Oral Thrush Risk Calculator
Your Medication Factors
Your Habits
Your Risk Assessment
Many people don’t realize that common medications can cause oral thrush - a fungal infection that turns your mouth into a sore, white-spotted mess. If you’re using an inhaler for asthma, taking antibiotics, or on immunosuppressants after a transplant, you’re at higher risk. It’s not rare. Around 20% of people using inhaled corticosteroids develop it, according to the NHS. And it’s not just uncomfortable - it can make eating, swallowing, and even talking painful.
Why Medications Cause Oral Thrush
Your mouth is home to trillions of tiny organisms - bacteria, viruses, and fungi. Normally, they keep each other in check. But when you take certain drugs, that balance breaks. Antibiotics kill off good bacteria that usually hold Candida albicans - the main fungus behind thrush - in check. Inhaled steroids coat your mouth and throat, creating a moist, sugar-rich environment where Candida thrives. Immunosuppressants weaken your body’s ability to fight off invaders at all.
It’s not just one drug. It’s the combination. Someone on asthma inhalers plus a course of amoxicillin? That’s a perfect storm. The CDC reports over 12.9 million Americans use inhaled steroids. Multiply that by the millions taking antibiotics each year, and you’ve got a huge population quietly developing thrush without knowing why.
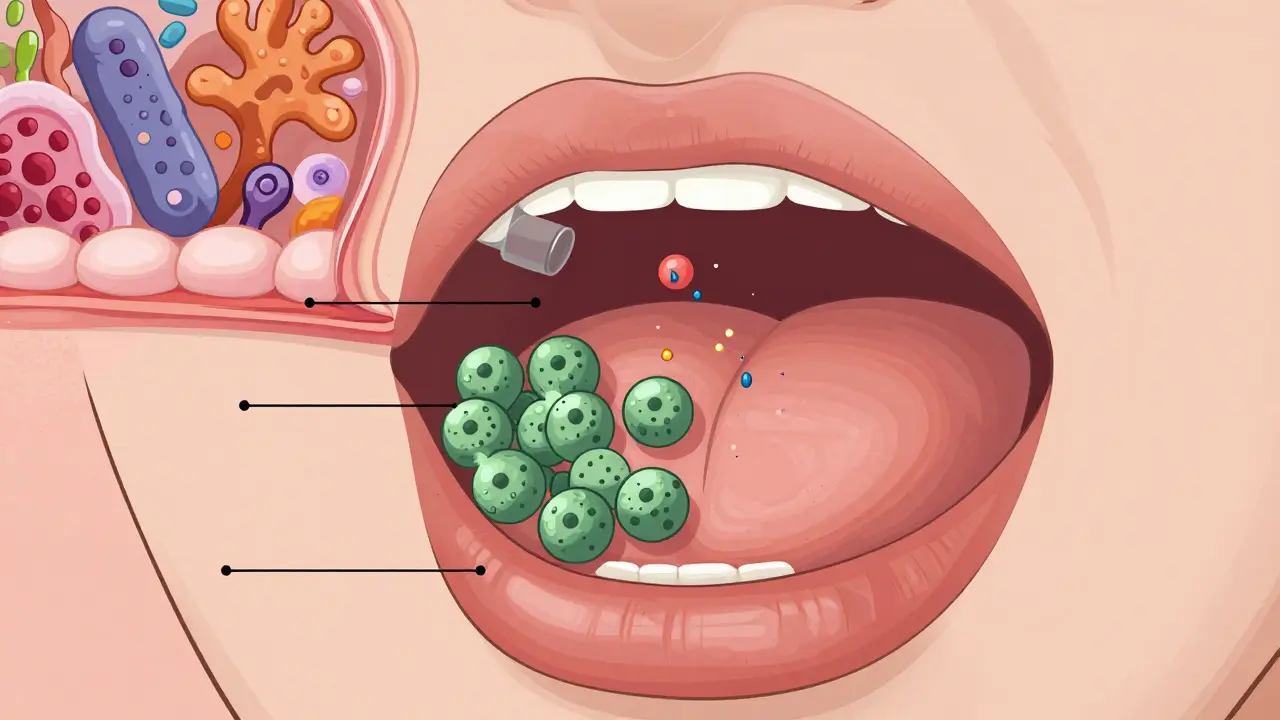
What Oral Thrush Looks and Feels Like
It doesn’t always look like the textbook white patches. Sometimes it’s just redness under your dentures. Other times, you’ll see creamy, cottage-cheese-like spots on your tongue or inner cheeks. If you scrape them off, you might see raw, bleeding tissue underneath. The real tell? Pain. Swallowing feels like swallowing sand. Your taste buds feel dull. Your mouth burns, especially with spicy or acidic foods.
