When you take opioids for pain, you’re not just getting relief-you’re also stepping into a biological tightrope. These drugs work by locking onto receptors in your brain and spinal cord, quieting pain signals and sometimes giving you a wave of calm or even euphoria. That’s why they’re so effective. But that same mechanism is what makes them dangerous. Over time, your body adapts. You need more to feel the same effect. That’s tolerance. And once tolerance sets in, dependence follows. Then comes the real threat: overdose. And it doesn’t matter if you’ve been on them for weeks or years. The risk doesn’t disappear-it changes shape.
How Tolerance Builds-And Why It’s Dangerous
Tolerance isn’t just about needing a higher dose. It’s your brain rewiring itself. Every time you take an opioid, it triggers dopamine release and shuts down pain pathways. But with repeated use, your neurons start pulling back. Receptors get less responsive. Some even disappear from the cell surface. Your body starts producing more enzymes to break down the drug faster. You’re not just building a habit-you’re changing your biology.
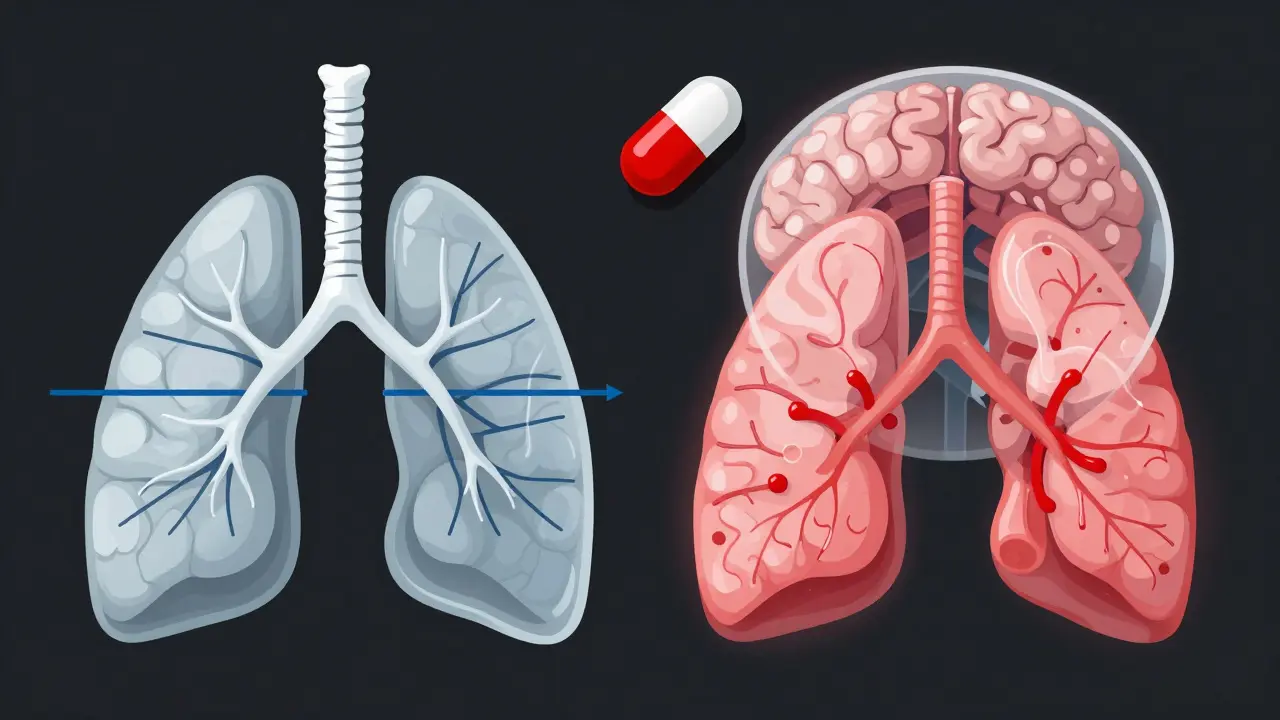
Here’s the scary part: tolerance to pain relief and euphoria develops quickly. But tolerance to respiratory depression-the kind that stops your breathing-doesn’t keep up. That’s why someone who’s been using opioids for months can still overdose. Their body learned to handle the high, but not the shutdown. A 2021 CDC report showed that 70.3% of opioid overdose deaths involved synthetic opioids like fentanyl, which is 50 to 100 times stronger than morphine. Even experienced users aren’t protected.
