Every year, thousands of children in the U.S. receive the wrong dose of medication-not because a doctor made a mistake, but because the weight on file was outdated, or someone converted pounds to kilograms wrong. In pediatric care, a single decimal point error can turn a safe dose into a dangerous one. Weight-based verification isn’t just a best practice-it’s the only reliable way to stop these errors before they happen.
Why Weight Matters More in Kids
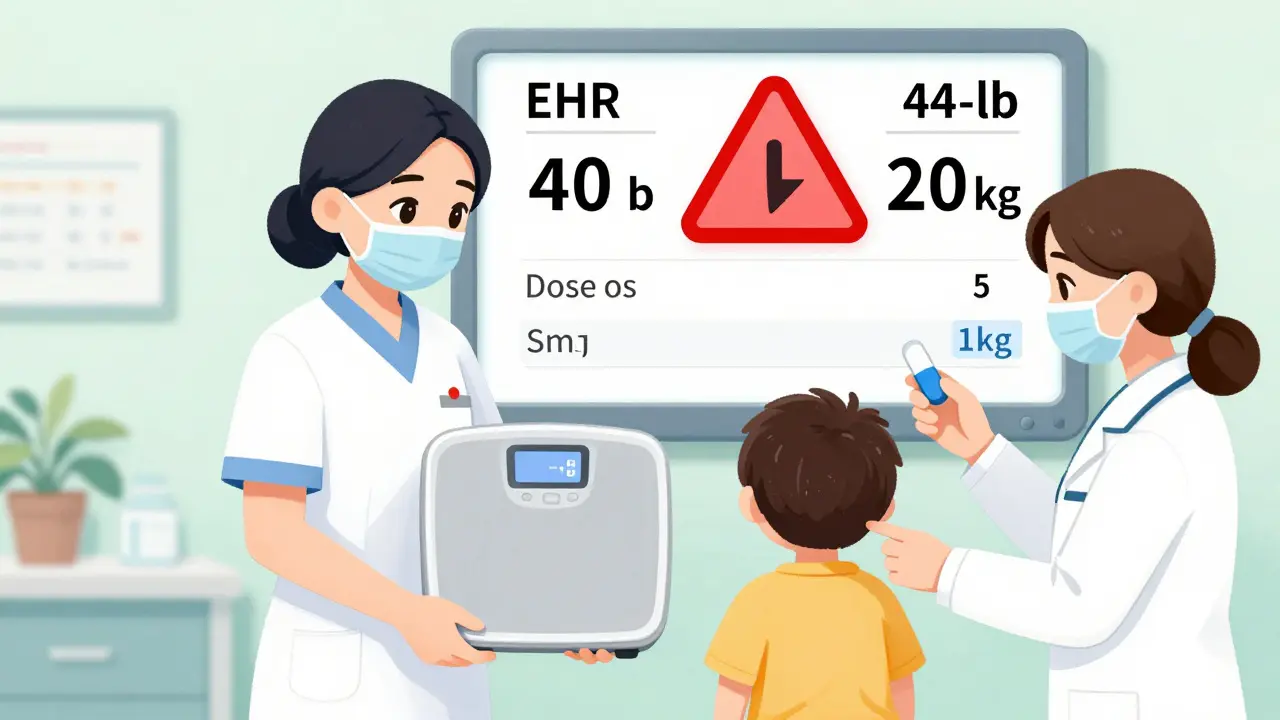
Adults often get fixed doses: one pill, one teaspoon, one injection. Kids don’t. Their bodies are smaller, their metabolism changes fast, and their dosing is almost always calculated by weight-milligrams per kilogram (mg/kg) or milligrams per square meter (mg/m²). That means if a child weighs 12 kg instead of 15 kg, and you give the same dose, you’re giving 25% too much. That’s not a small mistake. That’s a risk of seizures, organ damage, or worse. The numbers don’t lie. According to the World Health Organization, children are three times more likely to suffer a medication error than adults. And nearly one in five of those errors comes from a simple math mistake: converting pounds to kilograms. A child who weighs 44 pounds isn’t 44 kilograms. It’s 20 kg. Get that wrong, and you’re off by more than double.The Three Critical Points of Verification
Preventing these errors isn’t about one fix. It’s about three checks, done every time.- Prescription entry: When a doctor writes the order, the system must require the patient’s current weight in kilograms. No pounds. No estimates. No "I think he’s about 30 pounds." If the weight isn’t entered, the system shouldn’t let the order go through.
