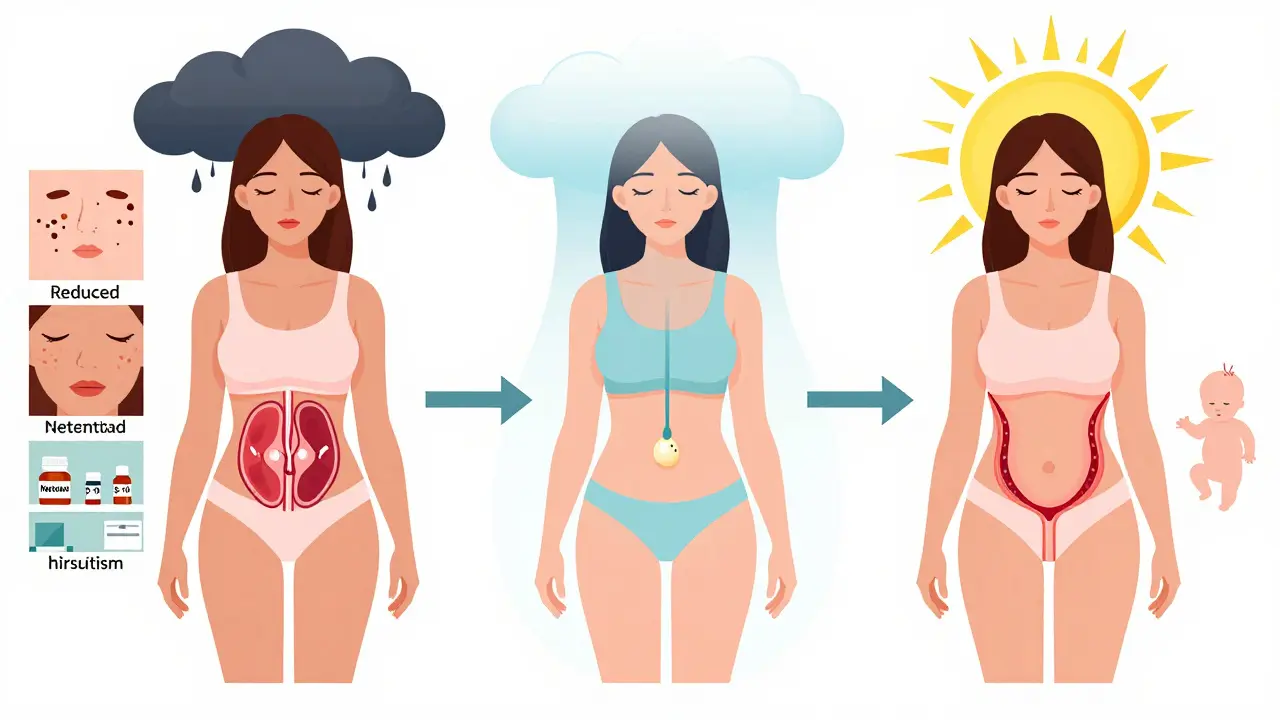
Polycystic Ovary Syndrome (PCOS) affects about 1 in 10 women of childbearing age. For many, the biggest struggle isn’t just irregular periods or acne-it’s not ovulating. And behind that ovulation problem? Often, insulin resistance. That’s where metformin comes in. It’s not a fertility drug like clomiphene or letrozole. But for women with PCOS, especially those with insulin resistance, it can be the missing piece.
What Metformin Actually Does in PCOS
Metformin was never designed to help women get pregnant. It was developed in the 1950s as a way to lower blood sugar in type 2 diabetes. But doctors noticed something strange: women with PCOS who took it for diabetes started getting regular periods-and sometimes, they got pregnant.
