Diabetic Meal Planning: What to Eat and What to Avoid for Better Blood Sugar Control
If you have diabetes, eating isn’t about restriction-it’s about balance. You don’t need to give up your favorite foods entirely, but you do need to know which ones help keep your blood sugar steady and which ones send it soaring. The goal isn’t perfection. It’s consistency. And the simplest, most effective tool for that is the Diabetes Plate Method.
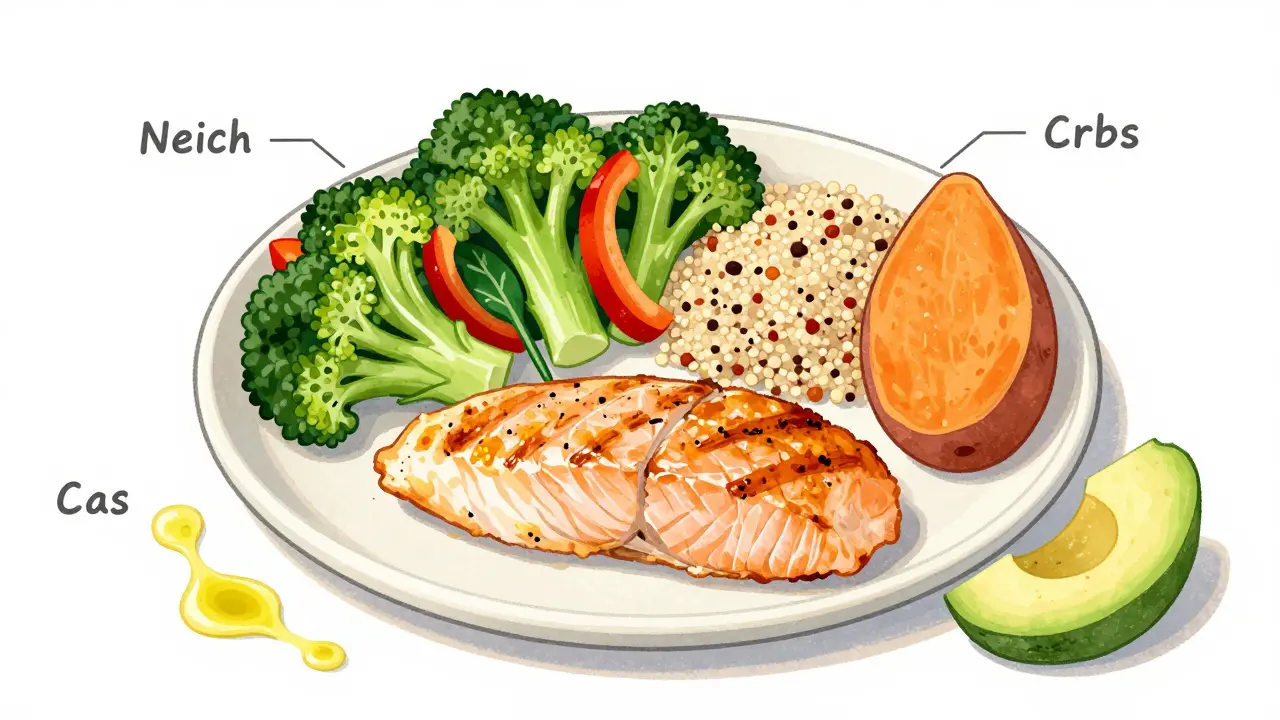
This method doesn’t require counting calories or tracking carbs with apps. You don’t need a scale or a food diary. Just grab a 9-inch plate-about the size of a standard business envelope-and divide it. Half goes to non-starchy vegetables. One-quarter to lean protein. One-quarter to healthy carbs. That’s it. The American Diabetes Association calls this the easiest way to manage blood sugar without guesswork.