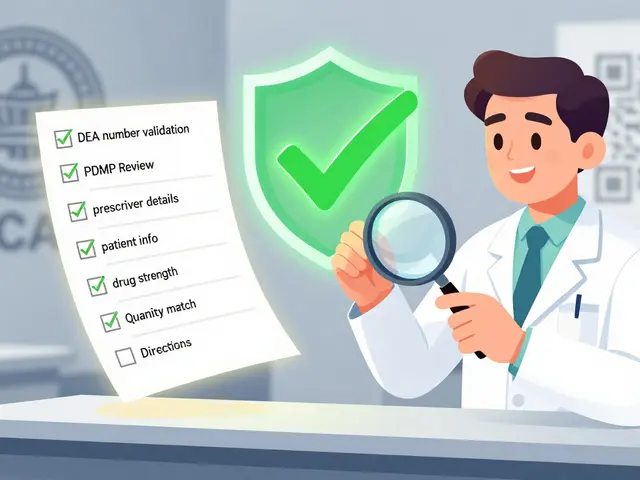
- Pharmacy verification: The pharmacist doesn’t just fill the script-they verify the math. The weight, the dose, the concentration, the volume. All of it. And they do it out loud, with a second person, if possible. In high-risk settings like ICUs, that’s non-negotiable.
- Bedside administration: Before the nurse gives the medicine, they check the weight again. Not just on the chart. On the scale. Right then. If the child’s weight has changed since admission-because they were sick, or had fluids drained, or were admitted for dehydration-the dose must be recalculated.
Technology That Actually Works
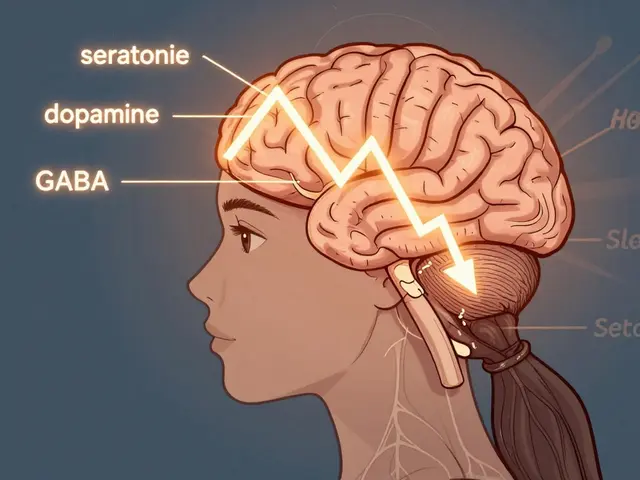
You can’t rely on people to remember every rule. Systems need to help. Electronic Health Records (EHRs) with built-in clinical decision support are the backbone of modern pediatric safety. These systems don’t just store weight-they calculate the dose automatically, flag doses that are too high or too low, and block orders that don’t match the patient’s weight range. A 2022 study in the Journal of the American Medical Informatics Association found that when these systems were properly set up, they cut dosing errors by 87.3%. But here’s the catch: they only work if they’re configured right. A system that flags every dose over 50 mg/kg for a 10-year-old might be useful for a 2-year-old-but it’s useless for a 14-year-old who weighs 50 kg. That’s why systems now use growth percentiles, not fixed numbers. Epic’s 2024 Pediatric Safety Module adjusts limits based on age and weight trends, reducing false alerts by over 60%. Barcode scanning at the bedside helps too. When the nurse scans the child’s wristband and the medication, the system checks: Is this the right drug? Is this the right dose for this weight? If not, it stops them. One study showed this cut administration errors by 74%.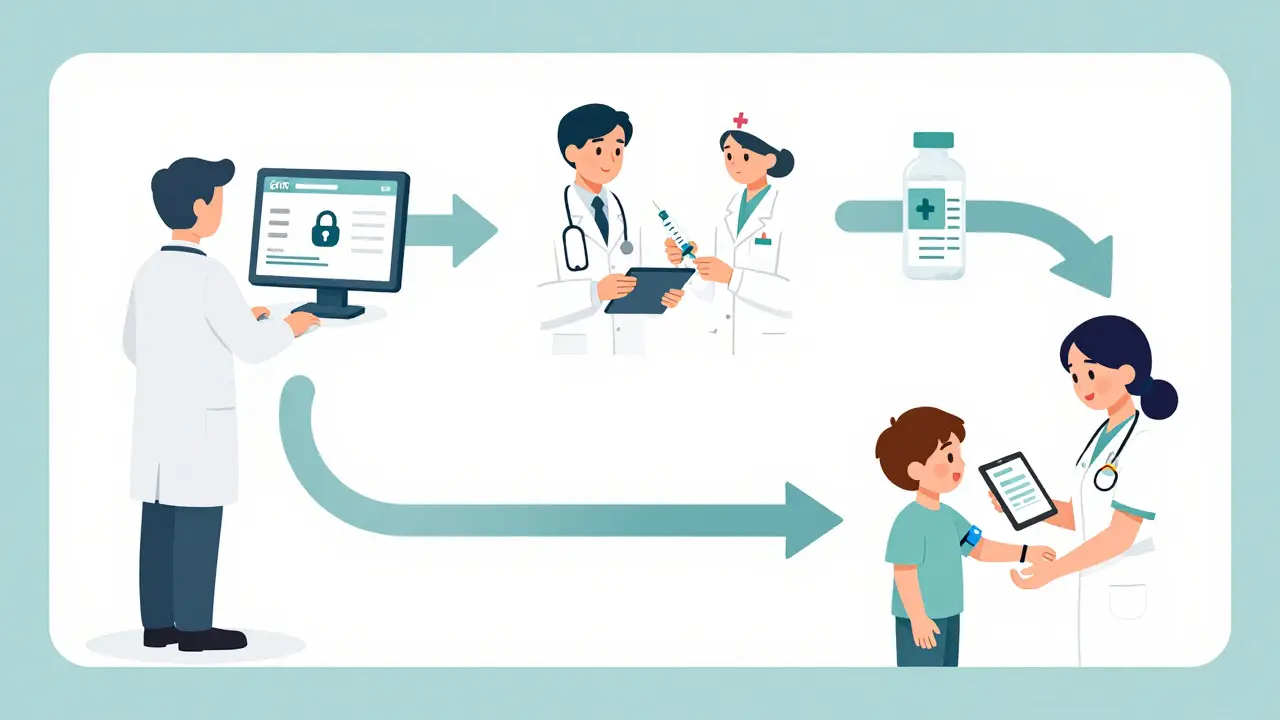
What Doesn’t Work