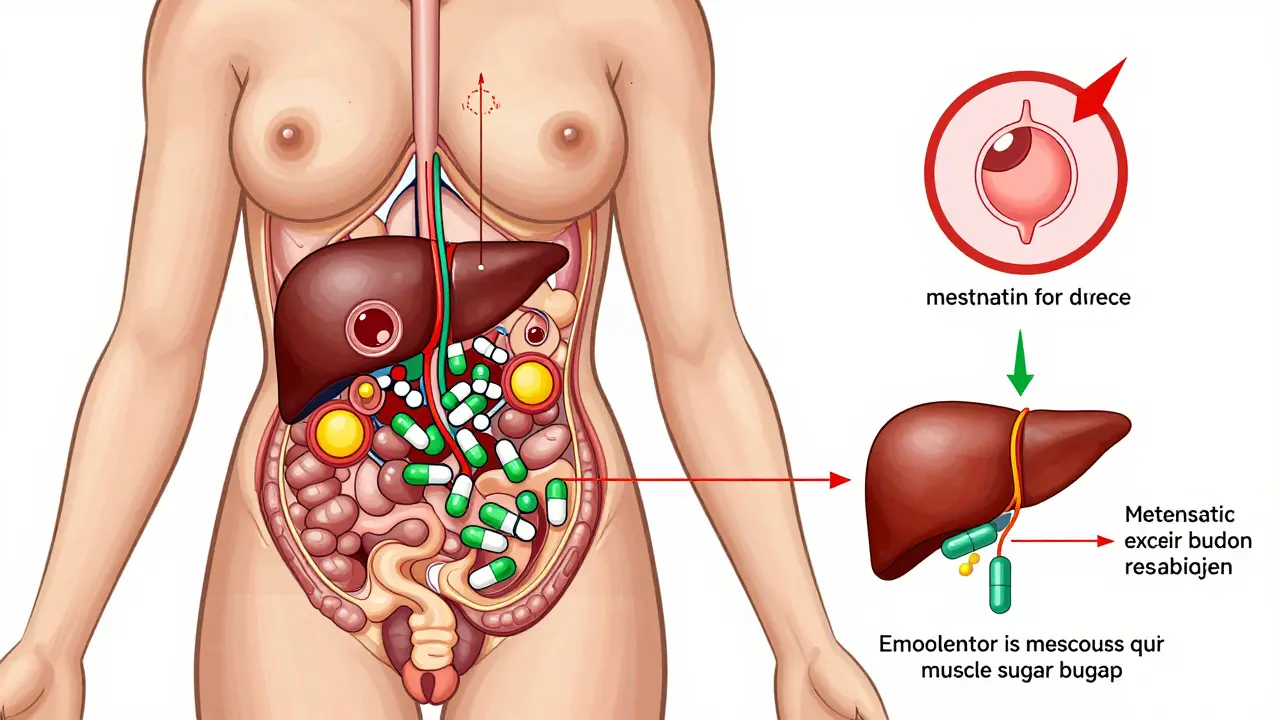
Turns out, metformin works on insulin. In PCOS, the body doesn’t respond well to insulin. The pancreas pumps out more to compensate, creating high insulin levels. That excess insulin tricks the ovaries into making too much testosterone. High testosterone = no ovulation. Metformin breaks that cycle. It reduces how much glucose the liver releases, helps muscles absorb sugar better, and even slows sugar absorption in the gut. The result? Lower insulin. Lower testosterone. A better shot at ovulation.
It’s not magic. But it’s science-backed. Studies show metformin can reduce fasting insulin by 20-30% in women with PCOS. That’s not a small change. It’s the kind of shift that can turn a 45-day cycle into a 28-day one.
Does Metformin Really Help You Ovulate?
Yes-but not for everyone.
A 2012 Cochrane review of 44 trials found women taking metformin were over twice as likely to ovulate compared to those on placebo. More recent data from 2023 confirms it: metformin improves ovulation rates in about 60-70% of women with PCOS who have insulin resistance.
But here’s the catch: if you’re not insulin resistant, metformin won’t do much. That’s why doctors now screen for it-through fasting insulin, HOMA-IR scores, or even just looking at body type. Women with PCOS who are lean but still have high insulin levels? They often respond best. Women with PCOS who are overweight? Metformin helps, but weight loss often does more.
And while metformin alone can get you ovulating, it’s not the most effective option for pregnancy. Letrozole, a drug originally used for breast cancer, is now the first-line treatment for ovulation induction in PCOS. It works better. But metformin? It’s the backup plan-or the team player.
Metformin vs. Other Fertility Drugs
Let’s compare the big three: metformin, clomiphene, and letrozole.
| Treatment | Ovulation Rate | Live Birth Rate | OHSS Risk | Cost (Monthly) |
|---|---|---|---|---|
| Metformin alone | 60-70% | 19-37% | Very low | $4-$10 |
| Clomiphene alone | 70-80% | 25-30% | Low | $30-$50 |
| Letrozole alone | 80-85% | 27-35% | Very low | $50-$100 |
| Metformin + Clomiphene | 75-85% | 30-40% | Reduced | $34-$60 |
| Metformin + Letrozole | 85-89% | 35-45% | Lowest | $54-$110 |
See that last row? Metformin + letrozole gives the highest live birth rates and the lowest risk of ovarian hyperstimulation syndrome (OHSS)-a dangerous overreaction to fertility drugs. That’s why many clinics now start with letrozole and add metformin from day one, especially if insulin resistance is present.
