When you're taking more than one psychiatric medication, the risk of dangerous interactions doesn't just go up-it explodes. It's not theoretical. Every year, thousands of people end up in emergency rooms because two medications they were told were safe to take together ended up triggering something life-threatening. The worst part? Many of these cases are completely preventable.
Why Psychiatric Drug Interactions Are So Risky
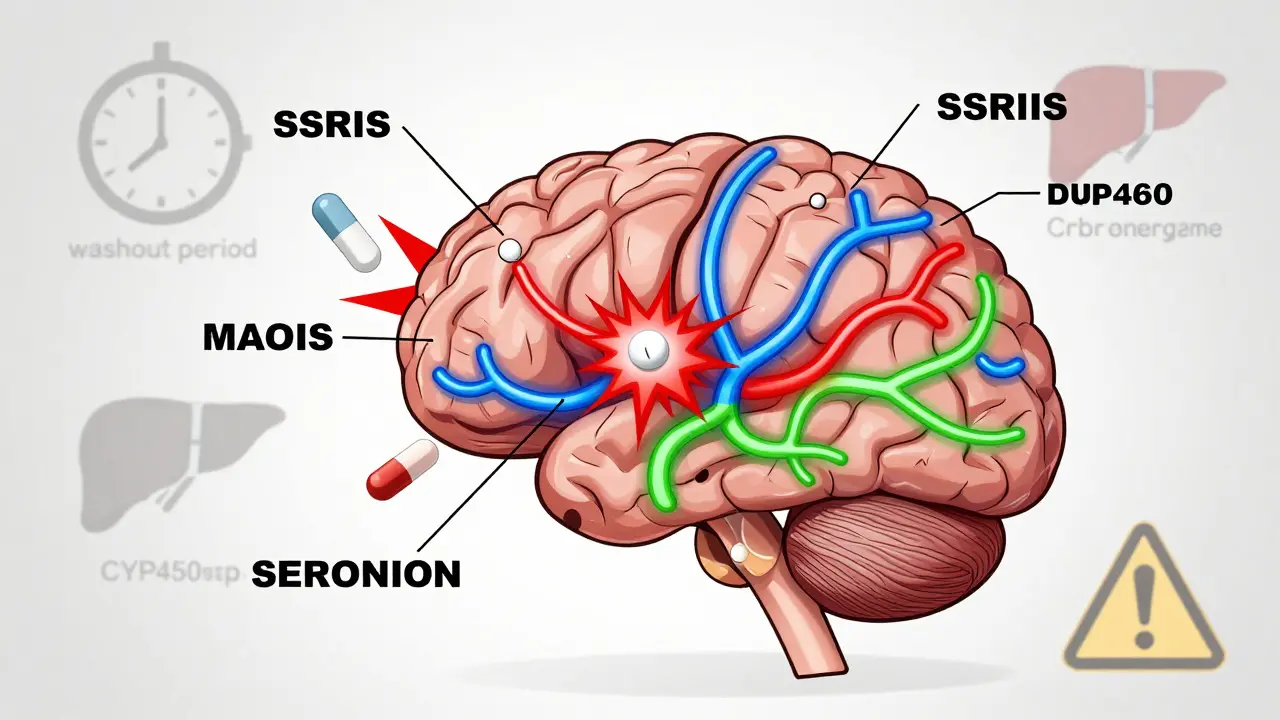
Psychiatric medications don't work in isolation. They tweak your brain chemistry-serotonin, norepinephrine, dopamine-and when two or more of them are mixed, they can amplify each other in ways doctors don't always predict. Unlike antibiotics or painkillers, these drugs target the same systems in your nervous system, so even small overlaps can become big problems. Take serotonin, for example. It's a key player in mood, sleep, and anxiety. SSRIs like fluoxetine and SNRIs like venlafaxine boost serotonin levels. So do certain opioids, migraine meds, and even some herbal supplements like St. John’s wort. Add an MAO inhibitor like phenelzine on top? That’s when serotonin levels can spike uncontrollably. This isn't just feeling jittery-it's serotonin syndrome, a condition that can cause high fever, seizures, irregular heartbeat, and even death. Mortality rates in severe cases range from 2% to 12%.The Most Dangerous Combinations
Some drug pairs are so risky they're basically red flags. Here are the top three you need to know:- MAO inhibitors + SSRIs/SNRIs: This combo is the classic serotonin syndrome trigger. Even with a washout period, if you switch from one to the other too soon, you're playing Russian roulette with your brain chemistry. The rule? Wait at least 14 days after stopping an MAOI before starting an SSRI. Some experts recommend 21 days for fluoxetine because it sticks around longer.
