Most people don’t realize how much they’re missing until they sit in a quiet room and hear a tone they never noticed before. That’s the moment audiometry testing reveals what your ears have been hiding. It’s not just about turning up the volume on the TV. It’s about understanding exactly how much sound you’re losing-and where.
What Audiometry Testing Actually Measures
Audiometry testing isn’t a simple hearing check. It’s a precise, science-backed process that maps your ability to hear sounds across different pitches, from low rumbles to high-pitched whistles. The test measures the quietest sound you can detect at each frequency, recorded in decibels hearing level (dB HL). This isn’t just noise-it’s a personal hearing fingerprint.
The standard test covers frequencies from 250 Hz to 8,000 Hz, which includes nearly all the sounds of human speech. If you can’t hear a 3,000 Hz tone at 25 dB HL, that means you’re missing the crispness of the letter “s” or “th.” That’s why conversations get fuzzy, even when people aren’t speaking softly.
There are two main ways sound is delivered: air conduction and bone conduction. Air conduction uses earphones to send sound through your ear canal, eardrum, and middle ear bones. Bone conduction skips those parts entirely. A small device taps gently against your skull behind your ear, sending vibrations straight to your inner ear. Comparing the two tells audiologists whether the problem is in your outer/middle ear (like wax buildup or fluid) or in your inner ear or nerve (like aging or noise damage).
The Hughson-Westlake Method: How Thresholds Are Found
There’s a reason this test takes 10 to 15 minutes per ear. It’s not random. Audiologists use the modified Hughson-Westlake method, a proven technique developed in 1944 and still the gold standard today. Here’s how it works:
- The test starts at 1,000 Hz-a middle pitch-played at a clearly audible level, usually around 40 dB HL.
- Once you hear it and respond (by raising your hand or pressing a button), the volume drops by 10 dB.
- If you don’t hear it, the volume goes back up by 5 dB until you do.
- This back-and-forth continues until the audiologist finds the softest level you can hear about half the time.
This method isn’t about guessing. It’s about precision. A threshold isn’t just “the quietest you heard.” It’s the point where you respond correctly 50% of the time. That’s how you get a reliable baseline.
Testing follows a standard order: 1,000 Hz, then 500, 2,000, 4,000, 8,000, 250 Hz. Bone conduction is tested at the same frequencies. Each result is plotted on an audiogram-a graph that looks like a mountain range. The dips show where your hearing drops.
Understanding Your Audiogram: What the Lines Mean
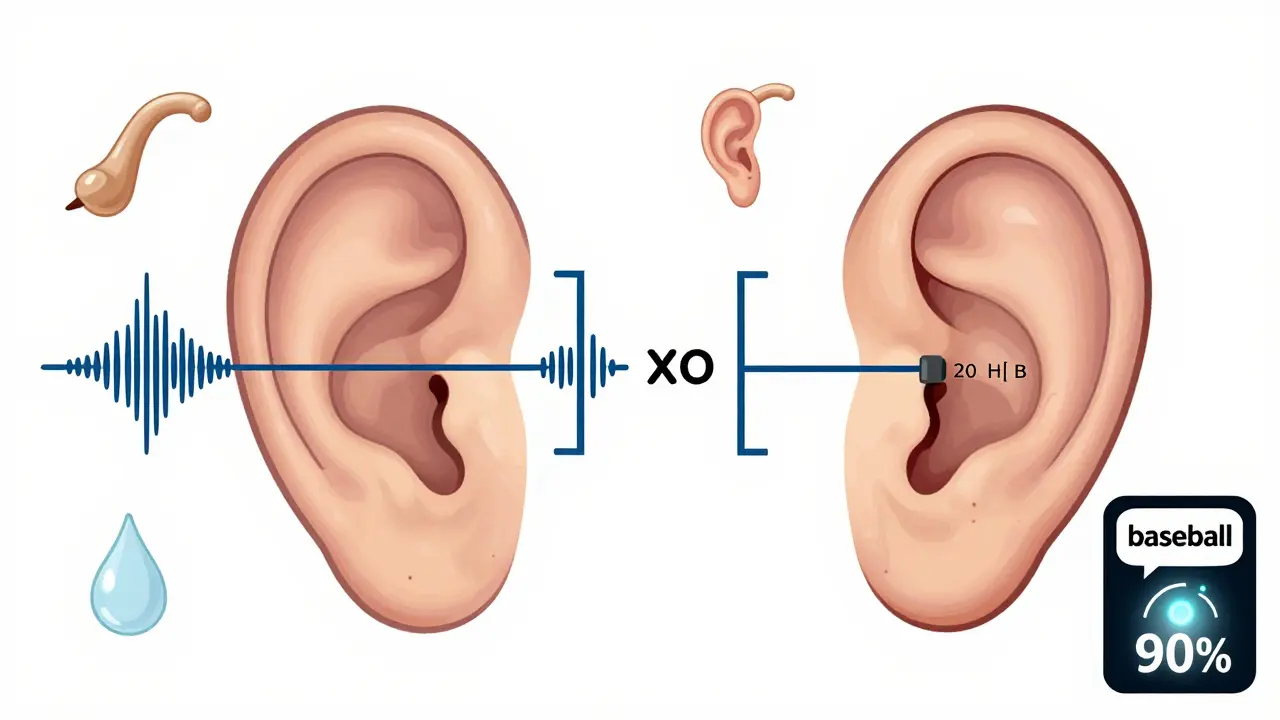
An audiogram isn’t just a chart. It’s a map of your hearing health. Symbols tell the story:
- Circles (O) = Right ear air conduction
- X’s (X) = Left ear air conduction
- Brackets [ ] = Right ear bone conduction
- < = Left ear bone conduction
