When you hear the word weight management, you might think of diets, gym memberships, or apps that track calories. But for millions of people living with obesity, it’s not about willpower-it’s about medicine. Medical weight management is a structured, science-backed approach to treating obesity as a chronic disease, not a personal failure. It’s not a quick fix. It’s a long-term plan that combines clinics, medications, and careful monitoring to help people lose weight and keep it off-while reducing their risk of diabetes, heart disease, and other serious conditions.
What Medical Weight Management Actually Means
Medical weight management isn’t just seeing a doctor and getting a prescription. It’s a full-system approach built around three pillars: clinical care, medication, and ongoing tracking. The American College of Cardiology’s 2025 guidelines define it clearly: it’s for people with a BMI of 30 or higher, or a BMI of 27 or higher if they have conditions like high blood pressure, type 2 diabetes, or sleep apnea. These aren’t arbitrary numbers. They’re based on decades of research showing that losing just 5% of your body weight can significantly lower your blood sugar, blood pressure, and cholesterol.
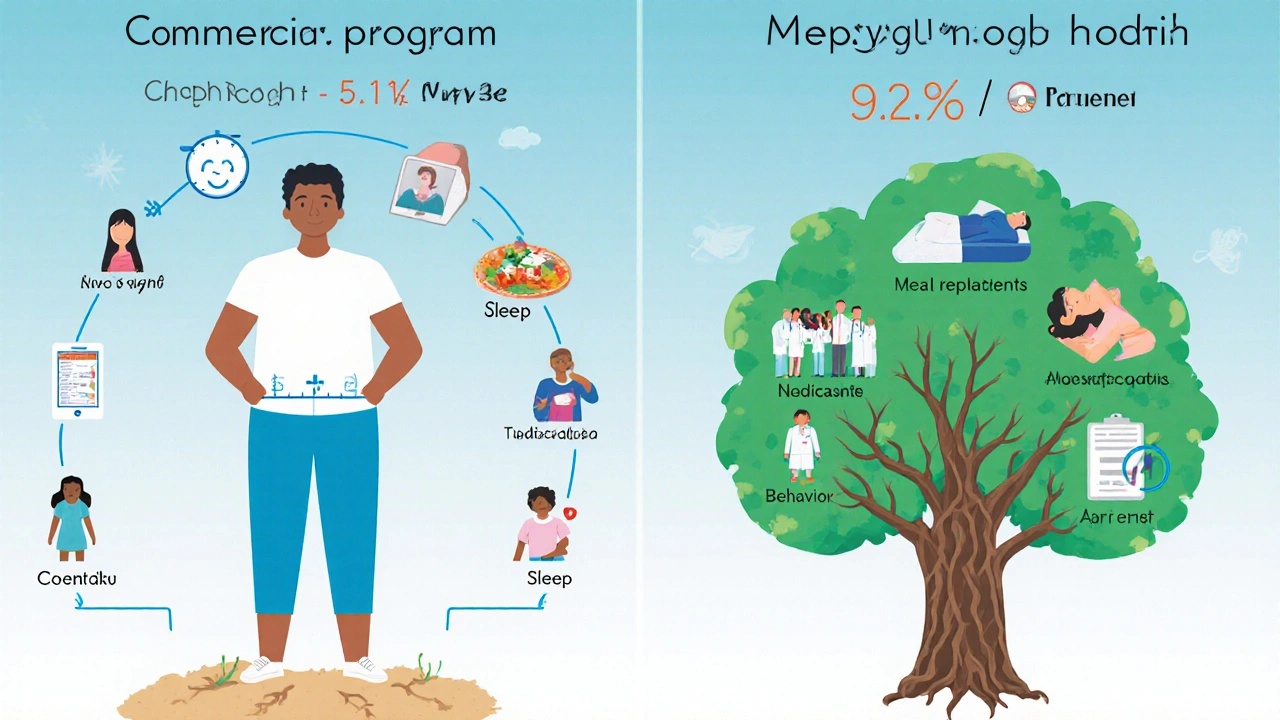
Unlike commercial weight loss programs that focus on meal replacements or group coaching, medical weight management is led by trained professionals-doctors, dietitians, behavioral therapists-who work together to create a personalized plan. The goal isn’t just to lose weight. It’s to improve your health. Studies show that people in these programs lose nearly twice as much weight as those in commercial programs-9.2% versus 5.1%-after one year.