What to Eat: The Building Blocks of a Diabetic-Friendly Plate
Start with the biggest part of your plate: non-starchy vegetables. These are low in carbs, high in fiber, and packed with nutrients that help your body use insulin better. Think broccoli, spinach, kale, zucchini, bell peppers, mushrooms, asparagus, green beans, and cabbage. You can eat large portions of these without worrying about spiking your blood sugar. Roast them, steam them, toss them in olive oil and garlic-there’s no wrong way to enjoy them.
Next, fill one-quarter of your plate with lean protein. This keeps you full longer and helps stabilize blood sugar after meals. Good choices include skinless chicken breast, turkey, fish (especially salmon, mackerel, and sardines for their omega-3s), tofu, eggs, and legumes like black beans and lentils. Avoid fried proteins. Instead, bake, grill, or pan-sear with olive oil. A 3-ounce portion of meat-about the size of your palm without fingers-is enough.
The final quarter? That’s where your carbs go. But not just any carbs. Choose complex, fiber-rich options like quinoa, barley, brown rice, whole-wheat pasta, sweet potatoes, and whole-grain bread. These digest slowly, so your blood sugar rises gradually instead of crashing later. Fruit belongs here too-one small apple, a cup of berries, or half a banana counts as a serving. Pair it with a handful of nuts to slow down the sugar spike even more.
Healthy fats are essential, too. They help your body absorb nutrients and keep you satisfied. Add avocado slices, a sprinkle of chia or flaxseeds, a drizzle of olive oil, or a small portion of almonds or walnuts. These aren’t empty calories-they’re blood sugar stabilizers.
What to Avoid: The Hidden Triggers That Raise Blood Sugar
Some foods might seem harmless, but they’re blood sugar landmines. Refined grains are the biggest offenders. White bread, white rice, regular pasta, and pastries are stripped of fiber and nutrients. They break down into sugar fast, causing spikes that stress your body. Swap them out. Choose whole grains instead-even if they cost a little more, they’re worth it for your long-term health.
Sugary drinks are another major problem. Soda, sweetened iced tea, fruit punch, and even 100% fruit juice can contain more sugar than a candy bar. One 12-ounce can of soda has about 39 grams of sugar-that’s almost 10 teaspoons. Water, sparkling water, unsweetened tea, or black coffee are better choices. If you want flavor, add a slice of lemon, lime, or cucumber.
Processed meats like bacon, sausage, deli ham, and hot dogs are high in sodium and preservatives. Studies link them to increased insulin resistance and heart disease risk. Opt for fresh, unprocessed meats instead. Same goes for high-fat dairy. Full-fat cheese, cream, and whole milk add unnecessary saturated fat. Choose low-fat or non-fat versions-but always check the label. Some “non-fat” yogurts make up for taste with added sugar. Look for plain versions and sweeten them yourself with a few berries.
Don’t forget sweets. Candy, cookies, cakes, pastries, and sweetened cereals have little to no nutritional value. They’re pure sugar, fast-acting and hard to control. If you crave something sweet, try a small piece of dark chocolate (70% cocoa or higher) or a few bites of fruit. Your body will thank you.
Timing Matters: When You Eat Is Just as Important as What You Eat
It’s not just about what’s on your plate-it’s about when you eat. Skipping meals can cause your blood sugar to drop too low, then rebound too high. Eating at regular times helps your body predict when it needs insulin. Aim for three meals a day with snacks if needed. Give your body two to three hours between meals to let blood sugar settle.
For people with Type 2 diabetes, spreading carbs evenly throughout the day works better than loading them into one big meal. A large dinner might cause your morning blood sugar to climb. A balanced breakfast, lunch, and dinner keeps things steady. If you’re active, a small snack before or after exercise can prevent lows.
Children with Type 2 diabetes often need three meals and three snacks daily to support growth. Their meals should be nutrient-dense and portion-controlled. The goal isn’t weight loss alone-it’s steady energy and healthy development.
Real Meals, Real Life: Sample Plates That Work
Here’s what a day of balanced eating looks like:
- Breakfast: Scrambled eggs with spinach and tomatoes, one slice of whole-grain toast, half an avocado.
