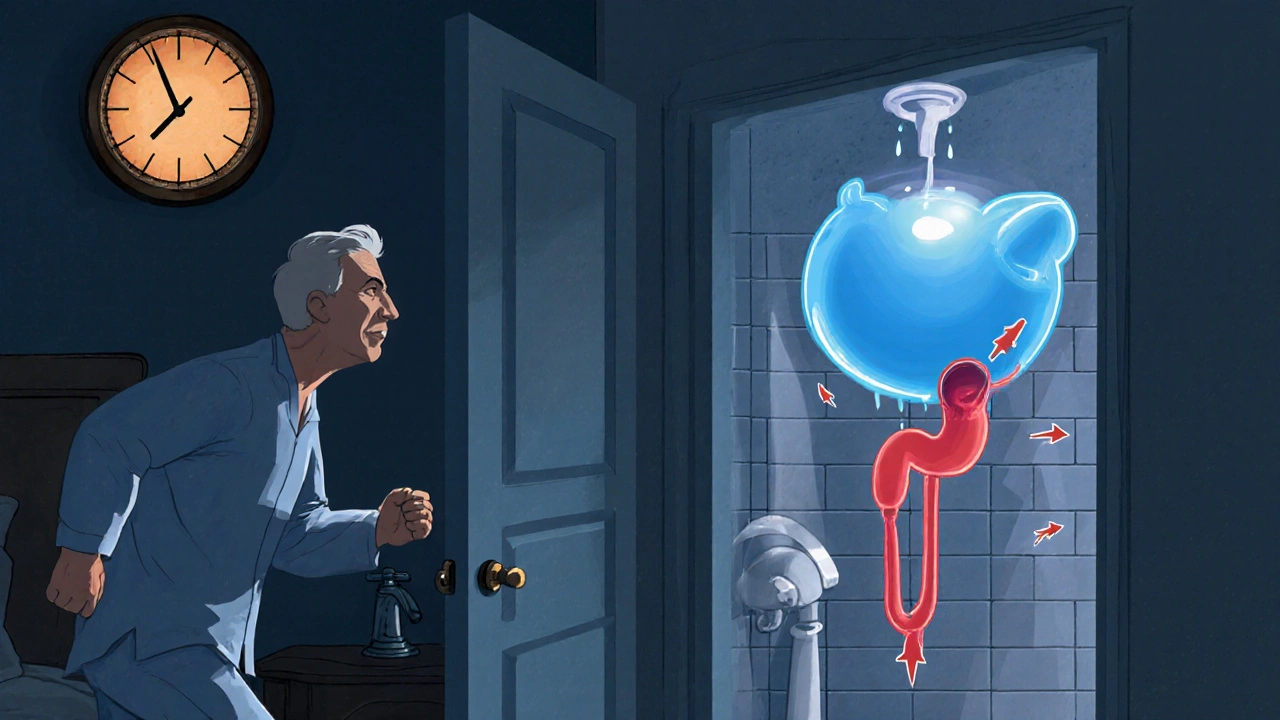
Imagine waking up multiple times at night, sprinting to the bathroom, or feeling a constant tug that you just can’t finish a pee. Those moments are more than just annoying-they could be early clues that your prostate is sending a distress signal.
What is BPH?
Benign Prostatic Hyperplasia (BPH) is a non‑cancerous enlargement of the Prostate gland. The prostate sits just below the bladder and wraps around the urethra, the tube that carries urine out of the body. As men age, the gland’s cells can multiply, making the organ larger and squeezing the urethra.
This squeeze doesn’t usually cause pain, but it does mess with urine flow. When the flow slows, the bladder works harder, leading to a whole suite of uncomfortable signals-collectively known as BPH symptoms.
Why the Urinary System Reacts
The bladder is a muscular sac that stores urine until you decide it’s time to go. If the urethra narrows, the bladder must generate higher pressure to push urine through. Over time, that pressure can weaken the bladder wall, and the nervous system may misinterpret signals, creating urgency, frequency, or incomplete emptying.
Common BPH Symptoms and What They Mean
- Urinary frequency - feeling the need to pee more than eight times a day. The bladder never feels full enough.
- Nocturia - waking up at least twice nightly to urinate. It’s a classic “middle‑of‑the‑night sprint.”
- Weak urine stream - a thin, dribbling flow that takes longer to finish.
- Urgency - a sudden, compelling need to pee that’s hard to postpone.
