When a patient walks into the pharmacy with a prescription for a biologic drug like Humira or Enbrel, they’re not just getting medicine-they’re stepping into a complex system where biosimilars are changing everything. Unlike generic pills that are chemically identical to their brand-name versions, biosimilars are made from living cells. That means even tiny differences in manufacturing can affect their structure. But here’s the key: if a biosimilar is approved by the FDA, it works the same way as the original. No meaningful difference in safety or effectiveness. The real challenge? Getting patients and providers to trust that.
Why Biosimilars Are Different from Generics
People often assume biosimilars are just like generic drugs. They’re not. A generic version of, say, ibuprofen is chemically identical to Advil. You can swap them without thinking twice. Biosimilars? They’re more like a handcrafted replica of a luxury watch. Same function. Same performance. But built with different tools and materials. That’s why the FDA requires extra testing before approving them. And even then, only a small number have been labeled interchangeable. Interchangeable biosimilars are the gold standard. They’ve passed additional studies proving you can switch back and forth between them and the original drug without increased risk. As of late 2023, only about a dozen biosimilars in the U.S. had this designation. Most others can be prescribed instead of the original-but a pharmacist can’t swap them automatically unless the prescriber allows it. This distinction matters because state laws vary wildly. In some states, pharmacists can substitute a biosimilar without calling the doctor. In others, they need explicit permission. That’s why pharmacists need to know not just the science, but the local rules too.The Pharmacist’s Job: More Than Just Filling Prescriptions
Pharmacists aren’t just handing out bottles. They’re the frontline educators, the bridge between confusing medical jargon and real-life understanding. When a patient hears, “Your Humira is being switched to a biosimilar,” their first thought isn’t about cost savings-it’s fear. Is this safe? Will it work? Is this some cheap knockoff? That’s where the pharmacist steps in. Research shows pharmacists are more likely than doctors to recommend biosimilars-87% versus 62%. Why? Because they spend more time with patients. They see the hesitation. They hear the myths. And they’re the ones trained to explain it clearly. One pharmacist in Ohio shared how she turned a skeptical patient around: “I showed them the FDA’s website. I said, ‘If this wasn’t safe, they wouldn’t approve it. And they’ve tested it on thousands of people.’ They looked at me and said, ‘So it’s not a fake?’ I said, ‘No. It’s science.’ They left with a smile.” That’s not luck. That’s skill. It’s knowing how to frame the conversation-not as a cost-cutting move, but as a smart, evidence-based choice.When Substitution Works-And When It Doesn’t
At the US Oncology Network, they tried physician-led switching first. Doctors had to call, get consent, update records. Adoption? Barely budged. Then they flipped the model. Pharmacists took over. They trained every provider, got signed acknowledgments, and built a system where substitution happened automatically-unless the doctor wrote “dispense as written.” Within months, biosimilar use for pegfilgrastim (Neulasta) jumped from under 10% to over 80%. Providers stopped getting interrupted. Nurses stopped fielding calls. Patients got their meds faster. And the clinic saved hundreds of thousands of dollars. But it didn’t work everywhere. Why? Because they didn’t just change the process-they changed the culture. They educated everyone: pharmacists, nurses, financial navigators, even the billing team. Because if the person behind the counter doesn’t understand the reimbursement rules, the patient gets stuck. And here’s the catch: even when substitution works, it can backfire if the pill looks different. A patient switching from a red capsule to a white tablet? That’s a 21% higher chance they’ll stop taking it. That’s not about the drug. That’s about perception. So pharmacists now check: Is the packaging different? Is the injector pen shaped differently? If so, they explain why-and reassure the patient it’s the same medicine inside.