Metformin alone? It’s slower. It can take 3-6 months to see regular ovulation. But it’s safer, cheaper, and helps your long-term health. If you’re not ready for aggressive fertility treatment-or you’re trying to avoid multiple pregnancies-metformin is a smart first step.
How to Take Metformin for PCOS
Most doctors start low. One 500mg tablet once a day with dinner. Why dinner? That’s when your blood sugar spikes the most, and metformin works best then. After a week or two, if you’re not sick to your stomach, you bump up to 500mg twice a day. After another week, maybe 500mg three times a day. That’s 1,500mg-the sweet spot for most women.
Some switch to the extended-release version (metformin XR). It’s pricier, but it cuts nausea and diarrhea by half. If you’ve ever had stomach cramps after taking regular metformin, XR is your friend.
Side effects? About 1 in 3 people get them at first. Bloating. Diarrhea. That weird metallic taste. Most fade after 2-4 weeks. Taking it with food helps. So does going slow. Don’t rush the dose increase. Your gut needs time to adjust.
And yes-you need to be sure you’re not pregnant before starting. Metformin is Category B, meaning no harm was seen in animal studies. But no one wants to risk anything. A negative pregnancy test is standard before you begin.
What Happens When You Get Pregnant?
This is where things get messy.
Some doctors stop metformin as soon as you get a positive test. Others keep it going through the first trimester. Why? Because insulin resistance doesn’t vanish when you’re pregnant. In fact, it gets worse. And women with PCOS are at higher risk for miscarriage, gestational diabetes, and preeclampsia.
A 2023 meta-analysis of 12 trials found women who kept taking metformin into early pregnancy had higher clinical pregnancy rates than those who stopped. No increase in birth defects. No red flags. So many reproductive endocrinologists now recommend continuing metformin until at least 12 weeks.
It’s not official policy everywhere. But if you’re on metformin and find out you’re pregnant, don’t just quit. Talk to your doctor. The data supports keeping it.
It’s Not Just About Babies
Metformin doesn’t just help you ovulate. It helps you live better.
Women with PCOS are 3-7 times more likely to develop type 2 diabetes by age 40. Metformin cuts that risk. The REPOSE trial showed it reduced diabetes incidence by nearly 50% over 3 years in high-risk women.
It also helps with acne and unwanted hair. Why? Lower insulin = lower testosterone. That means less facial hair, fewer breakouts. For women who can’t or won’t take birth control pills, metformin is the only oral medication that tackles both fertility and androgen symptoms.
And it’s cheap. In the U.S., a month’s supply of generic metformin costs between $4 and $10. Clomiphene? $30-$50. Letrozole? $50-$100. If you’re paying out of pocket, that matters.
Who Benefits Most?
Not every woman with PCOS needs metformin. But if you have:
- Irregular periods and no ovulation
- High fasting insulin or HOMA-IR score
- Normal or only mildly elevated BMI (lean PCOS)
- Acne, hirsutism, or dark patches of skin (acanthosis nigricans)
- Family history of type 2 diabetes
…then metformin is likely worth trying. Especially if you’re not ready for stronger drugs-or if you’ve tried clomiphene and it didn’t work.
And if you’re doing IVF? Metformin cuts your risk of OHSS by over 70%. That’s huge. Many clinics now give it to everyone with PCOS before starting stimulation.
What’s Next?
The debate isn’t over. Some experts say metformin should be first-line. Others say letrozole is still king. But the trend is clear: we’re moving away from one-size-fits-all treatment.
Metformin isn’t a miracle. But it’s one of the few PCOS treatments that fixes the root problem-insulin resistance-instead of just masking symptoms. It doesn’t guarantee pregnancy. But it gives your body the best chance to work the way it should.
If you have PCOS and you’re trying to conceive, ask your doctor about insulin testing. If you’re insulin resistant, metformin might be the quiet hero your treatment plan is missing.
How long does it take for metformin to help with ovulation in PCOS?
Most women start seeing more regular cycles after 2-3 months of consistent use. Ovulation typically returns between 3 and 6 months. Some need up to 8 months, especially if they start at a low dose. Patience is key-metformin works slowly but steadily on the underlying insulin resistance.
Can metformin cause weight loss in PCOS?
Yes, but modestly. On average, women lose 2-5% of their body weight over 6 months. It’s not a weight-loss drug, but by lowering insulin, it reduces fat storage and cravings. The real benefit isn’t the number on the scale-it’s improved insulin sensitivity, which helps ovulation and metabolic health.
Is metformin safe during pregnancy?