- TCAs + antihistamines or alcohol: Tricyclic antidepressants like amitriptyline already cause drowsiness, dry mouth, and blurred vision. Add diphenhydramine (Benadryl) or a glass of wine, and your central nervous system can shut down. This isn't just dizziness-it's respiratory depression, low blood pressure, and risk of falling or cardiac arrest.
- Lithium + NSAIDs or diuretics: Lithium has a tiny therapeutic window-0.6 to 1.0 mmol/L. Too little, and it doesn't work. Too much, and you get tremors, confusion, kidney damage, or seizures. NSAIDs like ibuprofen or naproxen can raise lithium levels by 25-50%. Even a single dose of a diuretic like hydrochlorothiazide can push you over the edge.
How Enzymes Make Things Worse
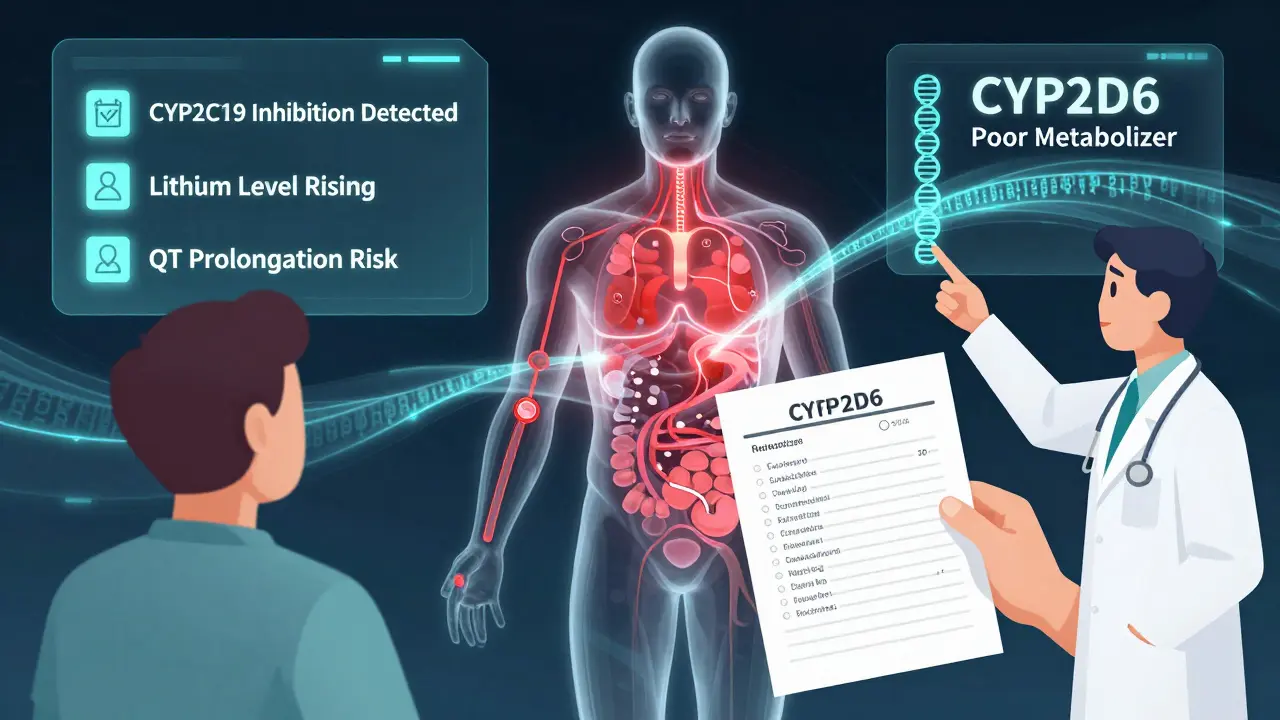
Your liver uses enzymes-especially CYP450 enzymes-to break down medications. Some psychiatric drugs slow down these enzymes, causing others to build up to toxic levels. Fluvoxamine is one of the worst offenders. It strongly inhibits CYP1A2, 2C9, 2C19, and 3A4. That means if you're on fluvoxamine and also take clozapine, theophylline, or even caffeine, those drugs can accumulate dangerously. Even medications you think are harmless can be risky. For example, omeprazole (a common heartburn pill) inhibits CYP2C19. If you're on citalopram (which relies on that enzyme), omeprazole can push citalopram levels too high, increasing your risk of heart rhythm problems like QT prolongation.