How Weight Loss Clinics Work
Not all clinics are the same. Some are part of big hospitals, others are standalone practices. But the best ones follow a clear structure. First, you’ll need to verify your BMI. Then comes an orientation-sometimes a video, sometimes a written handbook. You’ll fill out questionnaires about your eating habits, sleep, stress, and past attempts at weight loss. This isn’t just paperwork. It helps the team understand what’s really holding you back.
At West Virginia University’s program, for example, patients can’t even book their first appointment until they’ve completed these steps. Why? Because research shows that people who start with this kind of preparation are more likely to stick with the program. The clinic then assigns you a team: a physician to manage medications, a dietitian to design your meals, and a behavioral coach to help you deal with triggers like emotional eating or late-night snacking.
Appointments aren’t weekly. They’re spaced out-every 2 to 4 weeks during the active phase. Each visit lasts 15 to 60 minutes. The dietitian doesn’t give you a rigid meal plan. Instead, they help you build flexible habits: how to eat out, how to handle holidays, how to keep protein in your meals when you’re tired. The behavioral coach doesn’t judge you for slipping up. They help you figure out why it happened and how to prevent it next time.
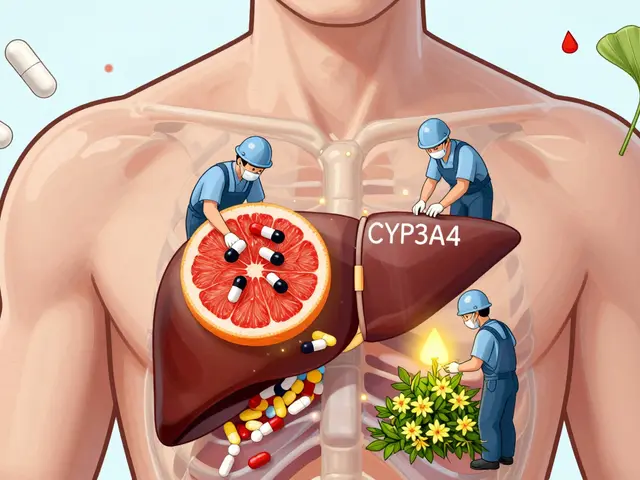
The Medications That Are Changing the Game
For years, weight loss medications were limited, ineffective, or unsafe. That changed with the arrival of GLP-1 receptor agonists. These drugs, originally developed for type 2 diabetes, turned out to be powerful weight loss tools. Two names dominate the field now: semaglutide (Wegovy®) and tirzepatide (Zepbound®).
At 72 weeks, semaglutide helped people lose an average of 14.9% of their body weight. Tirzepatide? 20.2%. That’s not just modest weight loss. That’s life-changing. For someone weighing 250 pounds, that’s 37 to 50 pounds gone. And it’s not just about appearance. Losing this much weight can put type 2 diabetes into remission, reduce heart attack risk, and improve mobility.
There’s a new player on the horizon: retatrutide. It’s a triple agonist-targeting GLP-1, GIP, and glucagon receptors-and early trials show it can lead to 24.2% weight loss in just 48 weeks. It’s not yet FDA-approved, but it’s the next big thing.
But here’s the catch: insurance coverage. Only 68% of commercial insurers cover these medications. Medicare Advantage plans? Only 12% do. That means for many people, the cost is $1,000 to $1,300 a month out of pocket. Some clinics offer payment plans. Some employers now cover it-47% of Fortune 500 companies do, up from 18% in 2022. But for many, cost remains the biggest barrier.
Why Monitoring Isn’t Optional
Weight loss isn’t linear. You’ll have good weeks and bad weeks. That’s normal. But without tracking, you won’t know what’s working. Medical weight management programs require regular monitoring-not just your weight, but your waist circumference, blood pressure, blood sugar, and sometimes even cholesterol and liver enzymes.
The American Diabetes Association recommends checking these metrics at least every 3 months during active treatment. Why? Because weight loss affects your body in real time. If your blood sugar drops too fast, your diabetes meds might need adjusting. If your blood pressure improves, you might be able to reduce or stop your pills. These aren’t side effects-they’re signs the treatment is working.
Patients who track their food, activity, and sleep using apps like MyWVUChart report higher success rates. It’s not about perfection. It’s about awareness. One patient on Reddit said the questionnaire system in their clinic helped them realize they were eating more at night because they were anxious, not hungry. That insight led to a simple change: a 10-minute walk before dinner. No extra calories. Just better habits.
Clinic vs. Commercial Programs: What’s the Real Difference?
