It’s 2025. You walk into the pharmacy to refill your antidepressant. The pharmacist hands you a small white pill in a plain bottle. "It’s the generic," they say. You take it home, but something feels off. You don’t feel better. You start blaming the pill. You’re not crazy. You’re experiencing something real - and it has nothing to do with chemistry.
Generics aren’t weaker. But your brain thinks they are.
Generic medications contain the exact same active ingredient, in the same dose, as their brand-name cousins. The FDA requires them to be bioequivalent - meaning they work the same way in your body. But here’s the twist: when patients believe they’re taking a cheaper, less-known version, their bodies often respond as if the drug doesn’t work as well. This isn’t imagination. It’s neuroscience.
Studies show that when people take a sugar pill labeled as a brand-name drug like Nurofen, they report pain relief just as strong as if they’d taken real ibuprofen. But when the same sugar pill is labeled "generic ibuprofen," the pain relief drops by nearly half. The pill didn’t change. Only the label did.
This isn’t about the drug. It’s about your brain’s expectation. Your mind has learned - from years of advertising, packaging, and word-of-mouth - that brand names mean quality. When you see a colorful box with a familiar logo, your brain says, "This will work." When you see a plain bottle with a generic name, your brain whispers, "Will this even help?"
How your brain tricks you into feeling worse
It doesn’t stop at effectiveness. Your perception can make you feel side effects that aren’t there.
In one famous study, people were given placebo pills - no active ingredients - and told they were statins, a cholesterol-lowering drug. Even though the pills were inert, 4% to 26% of participants reported muscle pain and quit taking them. Why? Because they’d heard statins cause muscle pain. So when they felt a normal ache or fatigue, their brain labeled it as a side effect. They weren’t lying. They were experiencing real discomfort - triggered by fear, not chemistry.
Even price changes your pain. In a 2017 study, researchers gave people identical pain-relief creams. One group was told it cost $200. The other, $2. The expensive cream? People reported feeling less pain. The cheap one? They felt more. Brain scans confirmed it: the "expensive" group had stronger activity in pain-processing areas of the brain. Their bodies were reacting to the price tag - not the cream.
And it’s not just pain. People on generic antidepressants report feeling less improvement - even when blood tests show identical drug levels to the brand-name version. One Reddit user wrote: "I switched to generic sertraline and felt like I was back at square one. My doctor said it’s the same. But I didn’t believe it. And I didn’t feel better."
Branding isn’t magic. But it’s powerful.
Brand-name drugs don’t have better ingredients. But they have better stories. They have logos, TV ads, doctor endorsements, and decades of trust. Generic drugs? They have a label, a barcode, and a lower price.
That’s why pharmaceutical companies now sell "premium generics" - same active ingredient, same dose, but with nicer packaging, brighter colors, and even brand names like "Advil Migraine" (which is just ibuprofen in a fancy bottle). These aren’t new drugs. They’re rebranded generics. And they’re working. In the migraine market, one premium generic now holds 17% of sales - even though it’s chemically identical to the $2 bottle down the aisle.
It’s not deception. It’s psychology. Your brain doesn’t care about molecular structure. It cares about signals. And packaging, price, and naming are powerful signals.
Why some people don’t notice the difference
Not everyone reacts this way. About 30% of people are highly sensitive to placebo and nocebo effects. The rest? They don’t care if it’s brand or generic. They just want it to work - and if it does, they don’t question it.
Studies show that people with chronic pain, anxiety, or depression are more likely to be affected. Why? Because these conditions are heavily influenced by expectation and emotion. Your brain is already scanning for signs of relief or danger. A simple label can tip the scale.
Cardiovascular patients? Less affected. Why? Their medication’s effects are measurable - blood pressure, cholesterol levels. If the numbers improve, they trust the pill, no matter the label.
But for depression? Anxiety? Migraines? Sleep? Pain? These are subjective. You feel them. No machine can measure them perfectly. So your brain fills in the gaps. And if you think the drug won’t work, your brain makes sure you feel it.