If air and bone conduction lines match, your hearing loss is sensorineural-likely due to aging, noise exposure, or genetics. If air conduction is worse than bone conduction by 15 dB or more, you have a conductive hearing loss. That could mean earwax, an ear infection, or a problem with your eardrum or middle ear bones.
Normal hearing is 25 dB HL or better across all frequencies. Mild loss is 26-40 dB. Moderate is 41-55 dB. Severe is 71-90 dB. Profound is 91+ dB. If your audiogram shows a 45 dB dip at 2,000 Hz, you’re missing the clarity of speech sounds like “sh,” “f,” and “th.” That’s why you understand people fine in quiet rooms but struggle in restaurants.

Speech Testing: Why Hearing a Tone Isn’t Enough
Some people hear the beeps perfectly but still can’t follow conversations. That’s where speech audiometry comes in. Two key tests fill the gap:
- Speech Reception Threshold (SRT): This finds the quietest level you can repeat 50% of two-syllable words like “baseball” or “hotdog.” Your SRT should match your average pure-tone hearing level within ±10 dB. If it doesn’t, something’s off-maybe a nerve issue.
- Word Recognition Score (WRS): This tests how clearly you understand speech at a comfortable volume. You repeat words from a list at 25-40 dB above your threshold. A normal score is 90-100%. If you score below 70%, even hearing aids won’t fully fix the problem. That’s often a sign of retrocochlear damage-like a tumor on the auditory nerve.
One patient in Bristol told me his audiogram looked “fine,” but his word recognition was only 55%. He thought his hearing aids were broken. They weren’t. His brain couldn’t process speech clearly anymore. That’s why testing speech isn’t optional-it’s essential.
Tympanometry and ABR: The Hidden Layers
Audiometry isn’t just about tones and words. Two other tests often happen in the same visit:
- Tympanometry: A tiny probe seals your ear canal and changes the air pressure. It measures how well your eardrum moves. A flat line (Type B) means fluid is behind your eardrum-common in kids with ear infections. A normal result (Type A) means your middle ear is working right.
- Auditory Brainstem Response (ABR): Electrodes on your scalp record how your brainstem reacts to clicks or tones. This test doesn’t need you to respond. It’s used for babies, non-verbal adults, or when there’s suspicion of nerve damage. It’s the only way to know if a 6-month-old can hear without them saying a word.
These aren’t extras. They’re part of the full picture. A child with repeated ear infections might have normal hearing on pure-tone tests but still struggle in school because of fluctuating conductive loss. Tympanometry catches that. An older adult with sudden hearing loss might need an ABR to rule out an acoustic neuroma.
Who Needs Audiometry-and When
You don’t need to wait until you’re struggling to hear the TV. Here’s when testing matters:
- Newborns: CDC guidelines require all babies to be screened before leaving the hospital. If they fail, a full diagnostic test by 3 months is critical. Early intervention can prevent lifelong language delays.