It’s easy to mistake for canker sores or even a bad cold. But if you’ve been on antibiotics or steroids in the last two weeks and your mouth suddenly feels off - don’t wait. See your doctor. Left untreated, thrush can spread to your esophagus, making swallowing nearly impossible.
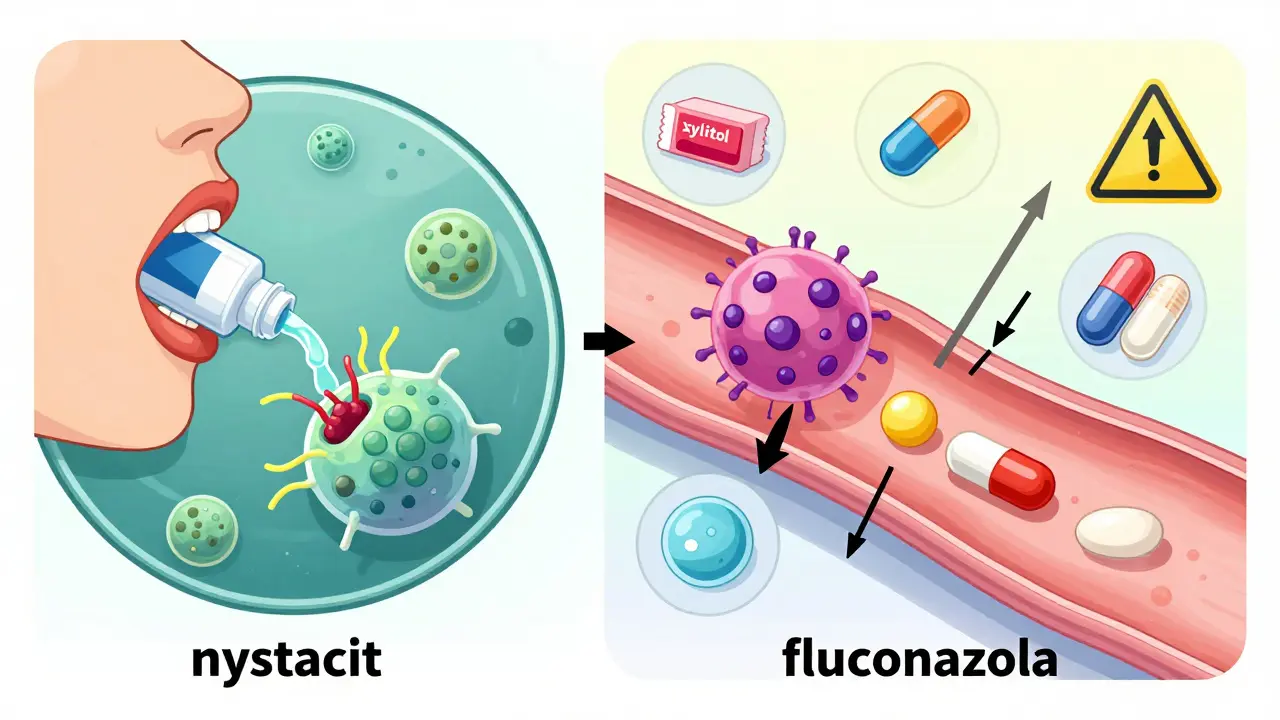
Nystatin: The First-Line Treatment
If you’re otherwise healthy and your thrush is mild, nystatin is what your doctor will likely prescribe first. It’s been around since the 1950s, and it works by punching holes in the fungal cell wall. You get a liquid suspension - usually 100,000 units per mL - and you swish it around your mouth for at least two minutes, four times a day. Then you spit it out. Not swallow it.
