Apixaban Perioperative Dosing Calculator
Procedure Risk Assessment
Recommended Action
Stop Apixaban
72 hours
Moderate risk procedure
Apixaban is a direct oral anticoagulant (DOAC) that blocks factor Xa, preventing clot formation in atrial fibrillation and venous thromboembolism. It’s taken twice daily, has predictable pharmacokinetics, and usually doesn’t need routine lab monitoring. While those qualities make life easier for patients, they also raise questions when a clinician plans an Invasive Procedure. The dilemma is simple: stop the drug to avoid bleeding, or keep it to prevent a dangerous clot.
Key Takeaways
- Apixaban should be stopped 24‑48 hours before most moderate‑to‑high bleeding risk procedures, longer if kidney function is impaired.
- Low‑risk procedures (e.g., dental cleaning) often allow continuation.
- Bridging with heparin is rarely needed for apixaban because of its short half‑life.
- Andexanet alfa is the specific reversal agent for emergency bleeding.
- Individual risk scores (CHA₂DS₂‑VASc, HAS‑BLED) guide how aggressively you manage anticoagulation.
How Apixaban Works and What Makes It Different
Unlike older Warfarin, which inhibits multiple clotting factors through vitamin K antagonism, apixaban targets a single step - factor Xa. This focused action gives it a rapid onset (about 3 hours) and a half‑life of roughly 12 hours in people with normal renal function. Because the drug is cleared partly by the kidneys, an eGFR below 30 mL/min can extend the half‑life to 15 hours or more, meaning you need extra time before surgery.
Why Invasive Procedures Raise Red Flags
Every cut, puncture, or instrument that breaches tissue carries a bleeding risk. The magnitude of that risk depends on the procedure’s invasiveness, the vascularity of the site, and whether a neuraxial block (spinal/epidural anesthesia) is planned. For example, a simple skin biopsy might cause only a tiny oozing, while an orthopedic joint replacement can release liters of blood. When you add a potent anticoagulant into the mix, the balance tips toward dangerous hemorrhage unless you adjust the regimen.
Assessing Patient‑Specific Risk
Two scoring systems dominate decision‑making:
- CHA₂DS₂‑VASc: predicts stroke risk in atrial fibrillation; higher scores push clinicians to avoid a gap in anticoagulation.
- HAS‑BLED: gauges bleeding tendency; a score ≥3 signals the need for extra caution.
Combine these scores with renal function, liver disease, and concomitant antiplatelet drugs (e.g., aspirin, clopidogrel). A patient with CHA₂DS₂‑VASc = 5, HAS‑BLED = 1, and eGFR = 80 mL/min will likely tolerate a short hold, whereas someone with eGFR = 25 mL/min and a recent gastrointestinal bleed may need a longer interruption.
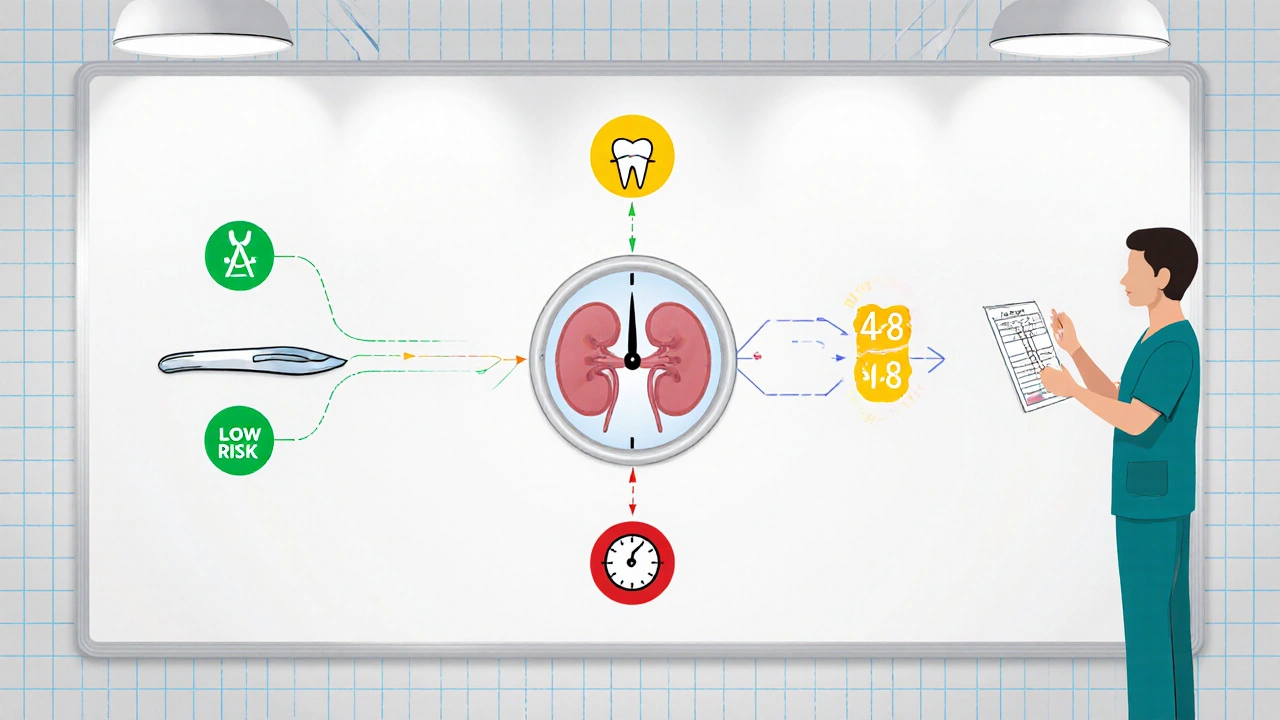
General Peri‑operative Strategies
- Determine bleeding risk category (low, moderate, high) based on the planned procedure.