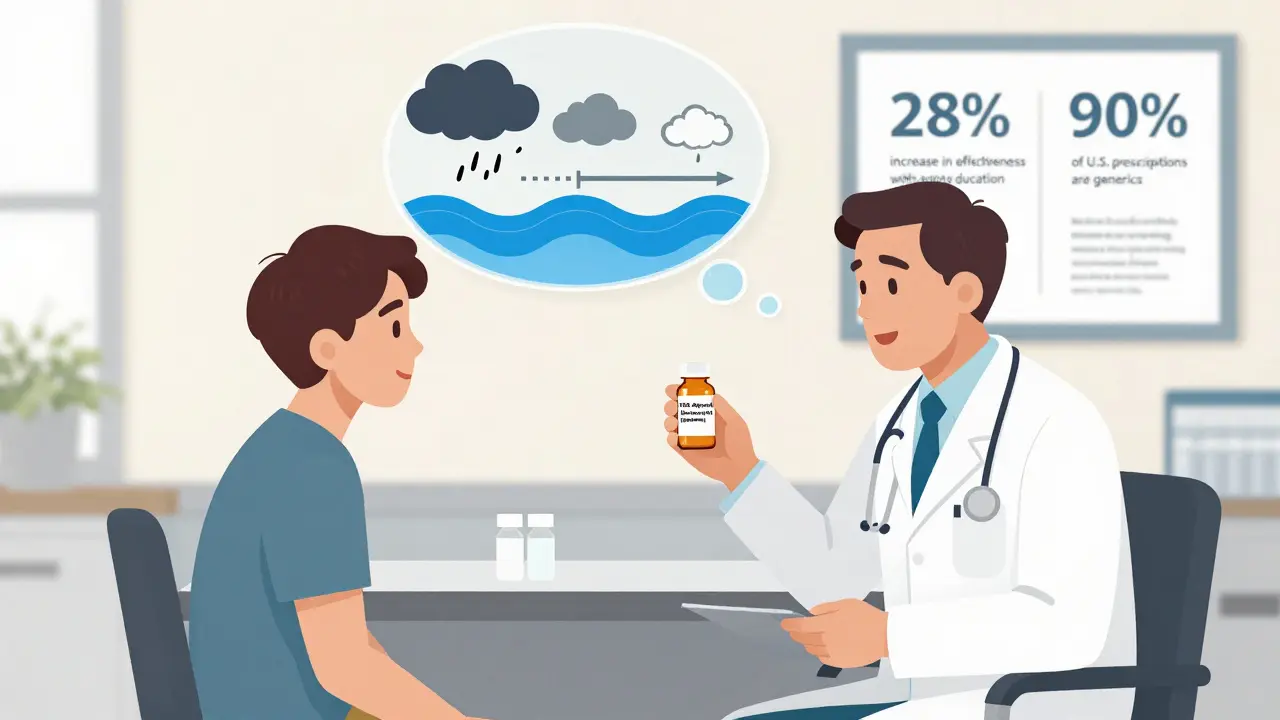
What doctors and pharmacists can do
This isn’t just a patient problem. It’s a system problem.
Doctors and pharmacists often say, "It’s the same thing." But that phrase - "it’s the same" - can backfire. It sounds dismissive. It implies the difference is imaginary. And that makes patients feel unheard.
What works better? Specific, calm explanations.
- "The FDA requires generics to deliver the same amount of medicine in your bloodstream as the brand. The difference is less than 10% - and that’s within safe, effective limits."
- "Over 90% of prescriptions in the U.S. are generics. Most people get the same results."
- "I’ve had patients who switched and felt better - because they stopped worrying about whether it would work."
Adding a simple note to the prescription bottle - "This is an FDA-approved equivalent to [Brand Name]" - increases patient confidence by 34%. That’s not branding. That’s clarity.
And never say, "This is cheaper." That triggers the nocebo effect. Mentioning price makes people expect worse results - even if the drug is identical.
The hidden cost of perception
This isn’t just about feelings. It’s about money.
When patients stop taking their generic meds because they think they don’t work, they end up back in the doctor’s office. They get unnecessary tests. They switch back to brand-name drugs. They miss work. They get sicker.
Researchers estimate that negative perceptions of generics cost the U.S. healthcare system $1.2 billion to $1.8 billion a year. That’s not because generics are worse. It’s because people believe they are.