- Adults over 50: Hearing loss affects half of people over 75. Annual checks after 50 catch early changes before they impact your social life.
- Noise-exposed workers: OSHA requires annual hearing tests for people in construction, manufacturing, or aviation. Noise damage is cumulative-and permanent.
- People on ototoxic drugs: Chemotherapy like cisplatin can damage hearing. Extended high-frequency testing (up to 10,000 Hz) detects early damage before it hits speech frequencies.
- Anyone with tinnitus, dizziness, or sudden hearing loss: These aren’t normal. They’re warning signs.
Many people think hearing loss is just “getting older.” But it’s not inevitable. It’s often preventable-and treatable-if caught early.
Common Misconceptions and Pitfalls
There are myths that keep people from getting tested:
- “I can hear fine-I just don’t like the way people talk.” That’s often a sign of high-frequency loss. You hear the volume but miss the consonants.
- “Retail hearing aids are enough.” Over-the-counter devices don’t diagnose. They amplify everything. Without an audiogram, you might be boosting noise you don’t need and missing the frequencies you do.
- “The test is uncomfortable.” Bone conduction can feel odd, especially if you wear glasses. But it’s not painful. Most people say it’s less awkward than they expected.
- “I’ll know when I need help.” Hearing loss creeps in slowly. You adapt. Your brain fills in the gaps. By the time you notice, you’ve been missing speech for years.
And here’s a hidden danger: masking. If one ear is much worse than the other, sound can cross over to the good ear during testing. That gives false results. Proper masking-playing white noise in the better ear-is required by ASHA standards. Not all clinics do it right.
What Happens After the Test
Audiometry isn’t the end-it’s the beginning. The results guide next steps:
- Normal hearing: Re-test in 1-3 years, depending on risk factors.
- Mild to moderate loss: Hearing aids are often recommended. Modern devices can be programmed precisely to your audiogram, boosting only the frequencies you miss.
- Severe to profound loss: Cochlear implants may be an option. These require detailed mapping based on your audiogram and ABR results.
- Conductive loss: Medical treatment may fix it-earwax removal, antibiotics, or surgery for a perforated eardrum.
Without an audiogram, hearing aids are guesswork. With one, they’re tailored to you. That’s the difference between hearing louder and hearing clearly.
Access and the Future of Audiometry
Even with all the technology, access is uneven. Rural areas have far fewer audiologists. In some parts of the UK, you might wait months for an appointment. Tele-audiology is changing that. Apps and mobile booths like KUDUwave now let you do basic screening at home. But they’re not replacements for clinical testing-especially below 25 dB HL.
AI is starting to help too. New software can analyze audiograms and flag patterns like conductive loss with 87% accuracy. But it still needs a human to confirm. Audiometry isn’t going away. It’s getting smarter.
One thing won’t change: the value of a good audiologist. They don’t just run tests. They explain what the numbers mean. They show you your audiogram. They tell you what you’re missing-and what you can still hear. That’s not just science. It’s compassion.
How long does an audiometry test take?
A full diagnostic audiometry test usually takes 30 to 45 minutes. This includes air and bone conduction testing, speech recognition, and tympanometry. Screening tests, like those in pharmacies or schools, take only 5-10 minutes but don’t give a full picture.
Is audiometry painful?
No, it’s not painful. You might feel slight pressure from the earphones or a gentle vibration from the bone oscillator, especially if you wear glasses. Some people find the bone conduction test a bit strange, but it’s not uncomfortable. There’s no poking, needles, or electric shocks.
Can I do audiometry at home?
You can take online hearing screenings, but they’re not diagnostic. They can tell you if you might have a problem, but they can’t measure your exact thresholds or differentiate between types of hearing loss. For accurate results, you need a calibrated audiometer, controlled environment, and a trained professional.
What does 25 dB HL mean in real life?
25 dB HL is the standard for normal hearing. It’s about the level of a whisper from 3 feet away, leaves rustling, or a clock ticking in a quiet room. If you can’t hear a 25 dB tone, you’re likely missing soft speech sounds like “s,” “f,” or “sh,” which makes conversations harder to follow, especially in noisy places.
Why do I need bone conduction testing if I already had air conduction?