- Lunch: Grilled chicken salad with mixed greens, cucumbers, bell peppers, chickpeas, and olive oil vinaigrette, plus one small apple.
- Dinner: Baked salmon, roasted broccoli and carrots, ½ cup cooked quinoa, side of mixed berries.
- Snack (optional): A handful of almonds or a small Greek yogurt (unsweetened) with a sprinkle of cinnamon.
Or try this: Southwest-style turkey meatloaf with mashed red potatoes and a side salad with orange slices. That’s protein, complex carb, and non-starchy veg-all on one plate. The Diabetes Food Hub offers free, downloadable meal plans like this one, with recipes you can drag and drop into your own weekly schedule.

What About Diets? Keto, Mediterranean, Intermittent Fasting?
You’ve probably heard of low-carb diets, the Mediterranean plan, or intermittent fasting. The truth? There’s no single best diet for everyone with diabetes. The American Diabetes Association says the best plan is the one you can stick to.
The Mediterranean diet-rich in vegetables, fish, olive oil, nuts, and whole grains-is backed by strong evidence for heart health and blood sugar control. Many people find it sustainable because it’s not restrictive. Low-carb diets can work well for some, especially if they’ve struggled with insulin resistance. But they’re not for everyone, especially if you’re on certain medications.
Intermittent fasting-like eating only during an 8-hour window-has shown promise in small studies for improving insulin sensitivity. But it’s not recommended for everyone, especially older adults or those with a history of low blood sugar. Always talk to your doctor before making big changes.
The bottom line? Stick with what’s simple. The plate method works because it’s visual, flexible, and doesn’t require perfection. You can adapt it to any culture, budget, or lifestyle.
Barriers Are Real-But Not Impossible
Not everyone has access to fresh vegetables or affordable lean protein. Food insecurity affects about 23% of adults with diabetes in the U.S. That’s not a personal failure-it’s a system problem. If you’re struggling to afford healthy food, reach out to local food banks, community gardens, or nutrition programs. Many offer free diabetic meal kits or cooking classes.
Eating out? It’s doable. Ask for extra vegetables instead of fries. Choose grilled over fried. Skip the bread basket. Order dressings on the side. Most restaurants will accommodate if you ask.
And don’t let guilt creep in. One meal won’t ruin your progress. What matters is the pattern over weeks and months. Studies show that people who stick with structured eating for six months or more see HbA1c drops of 0.3% to 2.0%. That’s the difference between needing more medication and feeling in control.
Final Thought: Food Is Medicine
Diabetic meal planning isn’t about punishment. It’s about empowerment. Every bite is a chance to support your body, not fight against it. You don’t need to be a nutrition expert. You just need to know what to put on your plate-and what to leave off.
Start small. Use the plate method for one meal a day. Gradually add more vegetables, swap white rice for brown, swap soda for water. Track how you feel-not just your numbers. Do you have more energy? Are you less hungry between meals? That’s progress.
And remember: you’re not alone. Millions of people are doing this every day. With the right tools, the right mindset, and a little patience, you can eat well, feel well, and take real control of your health.
Can I still eat fruit if I have diabetes?
Yes, absolutely. Fruit is full of fiber, vitamins, and antioxidants. The key is portion control and pairing it with protein or fat to slow sugar absorption. One small apple, a cup of berries, or half a banana is a good serving. Avoid fruit juices-they’re concentrated sugar without the fiber. Choose whole fruit instead.
Is the keto diet safe for people with diabetes?
Some people with Type 2 diabetes see improved blood sugar control on a low-carb or keto diet. But it’s not for everyone. It can increase the risk of low blood sugar if you’re on insulin or certain pills. It may also raise LDL cholesterol in some people. Always talk to your doctor or a registered dietitian before starting any extreme diet. The plate method is safer and easier to maintain long-term.
Do I need to count carbs?