One study in the Journal of Pharmacology and Experimental Therapeutics found that opioid receptors block calcium channels and open potassium channels to calm nerve activity. That’s how they reduce pain. But that same action slows your breathing. When tolerance to pain fades but tolerance to breathing suppression doesn’t, you’re walking a knife’s edge.
Dependence Isn’t Addiction-But It’s Still Risky
Dependence means your body relies on the drug to function normally. Stop suddenly, and you’ll get sick: nausea, sweating, muscle aches, anxiety, insomnia. It’s not a moral failure. It’s physiology. Even people taking opioids exactly as prescribed can become dependent. The British Journal of Pharmacology confirmed in 2008 that chronic opioid use triggers a wide range of neuroadaptations-changes in brain chemistry that make stopping hard.
Dependence doesn’t always mean addiction. Addiction is when you keep using despite harm. But dependence makes addiction more likely. If you’re physically reliant on the drug to feel okay, the temptation to keep taking it-even when it’s no longer helping your pain-is powerful. A 2019 study in the Journal of Pain and Symptom Management found that 32% of patients prescribed opioids for chronic pain developed misuse behaviors within a year. That’s more than one in three.
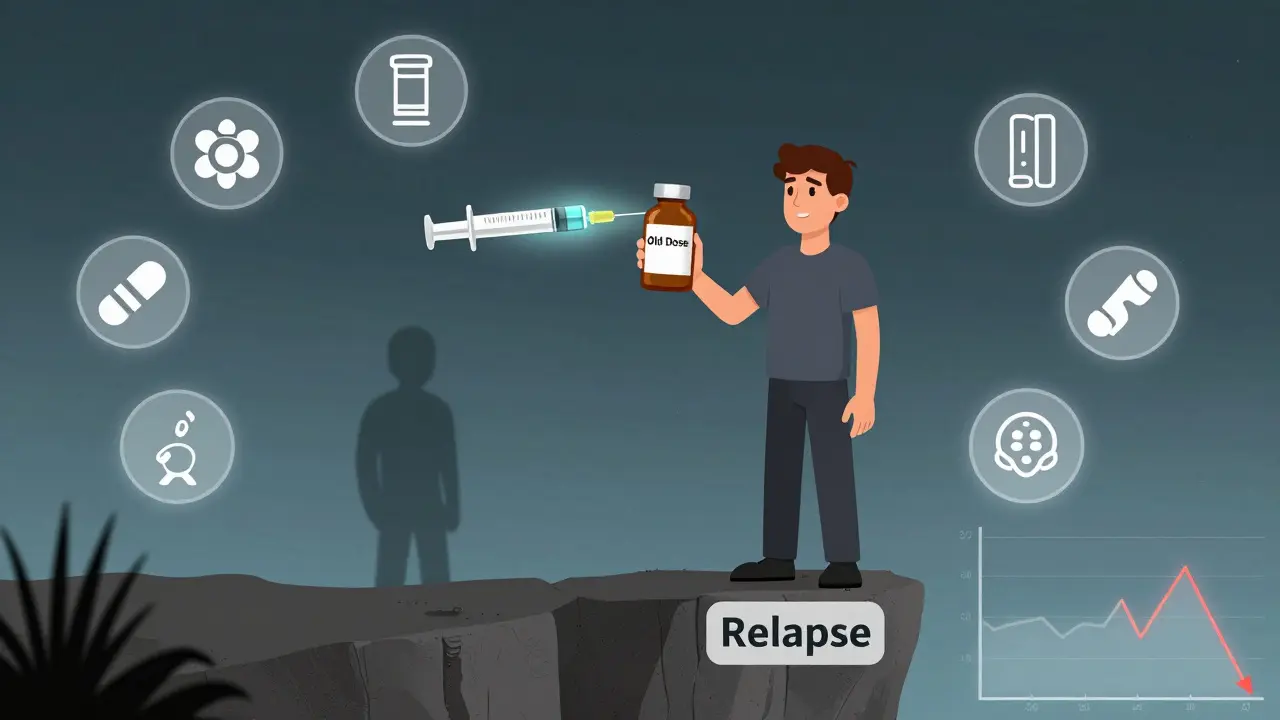
And here’s what most people don’t realize: dependence doesn’t go away after you stop. Your brain remembers. That’s why relapse is so common-and so deadly.