And it’s worse for mental health. Patients are 27% more likely to quit their generic antidepressant within 30 days than their brand-name version - even though both have the same chemical structure.
That’s not a failure of medicine. It’s a failure of communication.
Can we fix this?
Yes - and we already are.
Some clinics are using short educational videos before handing out generics. One study from Oxford found that showing patients a 90-second video explaining how expectations affect treatment increased the effectiveness of generic antidepressants by 28%. The video didn’t change the pill. It changed the mind.
Companies like Aurobindo Pharma are designing "expectation-optimized" packaging - using colors and fonts that signal trust and reliability, without crossing into misleading marketing. Blue and white? Calm. Clean. Professional. These aren’t gimmicks. They’re cues that help the brain relax.
The FDA now advises doctors to avoid phrases like "just a generic." Instead, they recommend: "This is a safe, approved, and effective version of your medication."
It’s not about selling more brand-name drugs. It’s about making sure people get the treatment they need - without their own minds getting in the way.
What you can do
If you’re on a generic medication and you’re not feeling better:
- Don’t assume it’s the pill. Ask your doctor to check your blood levels - many drugs have reliable tests to confirm you’re getting the right dose.
- Write down how you feel before and after switching. Sometimes, the change is in your head - and recognizing that helps you take back control.
- Ask for a simple explanation: "Can you tell me how this is the same as the brand?" Knowledge reduces fear.
- If you’re still unsure, try switching back to the brand for a few weeks - then switch again. You might be surprised by the results.
And if you’re a caregiver, parent, or friend: don’t dismiss someone’s concerns. Say, "I get why you’d feel that way. Let’s talk to your doctor about it."
The placebo effect isn’t a trick. It’s a window into how deeply our minds shape our bodies. And when it comes to medicine, perception isn’t just part of the story - it’s often the whole story.
Are generic medications really as effective as brand-name drugs?
Yes. By law, generic medications must contain the same active ingredient, in the same strength and dosage form, as the brand-name version. The FDA requires them to be bioequivalent - meaning they work the same way in your body. Studies show that for most conditions, generics perform just as well. But perception can make people believe they don’t - even when they do.
Why do some people feel worse on generic medications?
It’s often due to the nocebo effect - when negative expectations cause real physical symptoms. If someone believes generics are inferior, their brain may amplify normal sensations like fatigue or mild nausea as side effects. Brain scans show these reactions are real: the nervous system responds to belief, not just chemistry.
Does packaging or price affect how well a generic works?
Yes - not because the drug changes, but because your brain responds to cues. Studies show that identical placebos labeled as expensive or branded produce stronger pain relief and fewer reported side effects. Conversely, plain packaging or mentions of low cost can trigger worse outcomes. It’s not the medicine - it’s the meaning you assign to it.
Can doctors help patients feel better on generics?
Absolutely. Simple, clear communication makes a big difference. Explaining that generics meet the same FDA standards as brand-name drugs, avoiding phrases like "just a generic," and using phrases like "this is an approved equivalent" can increase adherence by 18-22%. Some clinics now use short educational videos before dispensing generics - and see up to a 28% boost in effectiveness.
Is it safe to switch from brand-name to generic medication?
For most people, yes. Over 90% of prescriptions in the U.S. are filled with generics, and they’ve been safely used for decades. The FDA requires strict testing for bioequivalence. However, if you have a condition with high placebo sensitivity - like depression, chronic pain, or anxiety - talk to your doctor before switching. Your perception matters, and your doctor can help you manage it.
Why do some pharmacies still push brand-name drugs?
Sometimes it’s insurance rules - some plans require you to try the generic first. Other times, it’s patient pressure. If a patient insists on the brand, the pharmacist may comply. But increasingly, pharmacies are trained to educate patients about generics, not just push them. The goal isn’t to save money - it’s to make sure patients get the treatment they need without fear getting in the way.
What’s next?
The future of medicine isn’t just about better drugs. It’s about better minds. We’re learning that healing isn’t just chemical - it’s psychological. And when we understand that, we can design treatments that work with the brain, not against it.
Generics aren’t second-rate. They’re the quiet heroes of modern healthcare - saving billions, reaching millions, and working just as well as the brand names. But only if we let them.