Not necessarily. The Diabetes Plate Method helps you manage carbs without counting. Half your plate is non-starchy veggies (almost no carbs), one-quarter is lean protein (no carbs), and one-quarter is healthy carbs. That gives you a natural balance. If you’re on insulin or need tighter control, carb counting may help-but it’s not required for most people.
Are artificial sweeteners safe for diabetes?
Most artificial sweeteners like stevia, sucralose, and aspartame don’t raise blood sugar. They’re safe in moderation. But be careful with products that use them-like sugar-free sodas or yogurts. They may still contain other ingredients that spike blood sugar, like refined carbs or added fats. Always check the label. Water or unsweetened tea is still the best choice.
How long does it take to see results from diabetic meal planning?
Some people notice better energy and fewer cravings within a week. Blood sugar levels often improve in 2-4 weeks. For measurable changes in HbA1c (your 3-month average), it usually takes 3-6 months of consistent eating. The biggest improvements happen when people stick with the plan for six months or longer. Patience and consistency matter more than perfection.






8 Comments
kabir das
Oh my GOD, I’ve been doing this wrong my whole life!!! Half plate veggies??? I thought I was being healthy eating my 3 slices of toast with jam and a side of bacon!!! I’m crying. I’m literally crying. Tears. Tears. Tears. And also, why is everyone so calm about this?? Like, this is LIFE-CHANGING. I’m telling my mom. I’m telling my boss. I’m telling my dog. I’m telling the mailman. I’m telling the guy who sells me samosas. He’s gonna cry too.
Laura Arnal
This is SO GOOD 😊 I’ve been using the plate method for 6 months and my A1c dropped from 8.2 to 6.1!! No meds changed, just food. Non-starchy veggies are my new BFFs 🥬❤️ I roast mine with garlic and chili flakes - it’s like dessert but actually good for me. Also, swapping soda for sparkling water + lime? Game. Changer. You got this, fam. One plate at a time 💪
Eli In
As someone who grew up eating rice with every meal in the Philippines, this made me tear up in the best way 🥹 I used to think I had to give up rice entirely - but now I just use half a cup of brown rice, pile on the bitter melon and tofu, and call it a day. My lola would’ve hated this, but my pancreas loves it. 🌏✨ The plate method isn’t about losing culture - it’s about honoring your body within it. Thank you for writing this with so much heart.
Ryan Pagan
Let’s be real - the Diabetes Plate Method is the only thing that’s ever stuck because it doesn’t treat you like a lab rat. No apps. No counting. No guilt trips. Just a goddamn plate. And yeah, white bread is a death trap disguised as comfort food. I used to eat three slices with peanut butter like it was a sport. Now? One slice of sourdough, one egg, and a mountain of sautéed kale. I feel like I’m not eating a diet - I’m eating like a human who gives a shit. Also, if you’re still drinking fruit juice, you’re basically drinking liquid candy with a side of delusion. Stop. Just stop.
Paul Adler
The clarity and evidence-based approach presented here is commendable. The emphasis on consistency over perfection aligns with longitudinal clinical outcomes observed in diabetes management. The plate method, while seemingly simplistic, leverages principles of glycemic load and satiety signaling effectively. It is particularly valuable in populations with limited health literacy or access to specialized nutritional counseling. Further research into cultural adaptations of this model would be beneficial.
DHARMAN CHELLANI
u mean like... dont eat rice? lol. bro. i eat 3 bowls a day. my sugar? fine. you guys are overthinking. its not the food. its the stress. and the meds. and the fact you all sit on your butts. also, fruit juice is fine. its natural. duh.
Kacey Yates
I tried this for a week and my blood sugar spiked after every meal. The plate method is a scam. They want you to buy organic kale and $12 quinoa so they can profit. Just take your pills and eat what you want. I did. My A1c is 6.5. Done.
ryan Sifontes
they said the same thing about low fat milk. now we know its full of sugar. they said no salt. now its fine. they said carbs are evil. now its the fat. they said vaccines. now its 5g. who do you trust? the plate? or the people who own the food companies? i eat bacon. i eat bread. i eat soda. i live. you die.