Who’s Most at Risk?
It’s not just about what you’re taking-it’s who you are. Older adults metabolize drugs slower. People with liver or kidney disease can’t clear medications efficiently. And if you’re on three or more psychiatric meds, your risk jumps dramatically. Studies show 30-50% of adverse drug events in psychiatric care come from interactions. People on polypharmacy regimens-like someone taking an SSRI, an antipsychotic, and lithium for bipolar disorder-are especially vulnerable. These aren’t rare cases. They’re the norm in many clinics. That’s why the American Association of Psychiatric Pharmacists insists on first-dose monitoring. If you start a new combo, you need to be observed for at least 2-4 hours after the first dose. No exceptions.What Doctors Should Be Doing
Good prescribers don’t just write prescriptions. They track. They monitor. They use tools.- PHQ-9 and GAD-7 to track depression and anxiety symptoms over time.
- AIMS to check for involuntary movements if you’re on antipsychotics-assessed quarterly.
- Drug interaction databases like Lexicomp or Micromedex-consulted before every new prescription.
- Laboratory monitoring: Lithium levels every 3-6 months, liver enzymes for valproate, complete blood counts for clozapine (weekly for the first 6 months).
What You Can Do to Stay Safe
You don’t have to be passive in your care. Here’s what you can do:- Keep a written list of every medication you take-including supplements, OTC drugs, and even occasional painkillers.
- Ask your doctor: “Is this new med safe with what I’m already taking?” Don’t assume they know.
- Use a pharmacy that offers medication reviews. Many chain pharmacies now do this for free.
- Watch for warning signs: confusion, muscle rigidity, high fever, rapid heartbeat, sweating. If you feel these, go to the ER. Don’t wait.
- Don’t stop or start anything without talking to your prescriber-even if it’s something you think is “natural.”
The Future: Better Tools, Fewer Mistakes
The good news? Tools are getting smarter. Digital systems now alert doctors in real time when a dangerous combo is prescribed. One study showed a 37% drop in serious interaction events when these systems were used properly. Genetic testing is also becoming more common. If you have a CYP2D6 or CYP2C19 poor metabolizer variant, certain antidepressants can build up to toxic levels even at normal doses. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has clear guidelines for this now. Ask your doctor if pharmacogenomic testing is right for you. And AI models are being tested by the National Institute of Mental Health. In the next few years, these systems may predict your personal risk based on your genes, age, liver function, and exact medication list-before you even take the first pill.Bottom Line: Knowledge Saves Lives
Psychiatric medications can be life-changing. But they’re not harmless. The biggest danger isn’t the drugs themselves-it’s the assumption that combining them is safe. Serotonin syndrome, lithium toxicity, and CNS depression don’t come with warning labels you can read online. They come on suddenly, often after a single new dose. The solution isn’t avoiding treatment. It’s being informed. Track your meds. Ask questions. Demand monitoring. If your doctor doesn’t talk about interactions, find one who does. Your brain-and your body-deserve nothing less.Can I take over-the-counter painkillers with my antidepressant?
It depends. NSAIDs like ibuprofen or naproxen can dangerously raise lithium levels and increase bleeding risk when combined with SSRIs or SNRIs. Acetaminophen (Tylenol) is usually safer, but it can stress the liver if you're also on medications like valproate or clozapine. Always check with your doctor or pharmacist before taking any OTC drug.
How long should I wait between stopping an MAOI and starting an SSRI?
Wait at least 14 days. For fluoxetine (Prozac), which stays in your system longer, wait 21 days. This isn’t a suggestion-it’s a safety requirement. Jumping from an MAOI to an SSRI too soon can trigger serotonin syndrome, which can be fatal.
Are newer antidepressants safer than older ones?
Generally, yes. SSRIs like sertraline and citalopram have fewer drug interactions than older TCAs or MAOIs. Vilazodone and vortioxetine also have lower interaction potential. But no drug is risk-free. Even newer meds like brexanolone or cariprazine can interact with other psychiatric drugs. Always review your full list with your prescriber.