Not all solutions are equal. Preprinted dosing charts? Helpful in small clinics, but they fail in complex cases. Paper orders? They’re outdated. A 2019 study found standalone paper protocols only reduced errors by 36.5%-far less than computerized systems. Even the best tech fails if people ignore it. A 2021 study found that 41.7% of weight-based alerts were overridden. And in 18.3% of those overrides, the dose was actually wrong. Why? Alert fatigue. Too many warnings. Too many false alarms. A nurse who hears "Dose too high!" five times a day for no reason will stop listening. That’s why systems need to be smart. Not just loud. They need to learn. New AI tools are being tested that predict a child’s expected weight based on age, past visits, and growth patterns. If the system sees a child who weighed 14 kg last month but now shows 20 kg, it flags it-not as an alert, but as a question: "Is this correct?" That’s how you reduce noise and increase trust.Standardization Is Key
Another big source of error? Inconsistent concentrations. One pharmacy uses vancomycin at 5 mg/mL. Another uses 10 mg/mL. A nurse grabs the wrong bottle, gives the same volume-and the dose doubles. The fix? Standardize. The American Society of Health-System Pharmacists recommends using only one concentration per drug across the entire facility. For liquid antibiotics, that means 5 mg/mL for most. For pain meds, it might be 10 mg/mL. When everyone uses the same numbers, mistakes drop by 72%. Same goes for labeling. All pediatric liquids must be labeled in milliliters-not teaspoons or tablespoons. A teaspoon isn’t standardized. It can be 4 mL or 6 mL. A milliliter is always 1 mL. That’s why the American Academy of Pediatrics says: no more teaspoons. Only mL.Training and Culture
Technology can’t fix a culture that punishes mistakes. If a pharmacist gets yelled at for questioning a doctor’s order, they won’t speak up next time. Successful programs train every staff member-nurses, doctors, pharmacists, even clerks-for at least 40 hours. They don’t just learn how to use the system. They learn why it matters. They practice real cases. They role-play what to say when they see a problem. And they’re not punished for catching errors. They’re thanked. Because the goal isn’t to blame-it’s to stop the error before it reaches the child. In one rural hospital, they started a monthly "Safety Huddle" where staff shared near-misses. No names. No blame. Just: "Here’s what almost happened." Within six months, they had cut their pediatric dosing errors in half.