- Incomplete emptying - the feeling that the bladder still holds urine after you’ve finished.
- Acute urinary retention - a painful inability to start urination at all. This is an emergency.
Red‑Flag Symptoms: When to Call a Doctor Right Away
Most men can monitor mild changes at home, but some signals demand prompt medical attention. Mark any of the following as “see a doctor now”:
| Symptom | Why It’s Serious |
|---|---|
| Acute urinary retention | Bladder can’t empty; risk of damage and infection. |
| Blood in urine (hematuria) | Could indicate infection, stones, or rare cancer. |
| Persistent pain in lower abdomen or back | May signal infection or kidney involvement. |
| Fever with urinary symptoms | Signs of a urinary tract infection that needs antibiotics. |
| Sudden, severe difficulty starting a stream | Possible blockage requiring urgent decompression. |
Self‑Check: How to Track Your Symptoms
- Start a bladder diary for a week. Note the time of each void, volume (if you can estimate), and any urgency.
- Rate each void on a 1‑5 scale for stream strength and completeness.
- Count nighttime trips. Two or more is a red flag for nocturia.
- Watch for any pattern of blood, pain, or sudden retention.
- Bring the diary to your next appointment - it speeds up diagnosis.
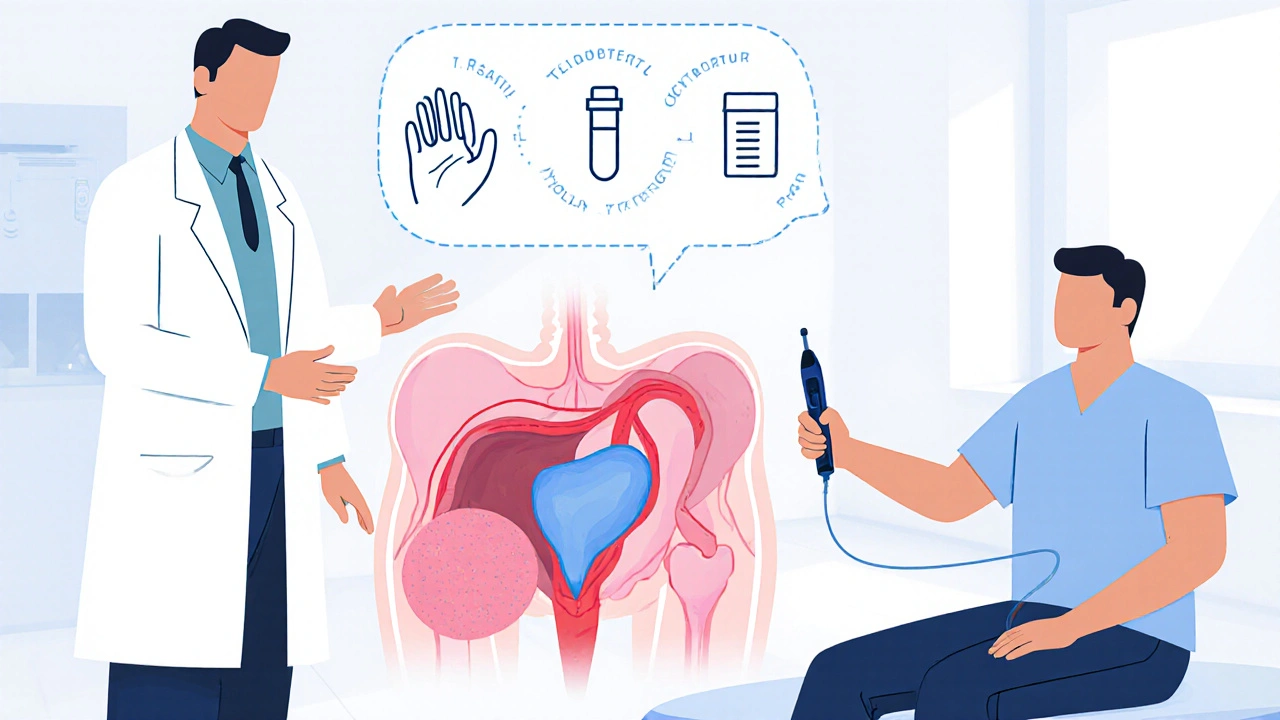
What to Expect at the Doctor’s Office
When you finally set the appointment, a Urologist will lead the assessment. Typical steps include:
- Medical history review - your diary, meds, and any related conditions such as diabetes or heart disease.
