Hot flashes that wake you up at 3 a.m. Night sweats so bad you need to change your pajamas. Mood swings that leave you wondering if you’re still you. If you’re going through menopause, you know these aren’t just inconveniences-they’re life disruptors. For decades, hormone therapy was the go-to fix. Then came the 2002 Women’s Health Initiative study, and everything changed. Suddenly, hormone therapy was seen as dangerous. But today, the science has caught up with real life. The truth isn’t black and white. For many women, especially those under 60 or within 10 years of their last period, the benefits of hormone therapy still outweigh the risks-if it’s done right.
What Exactly Is Hormone Therapy for Menopause?
Menopause hormone therapy (MHT), sometimes called hormone replacement therapy (HRT), replaces the estrogen your body stops making after menopause. If you still have a uterus, you also get progestogen. Why? Because estrogen alone can cause the lining of the uterus to thicken, raising the risk of endometrial cancer. Adding progestogen keeps that in check.
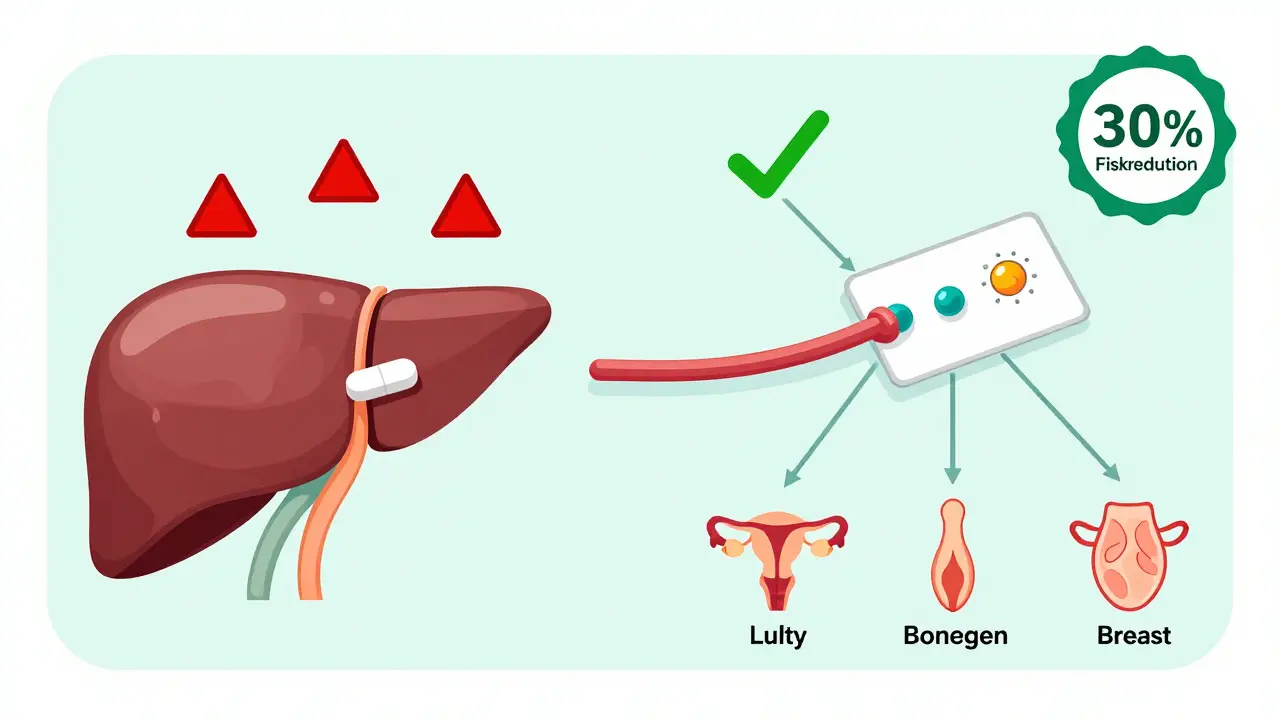
There are different ways to take it. Oral pills are common-like conjugated equine estrogens (Premarin) or 17-beta estradiol. But patches, gels, and sprays that go on your skin are becoming more popular. Why? Because they bypass your liver, which means less strain on your blood clotting system. Vaginal creams or rings are another option, mostly for dryness and discomfort during sex, not for hot flashes.
The goal isn’t to stay on it forever. It’s to use the lowest dose that works, for the shortest time needed. Most women find relief within a few weeks. For many, the therapy becomes unnecessary after 3 to 5 years.
The Big Benefits: More Than Just Hot Flashes
If you’re struggling with hot flashes and night sweats, hormone therapy is still the most effective treatment you’ve got. Studies show it cuts hot flashes by 75% compared to a placebo. That’s not a small win. It means sleeping through the night, staying focused at work, and not dreading social events because you might sweat through your shirt.