That last part is critical. A 2022 study found 42% of treatment failures happened because people swallowed the medicine instead of letting it sit in their mouth. The FDA and Cleveland Clinic both emphasize this. You need direct contact with the infected areas. Swishing after meals gives you the best chance.
It’s not glamorous. The taste? Chalky, bitter, unpleasant. Over 78% of users in WebMD surveys complain about it. But it’s safe. Less than 5% gets absorbed into your bloodstream. That means no liver stress, no drug interactions. It’s safe for kids, pregnant women, and seniors. A 30-day supply costs around $15.79 in generic form.

Fluconazole: When You Need Something Stronger
But what if nystatin doesn’t work? Or if you have severe thrush, or you’re immunocompromised? That’s when fluconazole comes in. Sold as Diflucan, it’s a pill you take once a day. It’s absorbed into your blood and travels everywhere - including your mouth. It’s more effective than nystatin: 95% success rate versus 89% in a 2022 meta-analysis.
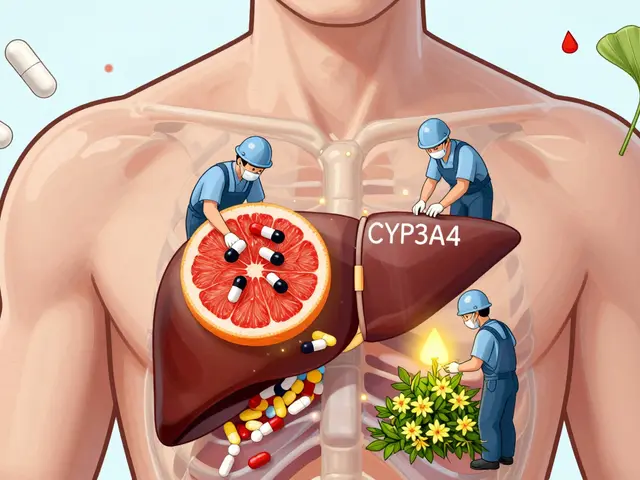
But it’s not without risks. Fluconazole can interact with 32 common medications - warfarin, phenytoin, diabetes pills. It can cause liver damage. The FDA has black box warnings for this. One patient on PatientsLikeMe developed acute liver failure after taking it. It’s also more expensive: $23.49 for generic, $347 for brand-name.
Doctors use it when they have to. For transplant patients, cancer patients, or anyone with recurrent thrush. It’s the gold standard - but only when the benefits outweigh the risks.
Resistance Is Growing - And It’s a Real Problem
Here’s something few patients know: Candida is learning to fight back. The European Society of Clinical Microbiology reports fluconazole resistance jumped from 3% in 2010 to 12% in 2022. That means more cases won’t respond to the usual pill. In hospitals, a scary new strain called Candida auris is spreading - resistant to multiple antifungals.
That’s why culture tests are becoming more common in recurrent cases. If thrush keeps coming back, your doctor might take a swab to see exactly which fungus is growing. Not all Candida are the same. Some respond to nystatin, others need something stronger - or newer.
Prevention: The Real Game-Changer
Here’s the truth: treating thrush is hard. Preventing it? Much easier.
If you use an inhaler, rinse your mouth with water immediately after every puff. Don’t just swish - spit it out. The NHS found this simple step cuts thrush risk by 65%. Brush your teeth twice a day. Floss. Clean dentures daily. If you wear them, take them out at night.
