Every year, tens of thousands of people end up in the hospital-not because their condition got worse, but because something they took to get better made something else they were taking dangerous. This isn’t rare. It’s common. And it’s mostly preventable.
Drug interactions happen when one substance changes how another substance works in your body. It could be another pill, a supplement, grapefruit juice, or even a health condition you already have. These aren’t just theoretical risks. They’re real, measurable, and often deadly. In the U.S. alone, drug interactions are linked to over 106,000 deaths each year and cause nearly 7% of all hospital admissions. That’s more than the number of people hospitalized for stroke or heart failure in some years.
How Drug Interactions Actually Work
There are three main types of drug interactions, and they all mess with your body’s ability to handle medication the way it’s supposed to.
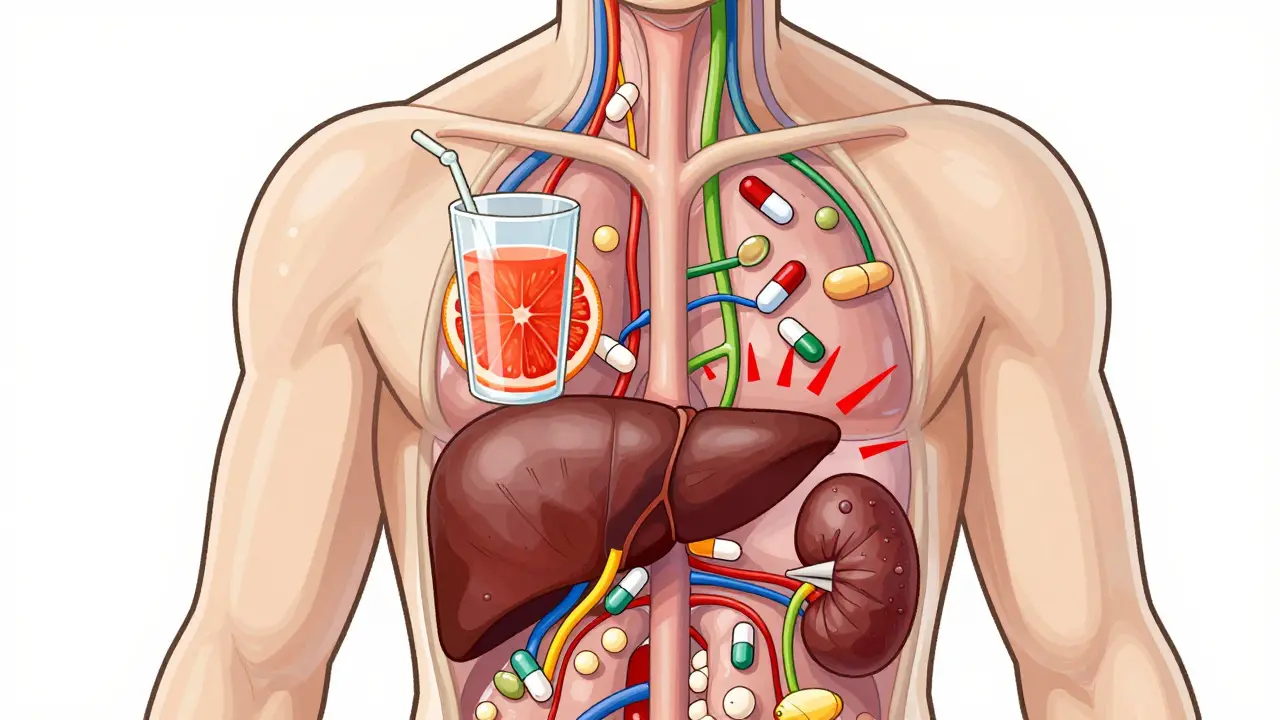
Drug-drug interactions are the most common. When you take two medications at the same time, one can speed up, slow down, or block the other. For example, fluconazole (an antifungal) stops your liver from breaking down simvastatin (a cholesterol drug). That causes simvastatin to build up in your blood-up to 2,000% higher than normal. That’s not just a bump in side effects. That’s a direct path to rhabdomyolysis, a condition where muscle tissue breaks down and can lead to kidney failure.