Can herbal supplements interact with psychiatric meds?
Yes, and often dangerously. St. John’s wort can cause serotonin syndrome when taken with SSRIs. Kava can increase sedation when combined with benzodiazepines or antipsychotics. Even ginkgo biloba can raise bleeding risk. Always tell your doctor about every supplement you take-even if you think it’s harmless.
What should I do if I think I’m having a drug interaction?
If you experience sudden confusion, high fever, muscle stiffness, rapid heartbeat, or seizures, go to the emergency room immediately. These are signs of serotonin syndrome or other serious interactions. Don’t wait. Don’t call your doctor first-get help now. Bring your medication list with you.






13 Comments
Kiran Plaha
I took sertraline and ibuprofen for months without knowing the risk. My doctor never mentioned it. I got dizzy one day and thought it was just stress. Turns out my lithium levels were creeping up. Scary stuff. Always ask.
Matt Beck
Brooo... serotonin syndrome isn't just 'feeling off' 😵💫 it's your brain screaming for mercy. MAOIs + SSRIs? That's not a combo, that's a death wish with a prescription. 🚨 I once saw a guy turn purple in the ER. No joke. #medsarenottoys
Ryan Barr
Pharmacology is not a suggestion. It’s a law of physiology. Ignorance kills.
Cam Jane
Hey everyone - if you're on more than two psych meds, please, PLEASE get a med review at your pharmacy. They’re free, they’re fast, and they could save your life. I work in a clinic and I’ve seen too many people get caught off guard by OTC stuff. Benadryl? Sounds harmless, right? Nope. It’s like pouring gasoline on a candle when you’re on TCAs. Don’t wait until you’re shaking to ask. Talk to someone before you take that next pill. You’re not being paranoid - you’re being smart.
Dana Termini
I appreciate how thorough this is. Most people don’t realize how much overlap there is between meds and supplements. I used to take St. John’s wort because it was 'natural.' Turns out, natural doesn’t mean safe. Now I keep a printed list and show it to every provider. Simple habit. Huge difference.
Wesley Pereira
so uhhhh... if u r on fluvoxamine and drink coffee... are u just a walking time bomb? 🤔 c'mon man. i thought my jitters were just from work. turns out my caffeine levels were 3x normal. thanks for the heads up doc. i’m gonna go drink some tea now. #cyp450isreal
Isaac Jules
Anyone who doesn’t monitor their lithium levels is a walking liability. And if your doctor doesn’t order regular labs? Fire them. This isn’t ‘maybe you should’ - this is ‘you’re gonna die if you don’t.’ Stop being lazy. Your brain isn’t a toy.
Amy Le
Why do Americans think they can just stack pills like candy? In India, they don’t do this. They trust their doctors. Here? Everyone’s a DIY chemist. You take 3 antidepressants, a painkiller, a sleep aid, and St. John’s wort? You’re not brave - you’re just stupid. This isn’t science. It’s a horror movie.
Pavan Vora
My uncle in Delhi took fluoxetine and then used ayurvedic herbs for depression... ended up in ICU with serotonin syndrome. We didn’t know it was possible. Now I tell everyone - even if it’s from grandma’s recipe, ask the doctor first. 🙏 India needs more awareness. Not just here - everywhere.
Stuart Shield
There’s something deeply human about how we treat our brains like machines we can tweak with a menu. We’ll pop a pill for sadness like it’s a light switch - but never check the wiring. This post? It’s not just info. It’s a quiet plea for humility. We’re not gods. We’re fragile, messy, beautifully broken things trying to stay alive. Treat your meds like you’d treat a live wire - with care, not curiosity.
Indra Triawan
I’ve been on 5 meds for 8 years. No one ever told me about CYP enzymes. Now I feel like I’ve been poisoned slowly. I’m not mad. I’m just... hollow. Like my body’s been a lab rat and no one even thanked me.
Susan Arlene
took tylenol for a headache. felt weird. didn’t think much. turned out my liver was struggling with valproate. lesson learned: if it’s not on your script, ask. simple.
Joann Absi
THIS IS WHY AMERICA IS DOOMED 😭💊 Everyone’s on something. Everyone’s mixing it. No one’s reading labels. I saw a TikTok where some girl said she took Adderall with Zoloft for ‘focus’... I cried. We’re not just dying. We’re dying because we think we’re influencers. Wake up.