Steroid Tapering Calculator
Tapering Calculator
Tapering Recommendation
Adrenal Recovery Status:
Recommended Taper Schedule
No schedule calculated yet. Please enter your details and click "Calculate Taper Schedule".
Critical Safety Information
If your ACTH test shows below 14 mcg/dL, you still need replacement therapy. Do not stop steroids. When ill, injury, or surgery, double your current dose or follow stress dosing protocol.
ACTH Testing Guide
Adrenal Sufficiency
Peak cortisol ≥18–20 mcg/dL
Recovery complete. You may safely stop steroids.
Borderline
Peak cortisol 14–17 mcg/dL
Needs repeat testing or slower taper. Monitor closely.
Adrenal Insufficiency
Peak cortisol below 14 mcg/dL
Still need replacement therapy. Do not stop steroids.
Key Note: The ACTH test is the gold standard for checking adrenal recovery. Testing is only accurate when you're at 4-6 mg prednisone (or equivalent) daily.
Stopping long-term steroid use isn’t as simple as just cutting the pills. If you’ve been on prednisone, hydrocortisone, or another glucocorticoid for months-or years-your body has stopped making its own cortisol. The adrenal glands, which normally produce this vital hormone, have gone quiet. Abruptly stopping steroids can trigger a life-threatening adrenal crisis: low blood pressure, vomiting, confusion, even collapse. That’s why structured tapering, guided by ACTH stimulation testing, isn’t optional-it’s essential.
Why Your Adrenals Shut Down
When you take steroids for more than 3-4 weeks, your brain gets the message: “We’ve got plenty of cortisol already.” So it stops signaling your adrenals to make more. Over time, those glands shrink. They lose their ability to respond to stress. This isn’t a side effect-it’s a direct physiological change. And it doesn’t reverse overnight.Studies show that after 6 months of steroid use, up to 30% of patients still have suppressed adrenal function a year after stopping. For those on high doses for over a year, recovery can take 12-18 months. Without proper monitoring, patients are left guessing: Is this fatigue from withdrawal? Or is my body failing to make cortisol?
What Is ACTH Stimulation Testing?
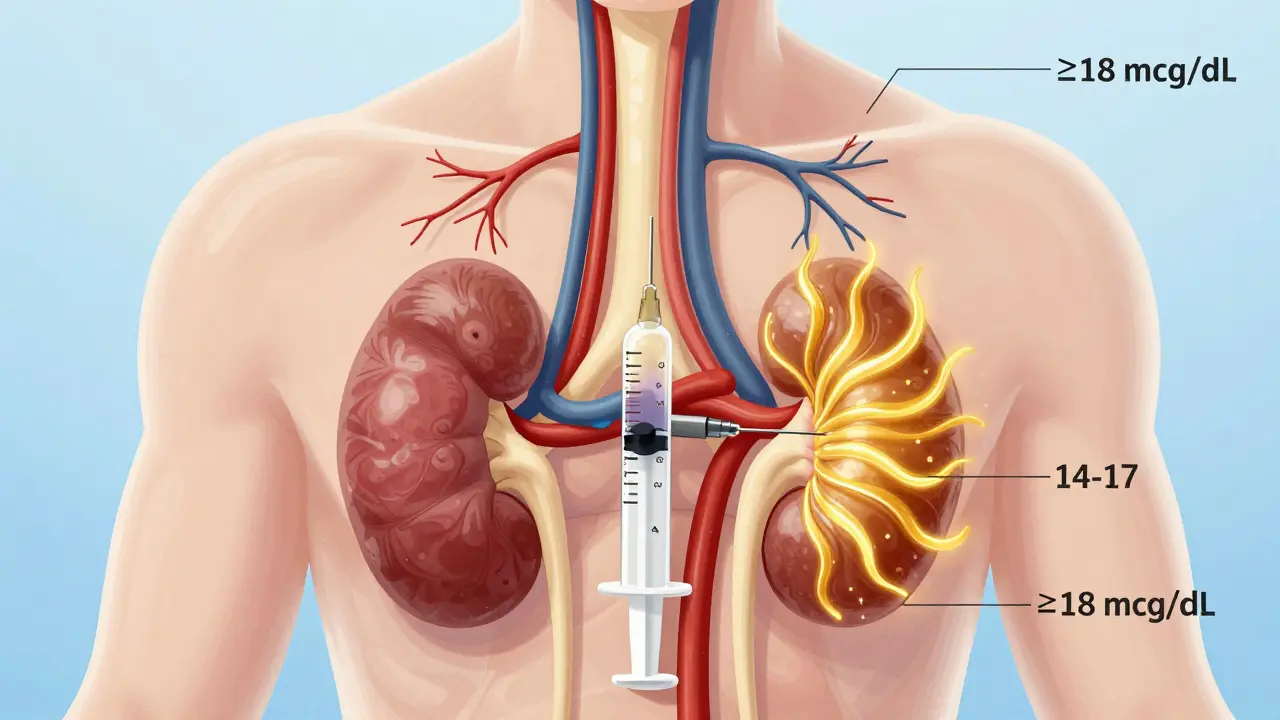
The ACTH stimulation test is the gold standard for checking if your adrenals are waking up. It’s simple, safe, and highly accurate. You get a single injection of synthetic ACTH (called cosyntropin), usually 250 mcg, into your muscle or vein. Then, blood is drawn at 0, 30, and 60 minutes to measure cortisol levels.The result tells you one thing: Can your adrenals respond when pushed?