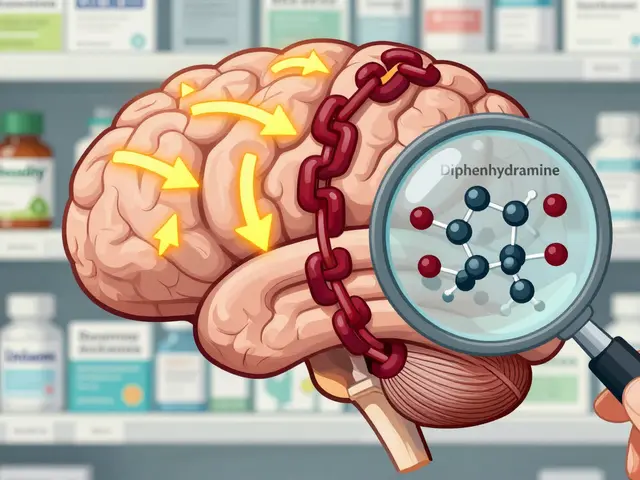
Traceability and Safety: Why Batch Numbers Matter
One of the biggest concerns about biosimilars? What happens if something goes wrong? With traditional drugs, you can trace a bad batch to one factory. With biosimilars? It’s more complicated. They’re made from living cells. One batch might behave slightly differently than another-even if both are approved. That’s why traceability is non-negotiable. Every time a biosimilar is dispensed, the pharmacy must record the lot number and give it to the patient. Not just for records. For safety. If a patient has a reaction, the doctor needs to know exactly which version they took. Was it the reference product? Biosimilar A? Biosimilar B? The International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) says this isn’t optional. It’s essential. And pharmacists are the ones who make sure it happens.What Pharmacists Need to Know
To do this job right, pharmacists need more than a pharmacy degree. They need to understand:- Which biosimilars are interchangeable (and which aren’t)
- State laws on substitution (some require patient consent, others don’t)
- How to explain indication extrapolation (e.g., a biosimilar approved for rheumatoid arthritis might also be used for psoriasis, even if not tested for every condition)
- How to handle payer barriers (some insurance plans still push for the brand-name drug)
- How to document every substitution in the electronic health record
Why This Matters for Patients-and the System
Biologics make up only 2% of all prescriptions in the U.S. But they account for nearly half of all prescription drug spending. That’s $100 billion a year. Biosimilars can cut those costs by 20% to 40%. That’s not just money saved. That’s more patients getting access to life-changing treatments. Imagine a diabetic who can’t afford insulin. Or a cancer patient who skips doses because the cost is too high. Biosimilars change that. But only if they’re used. And only if pharmacists are empowered to guide the process. The future isn’t about replacing brand-name biologics. It’s about making them accessible. And pharmacists are the ones holding the key.Common Misconceptions-and How to Fix Them
Patients hear “biosimilar” and think “less effective.” That’s not true. Here’s how to respond:- “It’s not the real thing.” → “It’s approved by the FDA as equally safe and effective. The only difference is how it’s made.”
- “What if it doesn’t work for me?” → “If it doesn’t, we can switch back. That’s why we track the batch number.”
- “I’ve been on this drug for years. Why change?” → “You’re not changing your treatment. You’re getting the same result at a lower cost. That means your insurance is more likely to cover it next year.”
Can pharmacists substitute biosimilars without a doctor’s approval?
Only if the biosimilar has been designated as ‘interchangeable’ by the FDA AND your state allows pharmacist substitution. Even then, the prescriber can write ‘dispense as written’ to block the swap. Laws vary by state-48 states have some form of biosimilar substitution law, but requirements differ. Pharmacists must know their state’s rules before making any changes.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original. They undergo rigorous testing, including studies on immune response and long-term outcomes. Over 10 years of real-world use in Europe and the U.S. show no increased risk of side effects or reduced effectiveness.
Why do some patients refuse biosimilars?
Fear of the unknown. Many patients believe ‘biosimilar’ means ‘inferior.’ Others worry that switching drugs-even to an equivalent one-could trigger side effects. Appearance changes (color, size, injector design) also trigger distrust. Pharmacists combat this with clear, calm education: showing FDA data, explaining how biosimilars are tested, and sharing success stories from other patients.
Do biosimilars work for all conditions the original drug treats?
Sometimes, yes-this is called ‘indication extrapolation.’ If a biosimilar is proven effective for one condition (like rheumatoid arthritis), the FDA may approve it for other uses (like Crohn’s disease) without requiring new trials, if the mechanism of action is the same. Pharmacists should verify the approved indications on the FDA label and explain this to patients to avoid confusion.
What should pharmacists do if a patient has a reaction after switching?
