Blueberries and grapes are especially helpful due to their anti-inflammatory compounds.
Is it expensive to eat a liver-healthy diet?
It can cost about $1.50 more per meal than a standard processed-food diet. But there are smart ways to save: buy frozen vegetables, cook in bulk, choose beans and lentils over meat, and shop seasonal produce. Community programs in places like Boston and Chicago have shown that with proper planning, you can cut costs by 35% while keeping meals nutritious. It’s an investment-but one that reduces future medical bills.
How long until I see results from a liver-healthy diet?
Many people feel better within 3-4 weeks-more energy, less bloating, clearer thinking. Liver enzymes often drop by 20-30% within 6 months. Liver fat reduction takes longer-typically 6-12 months. The key is sticking with it. Even small, consistent changes lead to measurable improvements. Don’t wait for a big transformation. Start where you are.
Should I avoid all alcohol if I have liver disease?
Yes. Even small amounts of alcohol can worsen liver damage, especially in fatty liver disease. There is no safe level for people with NAFLD or cirrhosis. Alcohol adds stress to an already overworked organ. If you drink, stopping is one of the most powerful things you can do for your liver-even more than diet alone in some cases.







9 Comments
Ali Miller
This is the most ridiculous piece of pseudoscience I've seen all week.
Who the hell says 'liver detox' doesn't exist? My cousin took milk thistle and his enzymes dropped 50% in 3 months.
You think a salad is going to fix years of binge drinking and McDonald's? LOL.
Science? More like corporate-sponsored propaganda.
They don't want you to know about real cures - they profit off your liver failure.
And don't even get me started on 'Mediterranean diet' - that's just fancy talk for 'eat like a poor Greek farmer.'
Meanwhile, real doctors prescribe meds for a reason.
Stop pushing food as medicine. It's dangerous. 🤡
Marissa Coratti
I appreciate the depth of evidence presented here, particularly the emphasis on the Mediterranean diet as a clinically validated intervention rather than a fleeting wellness trend.
It is imperative to underscore that non-alcoholic fatty liver disease (NAFLD), now reclassified as MASLD, is not merely a consequence of poor lifestyle choices but a complex metabolic condition influenced by genetics, epigenetics, and environmental factors.
That said, dietary modification remains the only intervention with reproducible, peer-reviewed outcomes in reversing hepatic steatosis and fibrosis.
The inclusion of anthocyanin-rich fruits, cruciferous vegetables, and monounsaturated fats aligns with the mechanistic pathways of nuclear factor erythroid 2-related factor 2 (Nrf2) activation and peroxisome proliferator-activated receptor alpha (PPARα) upregulation.
Furthermore, the reduction in fructose intake directly mitigates de novo lipogenesis in hepatocytes - a process that is both quantifiable and reproducible in randomized controlled trials.
It is also noteworthy that the PREDIMED trial demonstrated not only hepatic benefits but a 30% reduction in cardiovascular mortality - a critical point, as cardiovascular disease remains the leading cause of death in patients with MASLD.
While cost is a legitimate barrier, the assertion that frozen vegetables are nutritionally equivalent to fresh is supported by USDA data, and bulk legume purchases significantly reduce per-meal expenses.
For those seeking structure, I recommend the USDA’s MyPlate for Liver Health adaptation, which integrates these principles into a practical, scalable framework.
Consistency, not perfection, is the cornerstone of hepatic regeneration - and this article articulates that with remarkable clarity.
Micaela Yarman
I’m from Lebanon and this hits home. My grandma made this exact diet - no fancy labels, just olive oil, lentils, and fresh figs.
She lived to 94 with zero liver issues.
People think ‘healthy’ means expensive or boring - but real food? It’s just… food.
My mom still makes tabbouleh with parsley so fresh it stings your nose.
That’s the Mediterranean diet. Not a trend. A legacy.
And yeah, we didn’t need a study to tell us it worked.
We just knew. 🌿
mohit passi
bro the liver is a miracle organ 🤯
it regenerates if you stop beating it up
no magic pills just stop the sugar stop the fried stuff
eat real food
your body knows what to do
just stop getting in its way 🙏
Brittany Medley
I’m a registered dietitian specializing in hepatology, and I want to say - this is one of the most accurate, well-sourced, and compassionate summaries I’ve seen in a long time.
Too many influencers push ‘quick fixes’ that exploit fear - but this? This is medicine.
Also, the point about protein being safe for most with liver disease? Critical.
Many patients are still told to ‘limit protein’ out of outdated fear, when in reality, protein malnutrition accelerates muscle wasting and increases mortality.
And yes - coffee. Two cups. Black. No sugar. It’s a liver protector.
Also - frozen veggies? YES.
They’re flash-frozen at peak ripeness. Often more nutrient-dense than ‘fresh’ ones shipped across continents.
And if you’re worried about cost? Lentils, oats, cabbage, and eggs are your best friends.
One meal at a time. You’ve got this.
Ezequiel adrian
Y’all act like this is some new discovery.
My dad was a liver patient in Nigeria - no fancy clinics, no dietitians.
He ate garri, okra soup, and smoked fish.
Drank bitter leaf tea.
Walked 5km every day.
He’s alive at 72.
Don’t act like Western science invented healing.
We’ve been doing this for centuries.
And now you want to sell it as a $120 ebook? 🤡
JAY OKE
I started this diet 6 months ago.
Lost 22 lbs.
ALT dropped from 110 to 38.
Energy? Like I found a new battery.
Didn’t change anything else.
Just swapped soda for sparkling water.
Added broccoli.
Used olive oil.
That’s it.
My doctor said ‘you’re not supposed to reverse this.’
I said ‘well… I did.’
Joe bailey
Honestly this is the kind of post that makes me believe in humanity again.
So much noise out there about ‘detoxes’ and ‘keto miracles’ - but this? This is just… true.
My mum had fatty liver after menopause.
We started with one veggie-packed dinner a week.
Now? She makes her own hummus, eats walnuts like candy, and drinks black coffee like it’s water.
Her last scan showed ‘no signs of steatosis.’
She’s 68.
And she’s dancing.
Thank you for this.
Real food. Real results. No hype. 🙌
Amanda Wong
Let’s be real - this is just another ‘eat more veggies’ article dressed up as medical authority.
Where’s the long-term RCT data?
Who funded this?
Are you sure it’s not just correlation?
And why are you ignoring the fact that 70% of people with NAFLD are insulin resistant?
Changing your plate doesn’t fix your hormones.
Also - ‘coffee helps’? That’s it?
You’re ignoring the fact that caffeine increases cortisol in some people, which worsens visceral fat.
And why no mention of circadian rhythm?
This is dangerously oversimplified.
And you call it ‘science-backed’?
It’s anecdote with bullet points.
Stop misleading people.