The Hidden Danger: Lost Tolerance and Relapse
One of the most misunderstood risks is what happens after you stop using. If you’ve been on opioids for months or years, your body adjusts. You’ve built up tolerance. Then you quit. Maybe you go to rehab. Maybe you just decide it’s time. After a few weeks or months without the drug, your tolerance drops. Your body forgets how to handle it.
That’s when relapse becomes deadly. A person who used to take 80 mg of oxycodone a day might think they can pick up where they left off. But their body can’t. They take the same dose-and their breathing stops. The Journal of Substance Abuse Treatment found that 65% of opioid overdose deaths happened in people who had previously been treated for opioid use disorder. Narcan Saves Lives reported that 87% of overdose reversals since 2018 involved people who had been clean for a while.
One Reddit user shared: “After 6 months clean, I used my old dose and nearly died-paramedics said I was clinically dead for 4 minutes.” That’s not an outlier. It’s a pattern. Your body forgets how to protect itself. And that’s why recovery programs now teach: start low. Never go back to your old dose.
Fentanyl: The Silent Killer
Most opioid deaths today aren’t from prescription pills. They’re from fentanyl. It’s cheap, potent, and often mixed into other drugs without the user’s knowledge. A single milligram can kill. The DEA saw a 1,200% increase in fentanyl seizures between 2015 and 2022. In 2021, fentanyl was involved in over 28,000 overdose deaths in the U.S. alone.
Unlike morphine or oxycodone, fentanyl hits the brain fast and hard. There’s no warning. No time to react. And because it’s so strong, even people with high tolerance can’t adjust. A person who used to take heroin might think they’re safe. But if the powder they bought was cut with fentanyl, they’re in danger.
There’s no safe way to use illicit drugs laced with fentanyl. That’s why harm reduction groups push for naloxone access and drug checking services. Naloxone can reverse an overdose-but only if it’s available when you need it.
Why Buprenorphine Is a Game Changer
Not all opioids are created equal. Buprenorphine is a partial agonist. That means it activates opioid receptors, but only partly. It gives pain relief and reduces cravings, but it doesn’t cause the same level of respiratory depression as full agonists like heroin or fentanyl.
It also has a ceiling effect. After a certain dose, taking more doesn’t increase the high-or the risk of overdose. That’s why it’s one of the safest medications for treating opioid dependence. A 2020 Cochrane Review found that medication-assisted treatment with buprenorphine or methadone cuts overdose risk by half.
In 2023, the U.S. passed the Mainstreaming Addiction Treatment (MAT) Act, removing the old ‘X-waiver’ that limited who could prescribe buprenorphine. Now, any licensed doctor can prescribe it. That’s a huge step. More access means more lives saved.
What You Can Do-If You or Someone You Know Uses Opioids
- If you’re prescribed opioids, ask your doctor: Is this the lowest effective dose? Can I try non-opioid options?
- Never mix opioids with alcohol, benzodiazepines, or sleep aids. That combination dramatically increases overdose risk.
- If you’ve been clean for a while and are thinking of using again, start with less than half your old dose. Your tolerance is gone.
- Carry naloxone. It’s safe, easy to use, and can bring someone back from the brink. Many pharmacies now sell it without a prescription.
- If you’re struggling, reach out. Medication-assisted treatment works. You don’t have to quit cold turkey.
The CDC reports that communities with widespread naloxone distribution saw fatal overdoses drop by 34%. That’s not magic. It’s science. And it’s happening right now.