- Physical exam - a digital rectal exam (DRE) to feel the size and texture of the prostate.
- Blood test - the PSA test (prostate‑specific antigen) helps rule out cancer.
- Urinalysis - checks for infection, blood, or crystals.
- Imaging - an ultrasound or a post‑void residual scan measures how much urine remains in the bladder after you’ve voided.
Based on these results, the doctor will grade the severity (often using the International Prostate Symptom Score, or IPSS) and decide whether watchful waiting, medication, or a procedure is best.
Managing Symptoms: Lifestyle, Medicine, and Surgery
Lifestyle tweaks can ease many mild symptoms:
- Limit caffeine and alcohol, which irritate the bladder.
- Stay hydrated but avoid excessive fluids before bedtime.
- Practice timed voiding - go every 3‑4 hours even if you don’t feel the urge.
- Pelvic floor exercises (Kegels) can improve bladder control.
If tweaks aren’t enough, doctors often prescribe:
- Alpha‑blockers (e.g., tamsulosin) - relax the muscle fibers around the prostate, improving flow.
- 5‑alpha‑reductase inhibitors (e.g., finasteride) - shrink the gland over months.
For moderate‑to‑severe cases, minimally invasive procedures like transurethral microwave therapy (TUMT) or the gold‑standard transurethral resection of the prostate (TURP) can restore normal urine flow.

Quick Checklist: When to Book That Appointment
- Any episode of acute urinary retention.
- Blood in urine or persistent pain.
- More than two nightly trips to the bathroom.
- Weak stream that’s getting weaker.
- Urgency that disrupts work or sleep.
- Symptoms lasting longer than a month despite self‑care.
Remember, early evaluation not only eases discomfort but also helps rule out serious conditions like prostate cancer.
Bottom Line
Benign Prostatic Hyperplasia is a common, age‑related change, but its symptoms can range from a mild nuisance to a medical emergency. By paying attention to your bladder diary, knowing the red‑flag signs, and seeing a urologist promptly, you keep your prostate health in check and avoid unnecessary complications.
Frequently Asked Questions
Can BPH cause kidney damage?
If untreated, severe urinary retention can back up pressure into the kidneys, leading to hydronephrosis or reduced kidney function. Prompt treatment usually prevents permanent damage.
Is a urinary catheter needed for acute retention?
Yes. A temporary Foley catheter is often placed to drain the bladder immediately, followed by a plan for definitive treatment (medication or surgery).
Do all men with an enlarged prostate need surgery?
No. Many men manage symptoms with lifestyle changes and medication. Surgery is reserved for those with moderate‑to‑severe symptoms that don’t improve with other measures.
How often should I get a PSA test if I have BPH?
Guidelines vary, but most urologists recommend annual PSA testing for men over 50, or earlier if you have a family history of prostate cancer.
Can BPH symptoms improve on their own?
Mild symptoms can fluctuate, but the underlying gland enlargement usually progresses slowly. Regular monitoring helps catch worsening early.

15 Comments
Fabian Märkl
Sticking to a bladder diary can really save you a lot of hassle later!
Avril Harrison
Keeping coffee and alcohol intake low can make a noticeable difference in nocturnal trips.
I’ve found that setting a regular bathroom schedule, even when you don’t feel an urgent need, helps the bladder train itself.
Staying hydrated throughout the day but cutting back an hour before bedtime prevents that middle‑of‑the‑night sprint.
Pelvic floor exercises aren’t just for women; men can benefit from Kegels too.
If you’re tracking your symptoms, note any changes in stream strength alongside frequency.
These small adjustments often delay the need for medication.
Natala Storczyk
Listen up, gentlemen, the prostate does NOT wait for your schedule!
It expands like a ticking time bomb, squeezing the urethra and turning a simple pee into an ordeal!
You wake up at 2 a.m., dash to the bathroom, and still feel like you haven’t emptied a drop!
That pressure builds, and if you ignore it, you’re flirting with acute retention, which is a medical emergency!
Blood in the urine is not just a scare‑tactic; it can signal infection or worse!
Don’t think you’re invincible-your kidneys can suffer from back‑pressure damage!
Getting a PSA test yearly is a smart move, not a needless hassle!
Act now, schedule that urologist visit, and shut down the nightmare before it hijacks your life!!
nitish sharma
The pathophysiology of BPH involves hyperplastic growth of both stromal and epithelial elements within the prostate.