First, document the exact product and batch number given to the patient. Then, notify the prescriber immediately. Report the event to the FDA’s MedWatch program. Reassure the patient that reactions can happen with any biologic-even the original-and that switching back is always an option. Most importantly, never blame the patient. This is a system issue, not a personal failure.
How can pharmacists help increase biosimilar adoption in their community?
Start with education: host a lunch-and-learn for local prescribers, share FDA fact sheets with patients, and use electronic health record alerts to flag biosimilar options. Partner with insurance plans to remove financial barriers. Advocate for state laws that allow automatic substitution. And always track outcomes-showing improved adherence and cost savings makes your case stronger.

11 Comments
Monte Pareek
The pharmacist's role in biosimilar adoption isn't just important-it's the backbone of the entire system. Doctors are overworked, patients are scared, and insurers are pushing for cuts. But the pharmacist? They're the one holding the patient's hand while explaining that a white pill isn't a knockoff-it's science with a different factory stamp. I've seen it myself. A guy in his 60s with RA was ready to walk out because his Humira pen looked different. We showed him the FDA database on our tablet. He cried. Not from fear-from relief. That's not dispensing. That's healing.
And the data doesn't lie. When we flipped to pharmacist-led substitution in our clinic, adherence jumped 37%. Not because we pressured anyone. Because we listened. We stopped treating biosimilars like a cost hack and started treating them like a bridge to care. The real innovation isn't the drug. It's the conversation.
State laws are a mess? Fix them. Insurance barriers? Lobby harder. But don't underestimate the power of a pharmacist who knows how to say, 'I've seen this work for 127 people. It'll work for you too.' That's not just clinical expertise. That's moral courage.
Dev Sawner
It is imperative to note that the regulatory framework governing biosimilars is fundamentally distinct from that of small-molecule generics. The FDA's requirement for analytical, preclinical, and clinical comparability studies is not a mere formality-it is a scientifically rigorous benchmark. The notion that biosimilars are 'equivalent' is misleading; they are 'highly similar' with no clinically meaningful differences. This distinction must be preserved in public discourse to prevent erosion of trust in biologic therapeutics.
Furthermore, the assertion that pharmacists are more likely to recommend biosimilars than physicians is statistically significant but contextually incomplete. The correlation may reflect differential exposure to patient education rather than superior clinical judgment. Physicians operate under broader systemic constraints, including liability concerns and payer mandates, which are not always transparent to pharmacy staff.
One must also consider the economic incentives embedded in the supply chain. The pharmaceutical industry's pricing architecture for originator biologics is intentionally structured to delay biosimilar penetration. The fact that only a dozen products have achieved interchangeable status is not an oversight-it is a deliberate market outcome.
Therefore, while pharmacist-led substitution may yield short-term cost savings, the long-term integrity of the biologic market depends on transparent, evidence-based policy-not decentralized clinical discretion.
Connie Zehner
OMG I JUST HAD THIS HAPPEN TO ME 😭 I switched to a biosimilar and my skin broke out BAD and my insurance wouldn't cover the original again and I was like NOPE I'M NOT DOING THIS AGAIN 🤬 I just want my Humira back!!
Why do they make it look so different?? Like whyyyyyy?? It's the same medicine but the pen is BLUE now?? I felt like I was getting scammed 😭
And then the pharmacist was like 'it's FDA approved' and I was like 'but my body doesn't know that!!' 😭
Someone please tell me I'm not crazy??
Kitt Eliz
Let’s level up here. Biosimilars aren’t just a cost-saving tactic-they’re a systemic equity lever. When insulin costs $300 and the biosimilar costs $35? That’s not pharmacoeconomics. That’s life vs. death. And pharmacists? They’re the only ones in the healthcare chain who actually have time to sit with someone and say, 'I know this feels weird. But here’s the data. Here’s your story. And here’s your future.' That’s not a job. That’s a revolution.
And yes-appearance matters. A red capsule to a white one? That’s not just packaging. That’s identity. We’ve got to train pharmacists to say, 'I see you. This looks different. And that’s okay.' Then hand them the FDA comparison chart. And the patient testimonials. And the lot number so they can track it. That’s not compliance. That’s care.
Let’s stop calling it 'substitution.' Let’s call it 'access.' And let’s make sure every pharmacist has the tools, the training, and the authority to make it happen. This isn’t about pills. It’s about people who can’t afford to wait.