Watch your sugar. Candida feeds on it. Cut back on sweets and sugary drinks. If you have diabetes, keep your HbA1c below 7.0%. High blood sugar = easy pickings for fungus.
And try xylitol. It’s not just for gum. A 2022 study in the Journal of Dental Research showed xylitol reduces Candida colonization by 40%. Use toothpaste or mouth rinses with it. Chew xylitol gum after meals. It’s safe, natural, and works.
New Options Are Coming
There’s good news on the horizon. In March 2023, the FDA approved a new nystatin tablet called Mycolog-II. It sticks to your mouth lining for up to four hours - no more swishing four times a day. Early trials showed 94% effectiveness. That’s a huge win for people who can’t stand the taste or the schedule.
Probiotics are also gaining traction. Research in Nature Microbiology found that Lactobacillus reuteri, a specific strain of good bacteria, cuts thrush recurrence by 57% when taken alongside antifungals. You can find it in some supplements or fermented foods.
Three new antifungal drugs are in Phase II trials. They’re designed to be more targeted, with fewer side effects. The future isn’t just about killing fungus - it’s about restoring balance.
What to Do Right Now
If you suspect you have oral thrush:
- Check your meds. Are you on an inhaler, antibiotics, or immunosuppressants?
- Look in the mirror. White patches? Redness? Pain when swallowing?
- Don’t wait. See your doctor or dentist. Don’t try OTC remedies - they won’t work.
- If prescribed nystatin: swish for two minutes, four times a day. Spit. Don’t swallow.
- If prescribed fluconazole: tell your doctor about every other medication you take.
- Start prevention today: rinse after inhalers, brush twice, use xylitol, control blood sugar.
Oral thrush is treatable. But it’s not something you should ignore. The longer you wait, the harder it gets - and the more likely it is to come back.
Can oral thrush go away on its own?
Sometimes, yes - especially if it’s mild and caused by a short course of antibiotics. But if you’re on long-term steroids, immunosuppressants, or have diabetes, it won’t resolve without treatment. Waiting risks it spreading to your throat or esophagus. Don’t gamble with it.
Is oral thrush contagious?
Not really in healthy people. Candida is already in most mouths. Thrush happens when your body’s defenses are down - not from kissing or sharing cups. But if you’re immunocompromised, avoid sharing toothbrushes or eating utensils. The fungus can spread between people with weakened immune systems.
Can I use mouthwash for oral thrush?
Regular alcohol-based mouthwashes won’t help - they kill good bacteria too, making thrush worse. Antiseptic rinses like chlorhexidine are sometimes used in hospitals, but they’re not first-line for home use. Stick to water rinses after inhalers and prescribed antifungals. Avoid mouthwashes with sugar.
Why does nystatin taste so bad?
It’s a natural antifungal made from soil bacteria. The taste is unpleasant by design - it’s not meant to be palatable. It’s not a flavoring issue; it’s a chemical one. The new mucoadhesive tablet (Mycolog-II) was developed specifically to solve this problem. Until then, chilling the suspension slightly or mixing it with a bit of applesauce (if approved by your doctor) can help.
How long until I feel better?
Most people start feeling better in 2-3 days. The white patches fade within a week. But you must finish the full course - usually 7-14 days. Stopping early is the #1 reason thrush comes back. Even if you feel fine, keep using the medicine as directed.
Can I get oral thrush from my inhaler?
Yes - and it’s one of the most common causes. Inhaled corticosteroids leave a residue in your mouth and throat, killing protective bacteria and creating a perfect environment for Candida. That’s why rinsing your mouth with water immediately after each puff is so important. It’s not optional - it’s medical advice backed by data.
Are there natural remedies for oral thrush?
Coconut oil, garlic, and tea tree oil are often suggested online. But there’s no strong evidence they work reliably. Some may even irritate your mouth. If you have thrush, stick to proven treatments: nystatin or fluconazole. Natural remedies can be used for prevention - like probiotics - but not as a replacement for medicine.