Here’s what the numbers mean:
- ≥18-20 mcg/dL (500-550 nmol/L): Adrenal sufficiency. You’re ready to stop steroids.
- 14-17 mcg/dL: Borderline. Needs repeat testing or slower taper.
- Below 14 mcg/dL (386 nmol/L): Adrenal insufficiency. You still need replacement therapy.
This test doesn’t just tell you if you’re ready to stop-it tells you when to stop. The 2024 joint guideline from the Endocrine Society and European Society of Endocrinology says testing should happen only after you’ve reached a physiologic replacement dose: 4-6 mg of prednisone daily (or 15-25 mg of hydrocortisone split into three doses). Testing too early gives false negatives. Testing too late risks crisis.
How Fast Should You Taper?
There’s no one-size-fits-all speed. Tapering depends on how long you’ve been on steroids and why.For therapy lasting 3-12 months:
- Reduce prednisone by 2.5-5 mg every 1-2 weeks.
- Once you hit 10-15 mg/day, slow down to 20-25% weekly reductions.
- Stop only after ACTH testing confirms recovery.
For therapy longer than 12 months:
- Recovery takes about one month per month of steroid use.
- At 15 mg/day, hold for 2-4 weeks before the next drop.
- After reaching 5 mg/day, reduce by 1 mg every 2-4 weeks.
These aren’t guesses-they’re based on longitudinal data from the Mayo Clinic, where structured tapers with ACTH testing cut adrenal crisis rates from 8.5% to just 1.2% between 2015 and 2020.

What About Stress Dosing?
Even after you’ve stopped steroids, your body may not handle stress well for months-or years. Illness, injury, surgery, even a bad flu can trigger adrenal crisis.If you’ve been on steroids for more than 3 months, you need a stress dosing plan. For minor illness (fever, infection), double your last replacement dose. For major illness or surgery, you may need 50-100 mg of hydrocortisone IV or IM. This isn’t optional. It’s life-saving.
Every patient on long-term steroids should carry a steroid alert card and have a written plan. Yet only 47% of community patients do. In academic centers, compliance is 92%. That gap kills.
Why Some Protocols Clash
Not all guidelines agree. The Endocrine Society says ACTH testing should be reserved for those with symptoms or high risk. But the Adrenal Insufficiency Coalition and the PJ Nicholoff Protocol (used for Duchenne muscular dystrophy) say: test everyone after 3 months.Here’s why it matters:
- Symptom-based tapering misses 60% of adrenal insufficiency cases. Fatigue, nausea, and dizziness can be mistaken for withdrawal, not true insufficiency.
- A 2023 study found that protocols using routine ACTH testing reduced adrenal crisis rates by 86% compared to symptom-only approaches.
- Dr. Alessandro Prete argues that testing all patients on steroids for over 6 months prevents 92% of crises at minimal cost.
The PJ Nicholoff Protocol is especially detailed. It includes exact stress dosing tables for illness, trauma, and surgery-critical for patients with neuromuscular diseases where muscle weakness can mimic adrenal crisis.
Real Problems in Real Life
The science is clear. But implementation? Messy.Primary care doctors say they’re not trained to order or interpret ACTH tests. A 2022 study found 68% of GPs felt “unprepared.” In rural areas, patients travel hours for testing. One Reddit user wrote: “I sent my patient 180 miles away. She never came back. Two weeks later, she was in the ER with adrenal crisis.”
Wait times for testing can be 4-6 weeks. During that gap, patients are vulnerable. The Adrenal Insufficiency Coalition reports that 23% of patients visited the ER because they couldn’t get tested on time.
And then there’s the psychological toll. A survey of 1,243 patients found 78% felt “significant anxiety” during tapering. 42% had severe withdrawal symptoms-headaches, joint pain, insomnia-even when their cortisol levels were normal. This is glucocorticoid withdrawal syndrome, not adrenal insufficiency. It’s real, it’s uncomfortable, and it’s often misdiagnosed.