It also protects your bones. Estrogen helps keep bone density up. After menopause, bone loss speeds up. Women who skip hormone therapy are at higher risk of fractures-especially hip fractures, which can be life-altering after 60. One woman in a menopause forum shared that after 8 years on HRT, her DEXA scan showed stable bone density. Her sister, who refused therapy, broke her hip at 62.
Some women also notice improvements in skin elasticity and vaginal dryness. These aren’t just cosmetic. They affect quality of life, intimacy, and confidence.
The Real Risks: What You Need to Be Worried About
Here’s where it gets tricky. Hormone therapy isn’t risk-free. The biggest concerns are blood clots, stroke, breast cancer, and gallbladder disease.
Oral estrogen increases the risk of venous thromboembolism (VTE)-blood clots in the legs or lungs. The risk is low: about 3 in 1,000 women per year. But if you’re over 60, overweight, or have a history of clots, it’s not worth it. Transdermal estrogen (patches or gels) cuts that risk by about half. That’s why many doctors now recommend it as the first choice.
Stroke risk is also higher with oral estrogen, especially in older women. Transdermal forms show a 30% lower stroke risk, according to a 2018 study of 76,000 women.
Then there’s breast cancer. Estrogen-progestogen therapy increases risk slightly. The Women’s Health Initiative found 29 extra cases per 10,000 women per year. Estrogen-only therapy (for women without a uterus) shows almost no increase-just 9 extra cases per 10,000. And the longer you take it, the higher the risk. After 5 years, the risk starts to climb noticeably.
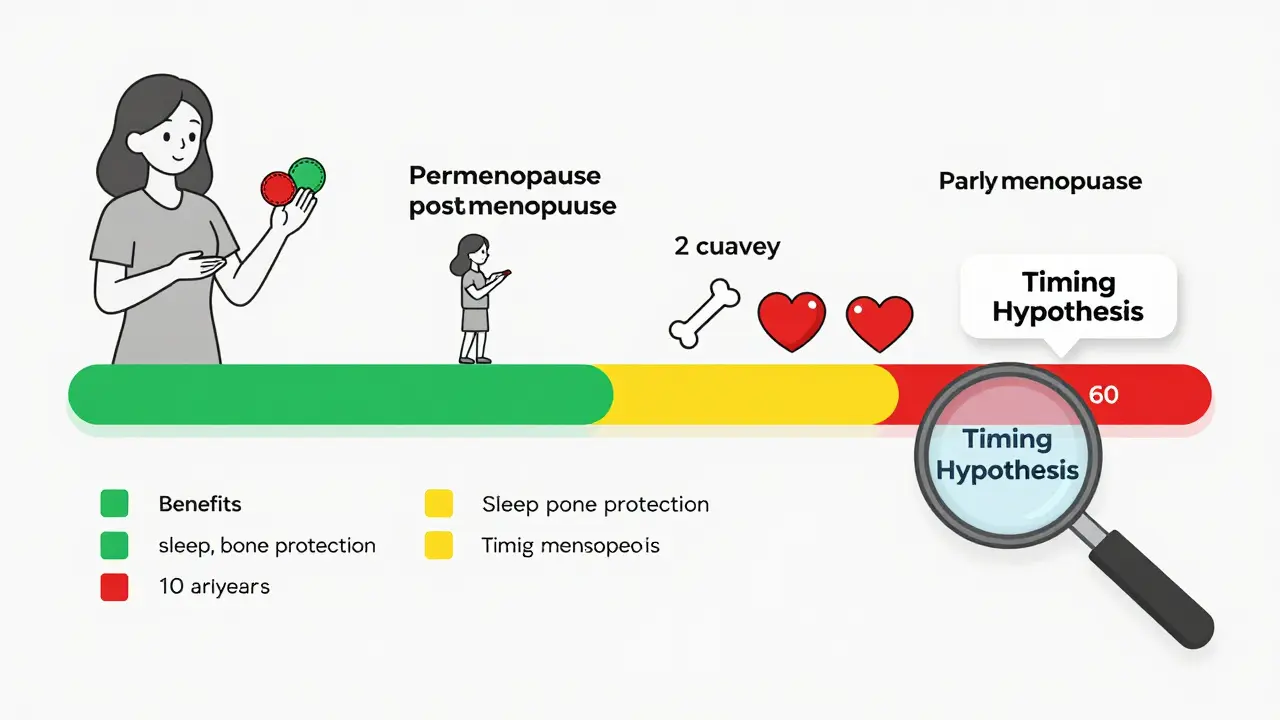
And here’s the key: timing matters. Starting hormone therapy before age 60 or within 10 years of your last period is much safer than starting later. That’s the “timing hypothesis.” If you wait until you’re 70, your body’s already changed. Hormones can trigger problems instead of preventing them.