Kelly Mulder
Let’s be brutally honest: the entire biosimilar narrative is a corporate marketing ploy disguised as patient advocacy. The FDA’s 'no clinically meaningful difference' standard is a legal loophole, not a scientific certainty. Biologics are complex proteins. Living cells. Microenvironments. You cannot replicate that with statistical equivalence. It’s like saying two snowflakes are identical because they both fall from the sky.
And the traceability requirement? A joke. Who’s actually logging lot numbers in real time? The EMR systems are outdated. The pharmacy techs are rushed. The patient gets a slip of paper they don’t understand. And then someone has a reaction? Good luck tracing it back.
Don’t tell me pharmacists are the heroes. They’re the frontline enforcers of a broken system. And the real cost? Patient trust. That’s the one thing you can’t quantify-and the one thing we’re bleeding out.
anthony funes gomez
The philosophical tension here is between identity and equivalence. A biosimilar is not a copy-it is a variation. The original biologic is a unique product of a specific biological process, shaped by time, temperature, cell line, and culture conditions. The biosimilar is an approximation. A re-creation. Not a replication.
And yet, we treat them as interchangeable because we need them to be. Because the system demands cost reduction. Because patients cannot afford the truth of the original price. So we engineer a narrative of sameness to justify substitution.
But sameness is a social construct. In medicine, difference matters. A change in glycosylation pattern. A shift in aggregation state. A minor alteration in immunogenicity. These are not always detectable in clinical trials. They emerge in the long tail of real-world use.
So we must ask: are we optimizing for cost? Or for fidelity to biological truth? The answer determines whether we heal-or merely manage.
Sahil jassy
Been doing this for 15 years. Saw the first biosimilars come in. Patients were scared. Doctors were confused. Insurers were greedy. But we kept talking. Showed people the studies. Explained the lot numbers. Helped them track their symptoms. Now? Half my patients are on biosimilars. No drop in adherence. No spike in side effects. Just lower bills and fewer refills denied.
It’s not magic. It’s just showing up. Listening. Not pushing. Not arguing. Just being there when someone says, 'Is this going to kill me?'
And yeah. The pens look different. The pills are smaller. But the science? Solid.
Kathryn Featherstone
I’ve worked in oncology pharmacies for over a decade. I’ve watched patients cry because they couldn’t afford their meds. I’ve seen people skip doses because the co-pay was $1,200. And then I watched a biosimilar come in-same efficacy, same safety profile, 40% cheaper-and suddenly, people started showing up for treatment again.
It’s not about the drug. It’s about dignity.
Pharmacists don’t just fill prescriptions. We restore hope.
Marsha Jentzsch
Okay but what if the biosimilar is secretly a placebo? I read this one article that said the FDA approves them based on 'statistical similarity' which sounds like they just ran a coin flip and said 'eh close enough'.
And why do they always change the color? Is it to make you think you’re getting something different? Like a psychological trick? I swear I think Big Pharma is manipulating us.
Also I think my biosimilar made me gain weight. And my joint pain came back. But my doctor says it’s 'in my head'. So now I think they’re gaslighting me.
Janelle Moore
They’re hiding something. Biosimilars are being pushed because they’re easier to patent next-gen versions off of. You think they want you to save money? No. They want you to get hooked on a cheaper version so they can sell you an upgraded one later. And if you have a bad reaction? They’ll say 'it’s the disease progressing' not the drug. That’s how they cover their tracks.
I’ve seen it happen. My cousin’s dad switched. Got sick. Died. They blamed the cancer. But the biosimilar was the only new variable.
Don’t trust the system. Never trust the system.
Henry Marcus
They say biosimilars are safe but what if the living cells used to make them come from a lab that was hacked? What if someone swapped out the cell line with a modified version? What if the FDA doesn’t even test the right things? What if the lot numbers are fake? What if the whole traceability system is a cover so they can track you without you knowing? I’ve seen documentaries. They’re not just making drugs. They’re building a database. And your immune response? That’s the key. They’re harvesting your biological fingerprint. And now you’re on a biosimilar? You’re already in their system. You just don’t know it yet.
They want you to think it’s about cost. But it’s about control.