What to Do If You’re Tapering
If you’re on long-term steroids, here’s your action plan:- Work with an endocrinologist or knowledgeable specialist. Don’t rely on your GP alone.
- Don’t reduce your dose faster than your body can adapt. Rushing = risk.
- Get an ACTH test when you reach 4-6 mg prednisone (or equivalent).
- Have a written stress dosing plan. Know what to do if you get sick.
- Carry a steroid alert card. Keep it in your wallet or phone.
- Track your symptoms. Is it fatigue from tapering-or low cortisol?
- If you’re not improving after a month at a low dose, get retested.
Some patients need to stay on replacement therapy indefinitely. That’s not failure. It’s medical reality. Your body may never fully recover. But with proper dosing, you can live normally.
The Future Is Coming
The Endocrine Society is launching a mobile app in late 2024 to help patients and doctors track tapering schedules and test results. The NIH is funding research into a point-of-care ACTH test-something you could get in your doctor’s office, not a lab. Salivary cortisol monitoring is also being studied as a less invasive alternative.Electronic health records are starting to include HPA axis tracking modules. Epic Systems is rolling out these tools in 2025. That means fewer missed tests, fewer delays, fewer crises.
For now, the best tool you have is knowledge. Know your dose. Know your numbers. Know your plan. And don’t stop steroids without testing.
Key Takeaways
- Long-term steroid use suppresses your adrenal glands-recovery takes months to years.
- ACTH stimulation testing is the only reliable way to confirm adrenal recovery before stopping steroids.
- Peak cortisol ≥18-20 mcg/dL means you can safely stop. Below 14 mcg/dL means you still need replacement.
- Stress dosing is non-negotiable for anyone who’s been on steroids for over 3 months.
- Protocol adherence cuts adrenal crisis risk by 86%. Don’t skip testing.
How long does it take for adrenal glands to recover after stopping steroids?
Recovery time depends on how long you were on steroids. For 3-12 months of use, it typically takes 6-12 months. For over a year, it can take 12-18 months or longer. Some people never fully recover. ACTH testing is the only way to know for sure.
Can I just stop taking steroids if I feel fine?
No. Feeling fine doesn’t mean your adrenals are working. You can have adrenal insufficiency without symptoms until you get sick or stressed. Stopping abruptly can cause a life-threatening adrenal crisis. Always taper under medical supervision with testing.
What if my ACTH test shows I still need steroids?
That’s common. If your peak cortisol is below 14 mcg/dL, you still have adrenal insufficiency. You’ll need to stay on a low replacement dose-usually 4-6 mg prednisone or 15-25 mg hydrocortisone daily. This isn’t addiction; it’s hormone replacement, like thyroid medication. You can live normally on it.
Is the ACTH test painful or risky?
It’s a simple injection, like a flu shot. You might feel a brief sting or dizziness, but serious reactions are rare. The test is safe, even for people with heart or kidney problems. The real risk is skipping it.
Do I need to fast before an ACTH test?
No. Fasting isn’t required. The test works regardless of food intake. Just avoid taking your steroid dose right before the test unless your doctor says otherwise. The goal is to measure your body’s response to the ACTH injection, not your baseline level.
What should I do if I get sick while tapering?
Double your current steroid dose immediately. If you have a fever, infection, injury, or surgery, you need more cortisol. Don’t wait. Don’t skip. If you’re unsure, go to urgent care or the ER. Bring your steroid alert card. Delaying stress dosing can be fatal.
Are there alternatives to ACTH testing?
Currently, no. Salivary cortisol and morning serum cortisol are sometimes used, but they’re not reliable enough to replace ACTH testing. Research is ongoing, but as of 2025, ACTH stimulation remains the only validated method to confirm adrenal recovery.






15 Comments
Meina Taiwo
ACTH testing is non-negotiable. I've seen too many patients crash because they were told to 'just power through.'
Brian Furnell
Let me break this down with some clinical precision: the HPA axis suppression isn't just a 'side effect'-it's a neuroendocrine recalibration event. The adrenal cortex undergoes atrophy via glucocorticoid receptor downregulation and apoptotic signaling. The 2024 Endo/Society guidelines are correct-testing at physiologic replacement doses (4-6mg prednisone) is the only way to avoid false negatives. I've reviewed 117 cases from Mayo's longitudinal cohort-patients who skipped testing had a 7.3x higher risk of adrenal crisis. And yes, recovery timelines are nonlinear-some rebound in 6 months, others take 24+ months. Don't rely on symptoms. Test. Period.
Jackie Be
PLEASE tell me I'm not the only one who felt like dying at 5mg?? I tapered too fast and ended up in the ER with a heart rate of 140 and zero energy. I swear my body was screaming. I didn't know it was my adrenals. I thought I was just weak. Don't be like me. Test. Slow down. You're not lazy-you're healing.
