Understanding the Link Between Open-Angle Glaucoma and Dry Eye Syndrome
As someone who has been researching eye health for years, I have come across many cases where patients suffer from both open-angle glaucoma and dry eye syndrome. This has led me to wonder about the relationship between the two conditions. In this article, I will discuss the possible link between open-angle glaucoma and dry eye syndrome, and why it is essential for anyone with either of these conditions to be aware of the other.
What is Open-Angle Glaucoma, and How Does it Affect the Eye?
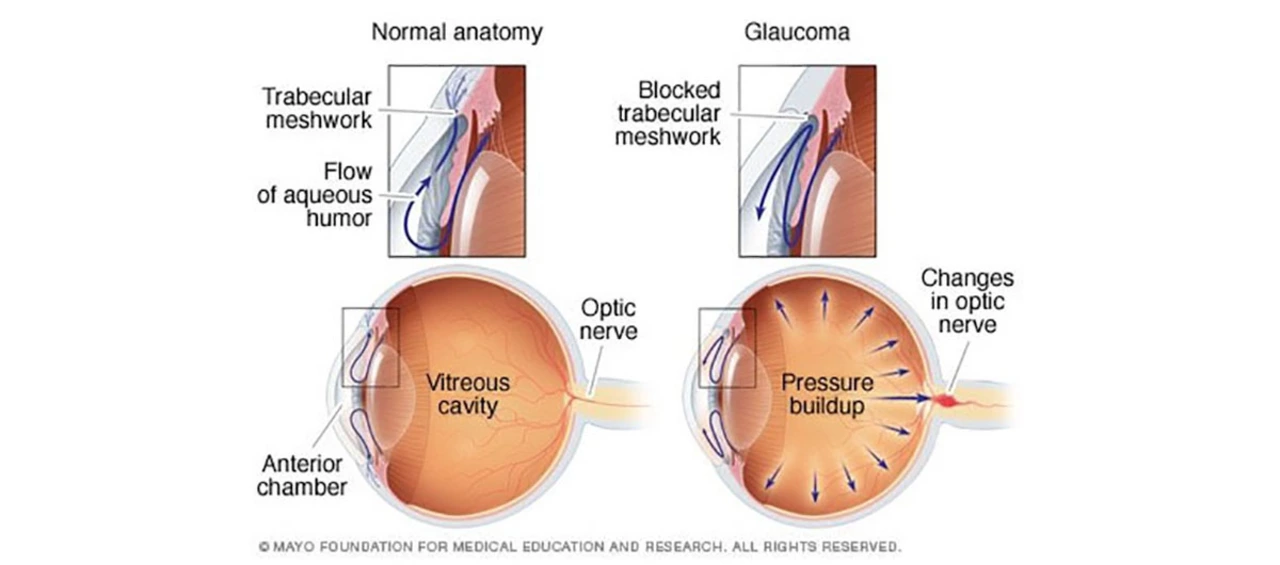
Open-angle glaucoma is a chronic eye condition that affects millions of people worldwide. It occurs when the eye's drainage system becomes less efficient over time, leading to increased pressure within the eye. This pressure can damage the optic nerve, which is responsible for transmitting visual information from the eye to the brain. If left untreated, open-angle glaucoma can lead to irreversible vision loss and, eventually, blindness.
The exact cause of open-angle glaucoma is still unknown, but certain factors can increase a person's risk of developing the condition. These factors include age, family history, high intraocular pressure, and certain medical conditions, such as diabetes and high blood pressure.
Dry Eye Syndrome: A Common and Uncomfortable Condition
Dry eye syndrome, also known as keratoconjunctivitis sicca, is a common condition that affects millions of people worldwide. It occurs when the eyes do not produce enough tears or when the tears evaporate too quickly, leading to dryness, discomfort, and sometimes even inflammation. Dry eye syndrome can have various causes, including aging, certain medications, medical conditions, and environmental factors such as exposure to wind and dry air.
Although dry eye syndrome is typically not a serious condition, it can significantly impact a person's quality of life. Symptoms of dry eye syndrome include burning, itching, redness, blurred vision, and a sensation that something is stuck in the eye.
Exploring the Connection Between Open-Angle Glaucoma and Dry Eye Syndrome
Recent studies have suggested that there might be a link between open-angle glaucoma and dry eye syndrome. One theory is that both conditions are related to the eye's inflammatory processes. Inflammation plays a role in the development of open-angle glaucoma, as it can cause the eye's drainage system to become less efficient. Similarly, inflammation can also contribute to dry eye syndrome by damaging the glands responsible for tear production.
Another possible connection between the two conditions is the use of certain glaucoma medications. For example, some eye drops used to treat glaucoma can cause dry eye symptoms as a side effect. This is particularly true for prostaglandin analogs, a common class of glaucoma medications that can cause changes in the composition of the tears, leading to dryness and discomfort.
Why It's Important to Be Aware of the Relationship Between These Conditions
Understanding the potential link between open-angle glaucoma and dry eye syndrome is crucial for several reasons. First, it can help patients and healthcare providers better manage both conditions. For example, if a person with glaucoma is experiencing dry eye symptoms, their healthcare provider may consider alternative treatments or adjust their medications to minimize side effects.