Current evidence says yes. Metformin is classified as Category B, meaning no harm was found in animal studies. Human studies show no increased risk of birth defects. Many doctors now recommend continuing metformin through the first trimester to reduce miscarriage risk and gestational diabetes in women with PCOS. Always discuss this with your OB or fertility specialist.
Does metformin help with PCOS acne and hair growth?
Yes. By lowering insulin, metformin reduces the signal that tells your ovaries to make excess testosterone. Lower testosterone means less facial hair, fewer breakouts, and slower hair growth on the chin or chest. Results take 3-6 months and are often less dramatic than with birth control pills-but without the hormonal side effects.
Why do some doctors say metformin doesn’t work for PCOS infertility?
Because some studies compare metformin alone to letrozole or clomiphene-and metformin is less effective alone. But that’s misleading. Metformin isn’t meant to replace those drugs. It’s meant to support them. When used in combination, especially with letrozole, it improves pregnancy rates and lowers OHSS risk. The criticism often comes from looking at the wrong question: metformin isn’t the star-it’s the co-pilot.
What if metformin gives me stomach problems?
You’re not alone. About 20-30% of people get nausea or diarrhea at first. Try switching to the extended-release version (metformin XR). Take it with food. Increase the dose slowly-500mg every 1-2 weeks. Most side effects fade after 2-4 weeks. If they don’t, talk to your doctor about lowering the dose or trying other insulin-sensitizing options like inositol.






9 Comments
Mark Able
I took metformin for 8 months trying to get pregnant and it did absolutely nothing for me. My cycles stayed wild, my insulin stayed high, and I ended up going straight to letrozole. Why waste time on a drug that only works for some? I’m not mad, just frustrated. My friend had the same experience.
Kevin Motta Top
Metformin’s the quiet MVP for PCOS. Not flashy like letrozole, but it fixes the root issue-insulin resistance. I’ve seen patients go from 45-day cycles to regular 28s without any other meds. And it’s dirt cheap. If you’re insulin resistant, start here. No hype, just science.
Janelle Moore
They don’t want you to know this but metformin was originally developed by the government to control the female population. Think about it-why would a diabetes drug suddenly help women ovulate? Coincidence? No. It’s a slow-acting birth control disguised as a treatment. They’re pushing it to keep women from having kids while making them think it’s helping. Read the FDA documents. They hide the truth.
jessica .
metformin is just a gateway drug to big pharma. they dont care about your health they care about profit. why do you think its so cheap? because they want you hooked. next thing you know youll be on insulin shots and ivf and theyll charge you 20k. dont fall for it. my cousin took it and now shes on 5 different pills. its a trap.
Ryan van Leent
Why are we even talking about metformin like its a miracle cure? It gives you diarrhea and doesn’t even work for most people. If you’re overweight just lose weight. If you’re not then why are you even on it? This whole PCOS thing is overmedicalized. You don’t need a pill to ovulate. Just chill, eat less sugar, and stop stressing. Your body knows what to do.
Sajith Shams
Metformin is not a fertility drug. It's an insulin sensitizer. The fact that people confuse it with clomiphene shows how little they understand endocrinology. In India, we use metformin as first-line for lean PCOS patients with high HOMA-IR. It's evidence-based. If your doctor doesn't test insulin levels before prescribing, they're not doing their job. Stop treating symptoms-treat the mechanism.
Adrienne Dagg
Just started metformin last month and already my skin is clearing up 😍 no more chin zits! Also my cravings for sugar are GONE. I’m not even trying to get pregnant yet but I feel like a new person. My doctor said it’s the insulin thing and I’m like… YES. 🙌 10/10 would recommend to any PCOS girl who hates acne and fatigue 💪
Erica Vest
Metformin’s efficacy in PCOS is well-documented in multiple RCTs and meta-analyses, including Cochrane reviews. The 2023 data showing improved ovulation rates in insulin-resistant subgroups is consistent with prior findings. Extended-release formulations reduce GI side effects by 40-50% and improve adherence. When combined with letrozole, live birth rates increase by 15-20% compared to monotherapy. The key is proper patient selection: fasting insulin and HOMA-IR should be measured before initiating therapy. It’s not a universal solution, but for the right patient, it’s a foundational intervention.
Chris Davidson
Metformin doesn't cure anything. It just masks symptoms. Real healing comes from diet and lifestyle. Why are we giving pills to women instead of teaching them how to eat? The medical system is broken. They want you dependent. I've seen women get off metformin and go keto-suddenly their cycles return. No drugs needed. Stop trusting the system. Take back your health.