- Calculate stop time:
- Low risk - continue apixaban (or hold 24 h if you prefer).
- Moderate risk - stop 24 h before (48 h if renal impairment).
- High risk - stop 48‑72 h before; extend to 96 h for eGFR < 30 mL/min.
- Bridging? Generally not needed because apixaban’s short half‑life covers the gap. Reserve low‑dose unfractionated heparin only for patients with very high thrombotic risk (recent VTE, mechanical heart valve).
- Reversal in emergencies: use Andexanet alfa for rapid factor Xa inhibition reversal. If unavailable, consider activated charcoal (if ingestion < 2 h ago) or prothrombin complex concentrate.
- Restart timing: resume 24 h after low‑risk procedures, 48-72 h after moderate risk, and 72-96 h after high‑risk or neuraxial blocks, provided hemostasis is confirmed.
Procedure‑Specific Guidance
| Procedure | Bleeding Risk | Stop Apixaban | Restart | Bridging Needed? |
|---|---|---|---|---|
| Dental cleaning, simple skin biopsy | Low | Continue (or 24 h if clinician prefers) | Immediately | No |
| Colonoscopy with polypectomy | Moderate | 24 h (48 h if eGFR < 30) | 24-48 h | No |
| Joint replacement, major abdominal surgery | High | 48-72 h (96 h if eGFR < 30) | 48-72 h | Rarely; consider low‑dose heparin only for extreme thrombotic risk |
| Spinal/epidural anesthesia | High (neuraxial bleed is catastrophic) | 72 h (extend to 96 h if renal dysfunction) | 48 h after catheter removal | No |
Reversal and Emergency Management
If a patient on apixaban bleeds heavily during or after a procedure, the first step is mechanical control - compression, surgical hemostasis, or interventional radiology. Pharmacologic reversal follows:
- Andexanet alfa binds factor Xa directly, neutralizing apixaban. Approved doses range from 400 mg bolus to a 2‑hour infusion.
- If andexanet isn’t on hand, prothrombin complex concentrate (PCC) 50 U/kg can provide partial reversal, though evidence is less robust.
- Tranexamic acid (TXA) may be added for mucosal bleeding, but it does not affect apixaban’s anticoagulant effect.
Common Pitfalls and How to Avoid Them
- Assuming all DOACs are the same. Dabigatran, rivaroxaban, and edoxaban have different half‑lives and renal clearance, so stop times vary.
- Neglecting renal function. A patient with eGFR = 25 mL/min can have a half‑life > 15 h, making a 24‑hour hold insufficient.
- Unnecessary bridging. Heparin adds bleeding risk without proven benefit for most apixaban patients.
- Resuming too early. Restarting within 12 h after a high‑risk surgery can precipitate a postoperative hematoma.
- Missing the reversal agent. Keep a protocol for andexanet alfa in the OR and the ED; delays cost lives.
Practical Checklist for the Clinician
- Verify the patient’s indication for apixaban and calculate CHA₂DS₂‑VASc and HAS‑BLED scores.
- Check latest serum creatinine; compute eGFR.
- Classify the upcoming procedure’s bleeding risk.
- Apply the stop‑time table; document the plan in the EMR.
- Order reversal agent (andexanet alfa) if the procedure is emergent or has a high bleed potential.
- Post‑procedure, reassess hemostasis before restarting apixaban.
Remember, the goal is to keep the patient safe from both clotting and bleeding. A thoughtful, individualized plan that follows evidence‑based timing usually does the trick.
Frequently Asked Questions
Can I take apixaban on the day of a dental cleaning?
For low‑risk dental work, most guidelines say you can continue apixaban. If you’re on antiplatelet therapy or have a high HAS‑BLED score, discuss a 24‑hour hold with your dentist.
Do I need to bridge with heparin before a knee replacement?