What About Non-Hormonal Options?
If you’re nervous about hormones, there are other choices. But they’re not as powerful.
SSRIs like escitalopram or paroxetine can reduce hot flashes by about 50-60%. That’s helpful, but not the same as 75-90% with hormone therapy. Gabapentin helps too-about 45% reduction-but causes dizziness in 1 in 4 users. And herbal options like soy or black cohosh? The evidence is weak. A Cochrane Review found they reduce hot flashes by less than half a day compared to a placebo. That’s barely noticeable.
For bone health, bisphosphonates like alendronate are effective, but they come with their own side effects-jawbone issues, stomach upset, and the need to take them on an empty stomach with water and stay upright for 30 minutes. It’s not easy.
Hormone therapy still wins when it comes to symptom relief. If your hot flashes are severe, non-hormonal options might not cut it.
Who Should Avoid Hormone Therapy?
Not everyone is a candidate. You should not use hormone therapy if you have:
- A history of breast cancer
- History of blood clots, stroke, or heart attack
- Unexplained vaginal bleeding
- Active liver disease
- Known or suspected estrogen-sensitive cancer
Even if you don’t have these, your doctor will check your blood pressure, cholesterol, and family history. If your mom had a blood clot at 55, that’s a red flag. If you’re overweight or smoke, that increases risk too. It’s not about being perfect-it’s about balancing risks.
How to Get Started the Right Way
If you’re considering hormone therapy, don’t just ask your doctor for a prescription. Have a real conversation.
First, track your symptoms. Use the Menopause Rating Scale. How bad are your hot flashes? Sleep? Mood? That helps your doctor decide if therapy is worth it.
Second, ask about delivery method. Transdermal estrogen (patch or gel) is usually safer than pills, especially if you’re over 50 or have any risk factors for clots.
Third, start low. Try 0.05 mg of estradiol patch or 0.3 mg of oral conjugated estrogens. Most women don’t need more. If symptoms don’t improve in 4 weeks, your doctor might adjust it.
Fourth, expect some spotting in the first 3 to 6 months. That’s normal. If it lasts longer or gets heavier, call your doctor. It could mean your dose needs tweaking.
Finally, plan to re-evaluate every year. Ask yourself: Are my symptoms better? Am I still taking the lowest dose? Is the benefit still worth the risk? You might be able to stop sooner than you think.
What’s New in 2025?
The field is changing fast. In July 2025, the FDA opened a public docket to review how risks and benefits vary by age, dose, and type of hormone. A landmark study presented at The Menopause Society’s 2025 meeting looked at over 120 million patient records. It found that starting estrogen during perimenopause-before your periods fully stop-was linked to an 18% lower risk of heart problems than starting after menopause.
Doctors are moving toward personalized care. Some clinics are already testing how your body metabolizes estrogen based on genetics. That could one day tell you whether you’re more likely to benefit or face side effects.
And the stigma? It’s fading. In 2024, 42% of Fortune 500 companies started offering menopause support programs. That’s not just a perk-it’s recognition that this isn’t a phase you just endure. It’s a health issue that needs attention.
Real Stories, Real Outcomes
On Reddit, a woman named u/MenopauseWarrior wrote: “I went from 15-20 hot flashes a day to 2-3 in 10 days on a 0.05 mg estradiol patch. I slept through the night for the first time in years.”
Another woman on HealthUnlocked said: “I took Prempro and got awful bloating and mood swings. I quit after 3 months. I didn’t blame the medicine-I blamed the dose. My doctor didn’t listen.”
That’s the thing. It’s not about hormone therapy being good or bad. It’s about finding the right version for you. The right dose. The right delivery method. The right timing.
For many women, it’s the difference between surviving menopause and thriving through it.
Is hormone therapy safe for women under 60?
Yes, for most women under 60 or within 10 years of menopause, hormone therapy is considered safe and effective when used at the lowest dose for the shortest time needed. The benefits-relief from hot flashes, protection against bone loss-typically outweigh the small increased risks of blood clots and breast cancer in this group. Starting therapy later, especially after 60, increases risks without clear benefits.
Do patches cause fewer side effects than pills?
Yes. Transdermal estrogen (patches, gels, sprays) avoids first-pass liver metabolism, which lowers the risk of blood clots and stroke by about 30-50% compared to oral pills. It also tends to cause less bloating and mood swings. Many doctors now recommend patches as the first choice, especially for women over 50 or with risk factors like high blood pressure or obesity.
Can hormone therapy help with sleep problems during menopause?