Final Thoughts
Oral thrush from medications isn’t a sign you did something wrong. It’s a side effect - a common, predictable one. The key is knowing it’s coming, recognizing it early, and acting fast. Use your inhaler correctly. Rinse. Brush. Watch your sugar. Talk to your doctor about prevention before you even get sick. And if it happens? Don’t panic. Nystatin works. Fluconazole works too - if used wisely. The best treatment is the one you’ll stick with. And the best prevention? A habit you don’t skip.

11 Comments
Roshan Joy
Just started using an inhaler last month and noticed white spots on my tongue. Thought it was just food residue. Glad I read this - rinsing after every puff is now a habit. Xylitol gum after meals too. Small changes, big difference.
Jason Shriner
so like... our bodies are just little fungal theme parks and meds are the free tickets? thanks, pharma. 🤡
Jennifer Littler
As a clinical pharmacist, I can confirm the nystatin swish-and-spit protocol is critical. Studies show compliance drops sharply when patients swallow it - often because they mistake it for a sore throat remedy. The mucoadhesive tablet (Mycolog-II) is a game-changer for adherence. Also, xylitol’s anti-adhesion mechanism against Candida is underutilized in primary care.
Alfred Schmidt
FLUCONAZOLE IS NOT A TOY. I watched my uncle go into liver failure because he took it with his blood pressure med and thought 'it's just a pill.' You don't play Russian roulette with your liver because you're too lazy to rinse your mouth. Stop being careless. This isn't a suggestion - it's a warning.
Alex Smith
Interesting how we treat thrush like a bug to be eradicated, but maybe we should be thinking about restoring balance instead. Probiotics like Lactobacillus reuteri? That’s not medicine - that’s ecology. We’ve been waging chemical war on our own microbiome for decades. Maybe it’s time to stop bombing the neighborhood and start gardening again.
Michael Patterson
Man I read this whole thing and I'm still confused. Like, is it the inhaler or the antibiotics or the sugar or the lack of brushing or the stress or the moon phase? I mean come on, it's like everything causes it and nothing fixes it. And why does nystatin taste like chalk mixed with regret? And why is everyone on here acting like this is normal? It's not normal. It's gross. And why is no one talking about the fact that the new tablet is like $80? I don't have that kind of money. I'm just trying to breathe and not have my tongue look like moldy cheese.
Madhav Malhotra
From India - we’ve been using neem rinses and turmeric paste for generations. Not a replacement for meds, but as a supportive ritual? Works wonders. Also, we don’t wait for symptoms - we rinse after inhalers like it’s prayer. Simple. Sacred. Effective.
Priya Patel
OMG I thought I was dying. White patches + burning mouth = I was convinced I had cancer. Turns out it was just my asthma inhaler + that one week of amoxicillin. I cried when the nystatin worked. Also, I started chewing xylitol gum like it’s my job. Now I’m addicted. And I don’t even like gum. 🙃
Sean Feng
So rinse after inhalers. Got it. Done. Next.
Priscilla Kraft
Thank you for writing this so clearly. I’m a nurse and I see this all the time - patients think it’s ‘just a sore mouth’ and delay care. The prevention tips are gold. Especially the xylitol and rinsing. I’ve started handing out pamphlets with this info to my asthma and transplant patients. Also, I love that you mentioned probiotics - L. reuteri is magic. My mom’s thrush hasn’t come back in 18 months since she started taking it. 🙏
Vincent Clarizio
You people are missing the bigger picture. This isn’t about thrush. This is about the collapse of the medical-industrial complex. They sell you inhalers, then sell you nystatin, then sell you fluconazole, then sell you the new tablet - all while knowing the real solution is $0.50 worth of water and a habit. They don’t want you to rinse. They want you dependent. The fungi are just the symptom. The real disease is profit-driven healthcare. Wake up. The system is rigged. And no, I’m not on any meds. I just breathe. And I’m fine. Probably because I don’t trust doctors. Or pills. Or anything with a patent.