Bridging is rarely required for apixaban because the drug’s short half‑life covers the gap. Only patients with a recent venous thromboembolism (< 3 months) might benefit from low‑dose unfractionated heparin.
What if my eGFR drops to 25 mL/min?
Reduced kidney function prolongs apixaban’s half‑life. Extend the pre‑procedure hold to 48 hours for moderate‑risk surgeries and 72‑96 hours for high‑risk or neuraxial procedures.
Is there a lab test to check apixaban levels?
Standard PT/INR or aPTT aren’t reliable. Anti‑Xa assays calibrated for apixaban give the most accurate concentration, but they’re rarely needed outside research or emergency reversal.
How quickly does andexanet alfa work?
Andexanet alfa restores normal clotting within minutes after the bolus dose, with the effect lasting about two hours. A continuous infusion can maintain reversal for longer procedures.
By following these steps, you minimize both bleeding and clotting complications, keeping patients safe when surgery and anticoagulation intersect. apixaban management isn’t a one‑size‑fits‑all; it’s a balance of timing, kidney function, and the specific procedure at hand.






14 Comments
Diane Thurman
Honestly, if you’re still Googling “when can I take apixaban after surgery” you’re probably not a real clinciian, you’re just winging it.
Sarah Riley
Risk stratification via CHA₂DS₂‑VASc vs. HAS‑BLED yields a binary decision matrix; proceed accordingly.
Jai Reed
Managing apixaban around invasive procedures requires a systematic approach that balances thrombotic and hemorrhagic risks.
First, obtain an accurate eGFR to adjust the drug’s half‑life; patients with eGFR <30 mL/min need extended hold times.
Second, calculate both CHA₂DS₂‑VASc and HAS‑BLED scores to understand the urgency of anticoagulation continuation.
Third, classify the planned procedure into low, moderate, or high bleeding risk using the provided table.
For low‑risk interventions such as dental cleanings, you may keep apixaban on board or stop it for no more than 24 hours if you feel uneasy.
Moderate‑risk procedures, like colonoscopy with polypectomy, generally demand a 24‑hour cessation, extending to 48 hours when renal function is impaired.
High‑risk surgeries-including joint replacement or neuraxial anesthesia-require a 48‑ to 72‑hour interruption, or up to 96 hours if eGFR is reduced.
Bridging with unfractionated heparin should be reserved for patients who have suffered a recent VTE or possess a mechanical heart valve; otherwise it merely adds bleeding potential.
In emergency bleeding, administer Andexanet alfa promptly; its bolus and infusion restore clotting within minutes.
If Andexanet alfa is unavailable, a 50 U/kg dose of prothrombin complex concentrate offers partial reversal, though evidence is less robust.
Post‑procedure, confirm hemostasis before restarting apixaban-typically 24 hours after low‑risk work, 48‑72 hours after moderate, and 72‑96 hours after high‑risk cases.
Do not rely on routine PT/INR to gauge apixaban activity; an anti‑Xa assay calibrated for apixaban is the only reliable laboratory test.
Document every step of the peri‑operative plan in the electronic medical record to ensure continuity of care across teams.
Communicate clearly with the surgical and anesthesia staff about the timing of the last dose and the intended restart window.
By following this checklist you minimize both clotting and bleeding complications, delivering safe, evidence‑based care.
WILLIS jotrin
That checklist looks solid, but remember each patient’s narrative can throw a wrench in the algorithm-sometimes the “low‑risk” label feels high when you factor in frailty.
Vin Alls
Think of apixaban like a fire‑starter: you want it lit when you need it, but you better douse the flames before you’re near a dry forest of surgery.
Bret Toadabush
Wake up! Big Pharma wants you to trust these “reversal agents” while they push hidden agendas – the real cure is just staying off the meds.
Iris Joy
Great points all around! If you’re uncertain, run the numbers with your team, double‑check kidney labs, and don’t hesitate to call a hematology consult for that extra confidence.
Tammy Sinz
Precisely-apixaban’s pharmacokinetic profile (Cmax ≈ 3 h, t½ ≈ 12 h) dictates that the “fire‑starter” metaphor aligns with its rapid onset and clearance, reinforcing the need for timing precision.
Christa Wilson
Love the checklist! 🎉
John Connolly
Team, remember that clear communication of stop‑times and restart windows is the simplest yet most powerful tool we have – shout it out on rounds!
Wade Grindle
Indeed, articulating the exact cessation interval on the whiteboard eliminates ambiguity and aligns the multidisciplinary team.
Sameer Khan
From a pharmacodynamic perspective, the interplay between factor Xa inhibition and peri‑operative hemostasis necessitates a calibrated cessation interval that reflects both renal clearance and procedural invasiveness.
Michael Vandiver
Exactly sameer great point 👍 no need for extra commas just clear timing
Harini Prakash
Thanks for the thorough rundown 😊 It’s helpful to see the steps laid out so clearly.