Yes, indirectly. Night sweats and hot flashes are the main reason women wake up at night during menopause. By reducing those symptoms, hormone therapy often restores deep, uninterrupted sleep. Some women report sleeping through the night for the first time in years after starting therapy. It’s not a sleep aid, but it removes the main barrier to good sleep.
How long should I stay on hormone therapy?
There’s no one-size-fits-all answer. Most women take it for 3 to 5 years. But if your symptoms are severe and you’re still under 60, you may continue longer. The key is annual reviews. Ask yourself: Are my symptoms still bothersome? Can I lower the dose? Is the benefit still worth the risk? Many women taper off successfully after 5 years. Others stay on low-dose therapy for bone protection, especially if they have osteoporosis.
Does hormone therapy cause weight gain?
No, hormone therapy doesn’t directly cause weight gain. The weight gain many women experience during menopause is due to aging, changing metabolism, and loss of muscle mass-not hormones. Some women report bloating or fluid retention early on, especially with oral pills, but that usually settles. If you’re gaining weight, focus on diet, strength training, and sleep-those matter more than whether you’re on HRT.
What if I had breast cancer in the past?
Hormone therapy is generally not recommended for women with a history of estrogen-receptor-positive breast cancer. Estrogen can fuel the growth of some breast cancers. Even low-dose or transdermal forms carry risk. If you’ve had breast cancer, talk to your oncologist about non-hormonal options like SSRIs, gabapentin, or lifestyle changes to manage symptoms.







10 Comments
Vikram Sujay
Hormone therapy, as a medical intervention, must be understood within the broader framework of physiological transition and individual biochemistry. The reduction of symptom severity does not inherently negate the systemic risks, nor does the absence of symptoms validate long-term safety. One must weigh not only the immediate relief but the epistemological certainty of longitudinal outcomes, which remain imperfectly mapped in contemporary literature.
mark etang
The scientific consensus has evolved, and it is now clear that for appropriately selected patients, hormone therapy remains a clinically superior option for managing vasomotor symptoms and preserving bone integrity. The data supporting transdermal administration over oral formulations is robust and should inform first-line clinical recommendations. This is not a matter of opinion-it is evidence-based medicine.
Brendan F. Cochran
they say hrt is safe now but last time i checked the fda still lists blood clots and cancer as risks... why are we pretending this is just a 'lifestyle choice' like coffee? they want us on pills so the pharma giants keep raking it in. wake up people. this ain't medicine, it's marketing.
jigisha Patel
It is statistically indefensible to claim that hormone therapy 'benefits outweigh risks' for women under 60 without specifying the exact cohort, duration, and formulation. The WHI data, while outdated, remains foundational. The 2018 transdermal study you cite had a 30% lower stroke risk-relative to what? Absolute risk remains negligible for most, but when applied to a population of 30 million, 'negligible' becomes catastrophic. Precision matters.
Jason Stafford
They’re hiding the truth. The same people who pushed HRT in the 90s are the ones writing the new guidelines. The FDA’s new docket? A distraction. They know estrogen accelerates tumor growth in latent cancers. They know it alters liver enzymes to favor clotting. They don’t care because they’re paid by the labs that make the patches. You think your doctor’s advice is independent? Think again.
Mandy Kowitz
Oh wow, so now we’re supposed to be grateful that Big Pharma gave us a magic pill to stop sweating through our blouses? How noble. Meanwhile, my 72-year-old aunt who never took hormones is hiking in Patagonia and I’m on a patch that makes me feel like a lab rat. Thanks, science.
Justin Lowans
There is profound wisdom in the principle of minimal intervention: use the lowest effective dose, for the shortest necessary time. This approach honors both the body’s natural rhythm and the ethical imperative to avoid iatrogenic harm. For many women, the restoration of sleep, focus, and emotional equilibrium is not trivial-it is transformative. Let us not dismiss this because perfection is unattainable.
Cassie Tynan
Let’s be real: the real villain here isn’t estrogen-it’s the fact that medicine still treats menopause like a personal failing rather than a biological milestone. We’re told to ‘tough it out’ or ‘take a pill,’ but nobody asks why society doesn’t adapt to aging women instead of forcing them to chemically conform. HRT might help, but it shouldn’t be the only option we’re given.
Rory Corrigan
Everything is energy, man. Estrogen isn’t just a molecule-it’s a vibration. When you suppress your natural rhythm with synthetic hormones, you’re out of sync with the earth’s cycles. I’ve been off everything since 2020. Cold showers, moon cycles, and breathwork. My hot flashes? They’re just my soul clearing out old energy. 🌙
Stephen Craig
Transdermal estrogen reduces clot risk. Start low. Re-evaluate yearly. That’s it.