Air conduction tests your entire hearing pathway. Bone conduction bypasses your outer and middle ear to test just your inner ear and nerve. If air conduction is worse than bone conduction by 15 dB or more, you have a conductive hearing loss-something treatable, like fluid or wax. Without bone conduction, you might miss that.
Can hearing loss be reversed after audiometry?
Sensorineural hearing loss (from aging or noise) can’t be reversed, but it can be managed with hearing aids or implants. Conductive hearing loss (from earwax, infection, or eardrum issues) often can be treated medically or surgically. Audiometry tells you which type you have-so you know what options are possible.
How often should I get my hearing tested?
If you’re under 50 and have no risk factors, every 5 years is fine. After 50, get tested every 1-3 years. If you’re exposed to loud noise regularly, have tinnitus, or take ototoxic medications, get tested annually. Early detection means better outcomes.







14 Comments
roger dalomba
Wow. A 12-page essay on beeps. Next up: how to properly hold a spoon.
At least I now know my ears are failing me... and so is my will to live.
Sophia Daniels
Oh honey, if you can't hear your own potential, you're already behind. This isn't just about decibels-it's about AMERICAN resilience. We don't whisper, we COMMAND. If your audiogram looks like a flatline, maybe you're just not trying hard enough.
And yes, I'm judging your earphones. They're probably from Target. 😏
Nikki Brown
People who ignore hearing tests are the same ones who think ‘just turn it up’ fixes everything. You’re not ‘getting older,’ you’re being lazy. And if you can’t hear your grandkids say ‘I love you’ because you refused to get screened, that’s not fate-it’s negligence.
And no, your AirPods aren’t a medical device. 🙄
Peter sullen
It is imperative to underscore that the modified Hughson-Westlake methodology remains the gold-standard psychophysical procedure for determining auditory thresholds, with a margin of error less than ±3 dB under controlled, calibrated environments.
Furthermore, the integration of tympanometric and ABR modalities constitutes a necessary triad of diagnostic validation, per ASHA 2023 clinical guidelines. Failure to adhere to this protocol constitutes a breach of audiological integrity.
Steven Destiny
You think this is about hearing? It’s about POWER. If you can’t hear the frequencies that matter-like your boss’s tone or your kid’s cry-you’re already losing. Get tested. Get loud. Get ahead.
Stop pretending it’s ‘just aging.’ It’s surrender.
sakshi nagpal
This is such a thoughtful breakdown. I work with elderly patients in Delhi, and many think hearing loss is normal. This helps me explain it better-especially the part about consonants being lost before volume.
Thank you for writing this with care.
Sandeep Jain
bro i got my hearing checked last year and my audiogram looked like a mountain range after an earthquake
turns out i just needed my ears cleaned. no hearing aids. no drama. just wax.
why do people make this so hard??
Brittany Fuhs
Anyone who uses retail hearing aids without a proper audiogram is basically giving up on their brain.
And if you think tele-audiology is the same as real testing? You’re delusional. This isn’t Amazon Prime. This is your auditory cortex.
Stop the laziness. America deserves better ears.
Fabio Raphael
I had a friend who thought her hearing was fine until she couldn’t hear her cat meow in the next room. Turns out, high-frequency loss. She cried when she heard it again through the hearing aid.
It’s not just about sound-it’s about connection.
Thank you for reminding us.
Amy Lesleighter (Wales)
hearing isn't about volume. it's about clarity.
you know how you miss the 's' in 'is'? that's your brain guessing. your ears are whispering. you just stopped listening.
get checked. it's not scary. it's just... quiet now.
Becky Baker
so like... if i can hear my dog bark but not my husband talking... is that a thing? 😅
Rajni Jain
my mom had this done last month and she was scared. but the audiologist sat with her for 20 mins just explaining the graph. she said it felt like someone finally saw her.
you’re not just testing ears. you’re listening to people.
thank you.
Natasha Sandra
my audiogram looks like a sad emoji 😔
but now i know why i keep asking ‘what?’ during family dinners.
hearing aids are kinda cute tbh. i got pink ones. 🎀
don’t wait like i did. you’re worth it.
Erwin Asilom
There is a profound psychological component to untreated hearing loss: social withdrawal, cognitive load, and increased risk of isolation. Early intervention mitigates these cascading effects.
Do not underestimate the dignity preserved by accurate diagnosis.