Who’s Falling Through the Cracks?
The biggest gap isn’t in big hospitals. It’s in small clinics and community pharmacies. A 2023 survey found that only 32.7% of rural community hospitals have full weight-based verification systems. Compare that to 94.3% of children’s hospitals. That’s not just a gap. It’s a danger zone. Community pharmacists often don’t have access to the child’s EHR. They get a paper script. The weight is scribbled in pencil: "30 lbs." They convert it. They guess. They dispense. And 28.4% of them report at least one weight-related near-miss every month. This isn’t just a tech problem. It’s a policy problem. Until every pharmacy, every clinic, every ER is required to verify weight in kilograms and use standardized concentrations, kids in underserved areas will keep being at risk.What You Can Do
If you’re a parent: Always ask for the dose in milliliters. Ask them to show you the weight on the chart. If they don’t know it, ask them to weigh your child again. If you’re a healthcare worker: Don’t assume the weight is right. Verify it. Even if it’s been done before. Even if the child looks healthy. Even if you’re busy. If you’re a hospital administrator: Don’t wait for a tragedy to act. Implement the triple-check system. Standardize concentrations. Train your staff. Budget for the pharmacists who will do the verification. It’s not a cost. It’s an investment in safety.What’s Next
The future is smarter. Wearables that track weight in real time for kids with chronic conditions. Blockchain records that lock in weight data so it can’t be changed. AI that predicts when a child’s weight is likely to change based on their illness. But the foundation won’t change. It’s still the same three checks: weight entered correctly, dose calculated correctly, dose given correctly. The tools will get better. The alerts will get smarter. But the human step-pausing, double-checking, speaking up-will always be the most important part. Because no algorithm can replace a nurse who says: "Wait. That doesn’t add up. Let me check the scale again."Why is weight in kilograms mandatory for pediatric dosing?
Weight must be in kilograms because all pediatric dosing formulas are based on metric units (mg/kg). Converting pounds to kilograms manually introduces a high risk of error-up to 12.6% of all pediatric dosing mistakes come from this step alone. Systems that require kilograms only eliminate that conversion step, reducing errors at the source. The American Society of Health-System Pharmacists and the American Academy of Pediatrics both mandate kilogram-only documentation for this reason.
Can electronic health records really prevent dosing errors?
Yes, when properly configured. EHRs with integrated clinical decision support can reduce pediatric dosing errors by up to 87.3%. These systems automatically calculate doses based on weight, flag doses outside safe ranges, and block orders if weight is missing. However, they only work if they’re customized to the facility’s protocols and if alerts aren’t so frequent they cause alert fatigue. Systems using growth percentiles instead of fixed weight thresholds have been shown to reduce false alerts by over 60%.
Why are standardized drug concentrations important?
When different departments or pharmacies use different concentrations of the same drug-for example, vancomycin at 5 mg/mL vs. 10 mg/mL-nurses can easily give the wrong volume, leading to double or half the intended dose. Standardizing concentrations across the entire facility ensures that if a nurse grabs any bottle of that drug, the concentration is the same. This simple change has been shown to reduce calculation errors by 72.4%.
How often should a child’s weight be verified?
For acute care settings, weight must be measured and documented within 24 hours of admission or any significant clinical change. For outpatient or chronic care, it should be updated every 30 days. The Institute for Safe Medication Practices warns that outdated weight is one of the top causes of dosing errors. Even a small weight change-like 1 kg in a 10 kg infant-can mean a 10% overdose if not recalculated.