Second, being aware of the relationship between these conditions can help patients recognize the symptoms of both and seek appropriate treatment early. Early detection and treatment of both open-angle glaucoma and dry eye syndrome are essential for preventing long-term complications and maintaining good eye health.
Conclusion: The Importance of Comprehensive Eye Care
In conclusion, there appears to be a connection between open-angle glaucoma and dry eye syndrome, although more research is needed to understand the exact nature of this relationship. By being aware of this potential link, those with either condition can better manage their eye health and work with their healthcare providers to find the most effective treatment options.
As always, it is essential to prioritize regular eye exams and comprehensive eye care, particularly for those with a higher risk of developing eye conditions such as open-angle glaucoma and dry eye syndrome. By staying proactive about your eye health, you can help ensure that your vision remains clear and comfortable for years to come.






20 Comments
James Gray
Totally agree, meds can dry ur eyes.
Scott Ring
When you think about the inflammatory cascade, it’s clear that both glaucoma and dry eye share common pathways. The eye’s immune response can affect the trabecular meshwork and the Meibomian glands at the same time. I’ve seen patients who start on prostaglandin analogues and then complain about gritty sensations. Adjusting the preservative load often helps those symptoms without compromising pressure control.
Shubhi Sahni
From a clinical perspective, it is essential to highlight that ocular surface disease may exacerbate measurement variability; therefore, clinicians should always consider tear film quality when interpreting intraocular pressure readings, especially in patients on chronic topical therapy, which often contains benzalkonium chloride, a known irritant.
Danielle St. Marie
🇺🇸 Our eye docs know best! 😎
keerthi yeligay
Dry eye can be a side effect of many glaucoma drops, so watch out for that.
Peter Richmond
In practice, a balanced treatment plan that addresses both IOP reduction and ocular surface health is paramount.
Bonnie Lin
Exactly, Peter. Adding a preservative‑free formulation or using artificial tears can make a huge difference for comfort.
sara fanisha
Great reminder, James! Staying positive and proactive about eye health always pays off.
Tristram Torres
Both conditions can be linked by inflammation, that's something worth noting.
Jinny Shin
Oh my gosh, it’s like a tragic romance between pressure and dryness – the drama never ends!
deepak tanwar
While the previous comment romanticizes the issue, the reality is that untreated glaucoma remains the leading cause of irreversible blindness, thus any ancillary discomfort should never distract from aggressive IOP management.
Abhishek Kumar
Looks like more research is needed.
hema khatri
Wow!!! The link between inflammation and eye health is just mind‑blowing – thanks for sharing!!
Jennell Vandermolen
Peter, your point about a balanced plan is spot‑on; patients appreciate when we address tear film health alongside pressure control.
Mike Peuerböck
It is incumbent upon ocular specialists to diligently assess both intraocular pressure dynamics and ocular surface integrity to ensure comprehensive patient care.
Simon Waters
Keeping an eye on both problems can save sight.
Vikas Kumar
Indeed, monitoring both is essential, though most patients overlook the dryness aspect.
Celeste Flynn
One of the reasons open‑angle glaucoma and dry eye often co‑occur is the shared role of chronic low‑grade inflammation. In glaucoma, inflammatory cytokines can remodel the trabecular meshwork, reducing outflow facility and raising intraocular pressure. At the same time, those same cytokines can impair the function of the meibomian glands, leading to evaporative dry eye. Moreover, many prostaglandin analogues contain preservatives such as benzalkonium chloride, which can disrupt the lipid layer of the tear film, causing increased tear evaporation. Studies have shown that patients on preservative‑rich drops report higher Ocular Surface Disease Index (OSDI) scores compared to those on preservative‑free alternatives. Switching to preservative‑free or using a short‑term topical steroid can mitigate surface inflammation while maintaining IOP control. Additionally, incorporating omega‑3 fatty acid supplements has been shown to improve tear film stability in glaucoma patients. Clinicians should routinely assess tear breakup time (TBUT) and corneal staining during glaucoma follow‑up visits. Addressing meibomian gland dysfunction with warm compresses or lid hygiene can also reduce dry eye symptoms without affecting glaucoma treatment efficacy. Punctal plugs are another option for refractory cases, as they increase tear retention without interfering with aqueous humor dynamics. It is also important to consider systemic medications; antihistamines and antihypertensives can exacerbate dryness and may need adjustment. Regular patient education about the potential side effects of eye drops empowers individuals to report symptoms early. Early intervention can prevent the vicious cycle where discomfort leads to poor adherence to glaucoma therapy, which in turn risks progression of optic nerve damage. Ultimately, a multidisciplinary approach involving optometrists, ophthalmologists, and primary care providers yields the best outcomes for patients facing both conditions.
Shan Reddy
Thanks for the detailed rundown, Celeste – that’s super helpful.
CASEY PERRY
Integrating ocular surface assessment into glaucoma management protocols enhances therapeutic efficacy and patient compliance.