Consequently, the urethral lumen narrows, necessitating increased detrusor pressure for voiding.
Patients commonly report nocturia, weak stream, and a sensation of incomplete bladder emptying.
A thorough clinical evaluation includes digital rectal examination, serum PSA measurement, and post‑void residual volume assessment.
Therapeutic options range from watchful waiting and α‑blockers to 5‑α‑reductase inhibitors and minimally invasive surgeries such as TURP.
Timely intervention can prevent progression to bladder decompensation and preserve renal function.
Nhasala Joshi
Yo, the whole BPH thing is basically a chronic obstructive uropathy that creeps up as you age.
Your bladder’s detrusor muscle gets over‑worked, leading to hypertrophy and eventual dysrhythmia.
If you start seeing hematuria or persistent dysuria, think of underlying infection or calculi 🧪.
Keep a meticulous voiding log; data trends can flag when the IPSS score creeps into the moderate zone.
And remember, the media loves to oversimplify, but the reality involves nuanced hormonal interplay, especially DHT.
Stay vigilant and keep those check‑ups on schedule, or the system will back‑fire 🚨.
Lyle Mills
Your points on fluid timing are spot on.
In practice, I see patients adhere to a 2‑hour buffer before sleep, which reduces nocturia significantly.
Additionally, behavioural therapy like timed voiding reinforces detrusor compliance.
Overall, lifestyle modulations often delay pharmacologic escalation.
Barbara Grzegorzewska
Honestly, your suggestion sounds like a textbook copy‑paste-real life is messier.
People don’t just schedule pee like a train timetable, they battle cravings and social pressures.
Nis Hansen
The existential weight of a compromised urinary stream can indeed feel overwhelming.
Yet, each symptom is a data point in the broader narrative of one's health.
By interpreting these signals with rational curiosity, we empower ourselves.
Medical inquiry offers tools-alpha‑blockers, surgical options-to rewrite that narrative.
Thus, proactive consultation transforms anxiety into actionable knowledge.
Rohit Sridhar
Exactly, turning fear into facts is the best strategy!
When you break down the problem, it becomes manageable.
Take one step at a time: track, talk, treat.
Sarah Hanson
Early detection of BPH not only alleviates discomfort but also safeguards renal health.
Regular PSA screening and symptom monitoring are indispensable components of preventive care.
kendra mukhia
When you read the BPH overview, the first thing you must realize is that most men downplay the seriousness of urinary symptoms out of sheer bravado. They convince themselves that a few extra trips to the bathroom are a trivial inconvenience, when in fact these cues are harbingers of potential renal compromise. The bladder, an organ often taken for granted, begins to suffer from chronic over‑distension, leading to detrusor muscle fatigue. This fatigue translates into poor contractility, which exacerbates residual urine volumes and creates a vicious feedback loop. If left unchecked, the stagnant urine becomes a breeding ground for bacterial colonization, paving the way for recurrent urinary tract infections. Moreover, the increased intravesical pressure can retrograde into the ureters, placing undue stress on the kidneys. Such back‑pressure, over time, may manifest as hydronephrosis, a condition that, if severe, can culminate in irreversible kidney damage. The psychological toll is equally significant; nightly awakenings disrupt sleep architecture, leading to daytime fatigue and diminished productivity. You might think a cup of coffee or a late‑night soda is harmless, but caffeine acts as a diuretic and bladder irritant, aggravating urgency. Dietary choices, fluid timing, and even stress levels play pivotal roles in the symptomatology of BPH. Clinical guidelines stress the importance of a comprehensive bladder diary, yet many patients neglect this simple yet powerful tool. Without objective data, physicians are forced to rely on subjective reports, which can misguide treatment pathways. Pharmacologic therapy, such as α‑blockers, offers symptomatic relief but does not address the underlying hyperplasia. Surgical interventions like TURP are reserved for refractory cases, but they carry their own set of risks and recovery challenges. In the end, the most prudent approach is a balanced combination of lifestyle modification, vigilant monitoring, and timely medical intervention to prevent the cascade of complications.
Bethany Torkelson
Your rant reads like a lecture, but the facts are solid.
People need that harsh wake‑up call to stop ignoring their health.
Grace Hada
Aggression doesn’t replace action; schedule that appointment now.
alex montana
Wow!!! BPH symptoms can totally mess with your life??! Take notes, drink water, and see a doc ASAP!!!
Wyatt Schwindt
Monitoring symptoms early is key.
A urologist can guide appropriate treatment.