What’s the biggest barrier to implementing weight-based verification?
The biggest barrier isn’t technology-it’s culture and workflow. Many providers resist systems that slow them down, even if they prevent errors. Training gaps also exist: 37.8% of pharmacy staff have inadequate knowledge of pediatric pharmacokinetics. Successful programs address this with mandatory training, leadership buy-in, and non-punitive reporting. The goal is to make safety part of the routine, not an extra step.




13 Comments
Cara Hritz
soooo i read this and like… why the hell are we still using pounds in the first place?? like my 3yo weighs 30lbs but i swear the nurse wrote 30kg on the chart once and i didnt catch it till the med was already drawn up… scary stuff
Ajay Brahmandam
Great breakdown. In India, we use kg exclusively but still see errors because nurses rush through calculations. The triple-check system works. Just need more training, not more tech.
Aliyu Sani
Man… in Lagos we dont even have reliable scales in some clinics. Weight is guessed. Dose is guessed. Kid gets sick. No one gets fired. Just another tragedy in the system.
Johnnie R. Bailey
Let’s be real - the real hero here isn’t the EHR or the barcode scanner. It’s the nurse who pauses. The one who says, ‘Wait, that doesn’t feel right.’ That’s the human algorithm no AI can replicate. Tech helps, but courage to speak up? That’s the real safety net.
Art Van Gelder
Look, I’ve worked in three different pediatric units and let me tell you - the biggest problem isn’t math, it’s momentum. Everyone’s rushing. The charge nurse is yelling about bed turnover. The pharmacist is on the phone with insurance. The nurse just wants to get the med in and move on. And somewhere in that chaos, a kid gets 25% too much vancomycin because no one stopped to ask: ‘Wait, did we even weigh him today?’ The tech is great, but if the culture doesn’t value the pause, it’s all theater.
Kiranjit Kaur
YES! This is why I push so hard in my clinic to standardize concentrations. Last month, we switched all antibiotics to 5mg/mL - no more confusion. One mom cried because her son finally got his meds right after three tries. This isn’t just policy - it’s love in action 💙
Nader Bsyouni
So we’re just supposed to trust tech that’s built by the same companies that sold us faulty airbags and opioid databases? Sure. And I’ve got a bridge in Brooklyn to sell you
Jeremy Hendriks
They say AI will fix this but what they really mean is they want to outsource responsibility. You think an algorithm cares if a 4kg preemie gets a 10mg dose? No. Only a human does. Stop pretending tech is the solution - it’s just the new scapegoat
jenny guachamboza
Also… did you know the CDC is secretly testing implants that track kids' weight in real time?? 😳 They’re calling it Project Pediatric Pulse. They’re gonna put a chip under the skin so the EHR auto-updates. I’m not joking. My cousin works in IT at NIH. This is real. 👁️🗨️
Jim Brown
The ethical imperative here transcends mere protocol. It is a moral covenant between the healer and the vulnerable - that no child shall be harmed by the negligence of a system that prioritizes efficiency over existential precision. The kilogram is not merely a unit of mass; it is the metric of human dignity. To permit pounds is to permit entropy in the sacred act of care. The triple-check is not procedure - it is liturgy.
Jamison Kissh
It’s fascinating how we treat weight like a static number when kids are dynamic. A child admitted for pneumonia might gain 1kg from fluids. A child with diarrhea might lose 2kg overnight. The system should treat weight like a live feed - not a frozen snapshot. That’s the next frontier: adaptive dosing based on real-time physiological shifts, not just yesterday’s scale reading.
Tarun Sharma
Standardized concentrations and kilogram-only entries are non-negotiable. Implementation requires leadership commitment, not just technology. Training must be mandatory and recurrent.
Gabriella da Silva Mendes
Let’s be honest - this whole thing is just a way for hospitals to get more funding from the government. They’re scared of lawsuits so they make everyone jump through hoops. Meanwhile, the real problem is that parents don’t know how to read a syringe. Teach them. Don’t make nurses do triple-checks for every 2-year-old who’s been to the ER three times this month. We’re drowning in bureaucracy, not saving kids.