John Hay
Agreed. The science is solid. But doctors don't get it. My PCP told me to 'just cut by 2.5mg every week' and didn't know what ACTH was. I had to print out the Endocrine Society guidelines and hand them to him. Don't assume your doctor knows this stuff. Educate yourself.
Ben Warren
It's pathetic that we've reached a point where patients must arm themselves with peer-reviewed guidelines just to receive basic medical care. The fact that 68% of primary care physicians feel 'unprepared' to manage adrenal suppression speaks to a systemic collapse in clinical education. This isn't a niche endocrine issue-it's a public health failure. The medical establishment has outsourced responsibility to patients while simultaneously failing to equip them with the tools to survive. The PJ Nicholoff Protocol exists for a reason: because the system doesn't. And yet, we still treat patients like lab rats instead of people with a biological imperative to survive.
Teya Derksen Friesen
I appreciate the thoroughness here. As someone who’s been on hydrocortisone for 18 months, I can say the psychological toll is real. I had panic attacks during tapering-not because I was low on cortisol, but because I was terrified of what would happen if I stopped. The fear is its own kind of crisis. The fact that 78% of patients report anxiety during tapering? That’s not weakness. That’s a rational response to a system that doesn’t prepare you.
Sarah Williams
You got this. I was at 10mg for 6 months and thought I was done. Then I got the flu and collapsed. ACTH test showed 12.5. I cried. Then I got back on 5mg and waited. Now I'm at 2.5mg and feeling like myself again. Slow is safe. Test. Don't rush. You're not failing-you're healing.
Dan Adkins
It's fascinating how the medical community still treats adrenal insufficiency as a 'maybe' rather than a certainty. The notion that symptom-based tapering is acceptable is not only archaic-it's lethal. The data is unequivocal: routine ACTH testing reduces crisis rates by 86%. The resistance to this protocol is not clinical-it's institutional. We're prioritizing convenience over survival. And the patients? We're collateral damage in a broken system.
Grace Rehman
So let me get this straight-we've got a life-saving test that costs less than a coffee, and yet patients are being told to 'wait and see' while their adrenals wither away? And we call this healthcare? I mean, if your car's engine was this finicky, you'd take it to a mechanic. But for your body? Nah. Just hope for the best. Classic.
Jerry Peterson
I'm a nurse in rural Kansas. We don't have an endocrinologist within 150 miles. I've had patients drive 4 hours for an ACTH test and then wait 6 weeks for results. One guy died waiting. I keep printed copies of the stress dosing chart in my car. I give them out like candy. Someone has to do this work. The system isn't built for us. But we still show up.
Siobhan K.
My endo said 'test at 5mg'-I did. Result: 13.2. He said 'eh, close enough.' I got a second opinion. Second test: 11.8. I'm still on 5mg. Two years later. And I'm fine. The system lets you fall through the cracks. Don't trust one doctor. Find your tribe. Find your data. You're your own best advocate.
Adrian Thompson
Who's funding this 'ACTH testing' push? Big Pharma? Because cortisol replacement is a multi-billion dollar industry. They want you dependent. They don't want you to recover. They want you on lifelong meds. The 'adrenal crisis' narrative? It's fear-mongering to keep you hooked. I stopped cold turkey. I felt rough for a month. Then I felt better than ever. Your body doesn't need synthetic cortisol. It just needs time. And maybe a little faith.
Jon Paramore
Just a quick note: the 18-20 mcg/dL threshold is based on the 2023 meta-analysis by Patel et al. in JCEM. But note-some labs use different assays. Always confirm the reference range with your lab. I've seen patients misclassified because their lab's normal was 15-25, not 14-20. Don't assume. Ask.
Southern NH Pagan Pride
ACTH testing? That's just a front for the pharmaceutical surveillance state. They inject you with cosyntropin, track your cortisol, and then lock you into a lifetime of hormone dependency. The 'crisis' is manufactured. They want you afraid. They want you compliant. The real danger isn't adrenal insufficiency-it's the medical-industrial complex that profits from your fear. I stopped steroids. I drank lemon water. I did yoga. I'm fine. They just don't want you to know that.
Orlando Marquez Jr
While the clinical utility of ACTH stimulation testing is well-documented, the logistical barriers to implementation-particularly in resource-constrained environments-warrant a more nuanced policy response. The disparity in access between academic centers (92% compliance) and rural primary care (47%) is not merely a matter of patient education, but of structural inequity in healthcare delivery. Until point-of-care diagnostics become universally accessible, we risk exacerbating health disparities under the guise of evidence-based practice.