Commercial programs like Weight Watchers, Noom, or Nutrisystem cost $20 to $60 a month. Medical clinics cost $150 to $300. At first glance, the commercial ones seem smarter. But the results tell a different story.
A 2024 JAMA study found that people in medical programs lost nearly double the weight of those in commercial programs after 12 months. And they kept it off longer. Why? Because medical programs don’t just focus on food. They address the root causes: hormonal imbalances, mental health, sleep quality, and medication needs. They also have the authority to prescribe drugs that commercial programs can’t.
Plus, medical clinics follow strict protocols. They document everything in your electronic health record. They coordinate with your primary care doctor. They don’t disappear after you hit your goal. They help you maintain. Commercial programs often fade out after 6 months.
That said, if you have mild weight concerns and no major health conditions, a commercial program might be a good starting point. But if you have a BMI over 30, or if you’ve tried and failed multiple times, medical weight management is the only approach proven to deliver lasting results.

Who Gets Left Behind-and Why
Despite all the progress, medical weight management isn’t equally accessible. Black and Hispanic patients are 43% less likely to be offered weight loss medications-even when they meet the same BMI and health criteria as white patients. That’s not a gap in care. It’s a gap in equity.
Part of the problem is bias. Some providers still see obesity as a lack of discipline. The ACC’s 2025 guidelines specifically warn against this. They recommend using chairs without armrests, offering blood pressure cuffs in multiple sizes, and never saying things like “you just need to eat less.”
Another barrier is geography. Most clinics are in urban areas. Rural patients often drive hours for a single appointment. Telehealth is helping, but not everywhere has reliable internet or trained providers.
And then there’s cost. Even if you have insurance, prior authorizations can delay treatment for weeks. One patient told the Obesity Action Coalition it took 8 weeks just to get approval for semaglutide. By then, motivation had faded.
What Success Really Looks Like
Success in medical weight management isn’t about hitting a magic number on the scale. It’s about feeling better. In a 2025 survey, 78% of patients said their quality of life improved after six months. The top reasons? Better sleep, more energy, less joint pain, and being able to play with their kids without getting winded.
One woman in her 50s lost 42 pounds in a year. She didn’t just lose weight-she stopped taking her diabetes meds. Her blood pressure returned to normal. She started walking her dog every morning. She told her doctor, “I didn’t know I could feel this good.”
That’s the real goal. Not a smaller size. Not a number on a chart. It’s reclaiming your health.
What Comes Next
The field is growing fast. By 2030, the U.S. obesity treatment market is expected to hit $5.1 billion. More medical schools are teaching obesity medicine-92% now, up from 36% a decade ago. More doctors are getting certified. More employers are offering it as a benefit.
The American Diabetes Association predicts that by 2030, weight management will be as routine in diabetes care as checking your HbA1c. That’s a big shift. It means doctors won’t wait for you to get sick before they talk about weight. They’ll address it early, like they do with high cholesterol or blood pressure.
And the science keeps evolving. New drugs are coming. Better monitoring tools are being developed. The focus is shifting from “lose weight” to “improve your health.” That’s the future of medical weight management.
Is medical weight management only for people with severe obesity?
No. Medical weight management is recommended for anyone with a BMI of 30 or higher, or a BMI of 27 or higher if they have conditions like high blood pressure, type 2 diabetes, or sleep apnea. Even modest weight loss-5% of your body weight-can significantly improve your health. You don’t need to be severely obese to benefit.
Are weight loss medications safe?
Yes, when prescribed and monitored by a qualified provider. GLP-1 medications like semaglutide and tirzepatide have been studied in tens of thousands of people over several years. Side effects like nausea or constipation are common at first but usually improve. Serious side effects are rare-under 0.2% in clinical trials. This is much safer than bariatric surgery, which carries a 4.7% complication rate.
How long do I need to stay on weight loss medication?
Obesity is a chronic condition, and like hypertension or diabetes, it often requires ongoing treatment. Stopping the medication usually leads to weight regain. Many people stay on it long-term, especially if they’re seeing health benefits. Your provider will monitor your progress and adjust your plan as needed. The goal is to keep your weight stable and your health improved.
Can I use medical weight management if I have type 2 diabetes?
Absolutely. In fact, the American Diabetes Association now lists weight management as a primary treatment goal for people with type 2 diabetes and overweight or obesity. Medications like semaglutide and tirzepatide not only help you lose weight but also improve blood sugar control-and can even lead to diabetes remission in some cases.