The Bigger Picture
Opioids aren’t going away. They’re still essential for cancer pain, surgery recovery, and severe trauma. But the way we use them has to change. The global opioid market was worth $17.6 billion in 2022. Yet prescriptions have dropped nearly 40% since 2012, thanks to better guidelines and awareness.
The real shift is happening in treatment. The NIH poured $1.5 billion into research for non-addictive painkillers and better overdose reversal tools. New drug formulations are being developed to block abuse without affecting pain relief. And more people are getting access to buprenorphine than ever before.
But the core problem remains: tolerance changes your body. Dependence changes your life. And overdose doesn’t care how long you’ve been using. It only cares if you’re breathing.







11 Comments
jaspreet sandhu
people think opioids are just bad because they make you high but its way deeper than that
your brain literally forgets how to feel normal without them
its not about willpower its about biology
ive seen guys who were doctors and soldiers end up in the same place
its not a choice its a trap
and when you think youve beat it and go back to your old dose you dont even realize how much your body changed
its like trying to run a marathon after a year of sitting on the couch
except the finish line kills you
Alex Warden
why are we even giving these to people in the first place
if you cant control your own body you dont deserve to be on them
we let people get addicted then act surprised when they die
its pathetic
my uncle took them for a broken ankle and now hes on methadone for life
he was 32
stop coddling weak people
LIZETH DE PACHECO
thank you for writing this so clearly
i have a cousin who got hooked after a car accident and i didnt understand why she couldn’t just stop
now i get it
its not about being weak
its about your brain changing
and the worst part is when people think they’re safe after being clean
theyre not
please carry naloxone if you or someone you love has ever used opioids
it saved my cousin’s life last year
Lee M
the entire system is broken
doctors prescribe like they’re handing out candy
pharmaceutical companies bribe and lie
the government looks away until bodies pile up
then they give a press release and call it progress
we dont need more awareness
we need accountability
who got rich off this crisis
and why are they still walking free
Kristen Russell
start low. never go back to your old dose.
this is the most important line here.
if you remember one thing let it be this.
Bryan Anderson
the data presented here is both compelling and deeply concerning
the distinction between dependence and addiction is often misunderstood in public discourse
and the neurological mechanisms described regarding receptor downregulation and respiratory tolerance mismatch are well-documented in peer-reviewed literature
what is encouraging is the growing accessibility of buprenorphine and the shift toward evidence-based harm reduction
these are not moral issues but public health imperatives
we must prioritize compassion over stigma
Liam George
they say fentanyl is in everything but what if its all a lie
what if the real killer is the government pushing this narrative to justify surveillance and control
why is naloxone free but you need a prescription for painkillers
why is buprenorphine suddenly available after 20 years of restrictions
they want you dependent on their solution
they want you to think you need their pills to survive
its not about health
its about power
and the opioid crisis is just the cover
sharad vyas
in india we dont have opioids like this but we have something worse
we have silence
people suffer in pain and no one talks about it
no one helps
no one understands
so when someone gets pills they grab them like a lifeline
its not about pleasure its about escape
and when the body changes no one is there to explain why
we need education not shame
we need doctors who listen not judges who scold
Dusty Weeks
im not saying you shouldnt use them but if you do... pls carry naloxone 😭🙏
my brother did and he lived
he says he still hears the alarm in his head
and he never touches it again
but he still wakes up scared
so please
just carry it
its not a sign of weakness
its a sign you care
Richard Thomas
the most terrifying thing about opioid tolerance isn't that it develops-it's that it's invisible until it's too late
you don't wake up one day and say 'wow i need more now'
you just notice the pain isn't gone as fast
and then you take a little extra
and then a little more
and then you're not taking it for the pain anymore
you're taking it because without it you feel like you're dissolving
and when you quit your body doesn't just miss it
it panics
it forgets how to breathe without the signal
and that's why relapse kills
not because you're weak
but because your biology doesn't know how to unlearn what it learned
Paul Ong
the real win is buprenorphine
no drama no hype
just a tool that works
people say its just replacing one drug with another
but its not
its giving people back their lives
im not a doctor but i know a guy who went from shooting up to fixing his car to playing with his kids
all because he got the right med
stop judging start prescribing
its that simple