Why is insurance coverage so inconsistent?
Insurance companies still view obesity as a lifestyle issue rather than a medical condition. While Medicare covers behavioral therapy for obesity, it rarely covers medications. Commercial insurers cover them at only 68% rates. This is changing slowly, as more data proves these drugs reduce long-term healthcare costs. But for now, coverage varies widely by plan, employer, and state.
What if I can’t afford a medical weight management program?
Start with your primary care provider. Ask if they offer basic weight management support or can refer you to a low-cost clinic. Some academic medical centers offer sliding-scale fees. Telehealth platforms like Virta Health or Noom (with medical oversight) may be more affordable than full clinic programs. Also, check if your employer offers wellness benefits-you might be eligible for partial coverage. Even small changes in diet, activity, and sleep can make a difference while you wait for better access.


9 Comments
Deepak Mishra
This is insane!! 😱 I just spent $1200/month on Zepbound and my doc says I need to do 17 more visits??!! Who designed this system??!! 😭 I’m not rich, I’m just trying to not die from diabetes!! 🤯
John Mwalwala
Let me break this down for you in layman’s terms: GLP-1 agonists are just the tip of the iceberg. Behind the scenes, Big Pharma is colluding with the CDC and FDA to create a permanent dependency model. They don’t want you cured-they want you subscribed. Think about it: why are these drugs so expensive? Because if you stop, you gain weight back… and they profit from your relapse. It’s not medicine-it’s a subscription economy disguised as healthcare. 🕵️♂️💸
Dan Angles
While the data presented is compelling, it is imperative to acknowledge the structural inequities embedded within the current framework of medical weight management. The disparity in access-particularly among marginalized communities-is not incidental, but systemic. Furthermore, the reliance on pharmaceutical intervention without equitable infrastructure development risks exacerbating existing health disparities. A truly patient-centered model must integrate social determinants of health, not merely pharmacological ones.
David Rooksby
Okay, so let me get this straight-your doctor gives you a $1300/month shot and tells you to ‘eat less’? And you call that science? 😂 I’ve been to clinics in London and they don’t even use the word ‘obesity’ anymore-they say ‘weight-related health condition.’ The whole system is just a glorified diet cult with better PR. And don’t get me started on the insurance nightmare. I had to submit 14 forms, get rejected twice, and then my GP had to call the insurer’s ‘special obesity liaison’ who sounded like a robot trained on 1990s infomercials. This isn’t medicine. It’s a bureaucratic obstacle course with a side of semaglutide.
Melanie Taylor
My mom did this program last year and she’s now walking her dog every morning and dancing at my sister’s wedding!! 🎉💃 She cried when she said she felt like herself again-not the ‘fat lady’ she’d been told she was for 30 years. 🥹❤️ I wish more people understood this isn’t about vanity-it’s about dignity. And yes, the cost is brutal… but if your insurance won’t cover it, ask your hospital for financial aid. They have programs! Don’t give up!! 💪
Teresa Smith
Obesity is not a moral failing. It is a complex, neuroendocrine, multifactorial disease. The persistent cultural narrative that equates weight with willpower is not only scientifically inaccurate-it is actively harmful. Medical weight management represents the first legitimate paradigm shift in decades: treating the biology, not blaming the patient. Those who dismiss it as ‘just another diet’ are either misinformed or willfully ignorant. The data is unequivocal. The question is not whether this works-it’s whether society has the collective will to make it accessible.
ZAK SCHADER
USA is getting soft. We used to just eat less and work out. Now we got rich doctors giving magic shots to people who won’t stop eating donuts. This is socialism for fat people. I worked two jobs and lost weight with a pedometer. You wanna fix obesity? Stop paying for it. Let people suffer like we did. 🇺🇸💪
Danish dan iwan Adventure
GLP-1 agonists ≠ cure. They’re pharmacological crutches. True metabolic health requires insulin sensitivity, circadian alignment, and protein leverage. No drug replaces these. Clinics are monetizing desperation. The real solution? Intermittent fasting + resistance training + sleep hygiene. Done. 🧠
Ankit Right-hand for this but 2 qty HK 21
USA spends $200B/year on obesity. India? We eat roti, walk 10km daily, and don’t need your fancy pills. This is Western medical imperialism disguised as progress. Your ‘science’ is just capitalism with a stethoscope. We don’t need your clinics. We need your arrogance to leave. 🇮🇳✌️