Drug-food interactions are sneaky because they seem harmless. Grapefruit juice is the classic example. It contains chemicals called furanocoumarins that block an enzyme in your gut (CYP3A4) responsible for breaking down about half of all prescription drugs. When you drink grapefruit juice with certain statins, blood levels can jump 300% to 600%. No one tells you this when you pick up your prescription. But your pharmacist might-if you ask.
Drug-condition interactions happen when your existing health problem changes how a drug behaves. For instance, if you have kidney disease, your body can’t clear out certain antibiotics the way a healthy person can. That means even a normal dose can become toxic. Or if you have an overactive thyroid and take levothyroxine (Synthroid), taking calcium or iron supplements at the same time can block absorption. You might think you’re taking your medication correctly, but your thyroid levels stay high because your body never absorbed the drug.
Why Some Medications Are More Dangerous Than Others
Not all drugs are created equal when it comes to interactions. Some are like landmines-tiny changes in how they’re taken can trigger big problems.
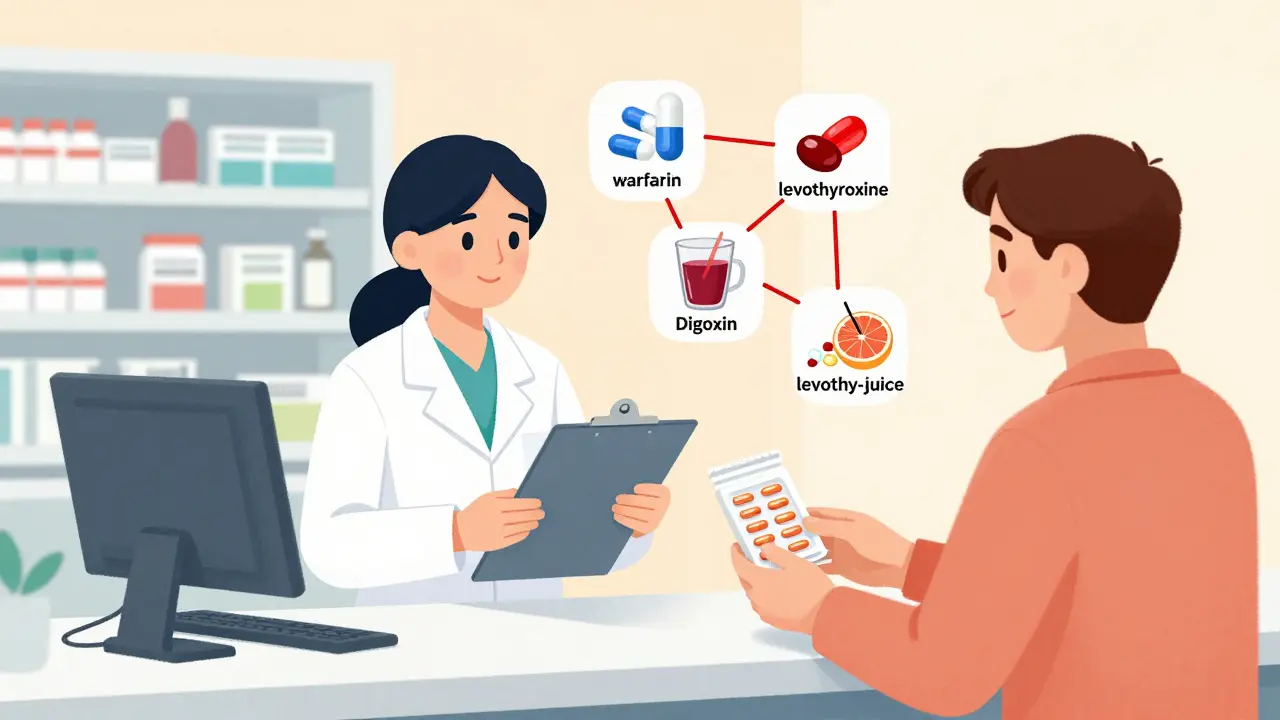
Warfarin (Coumadin) is the most notorious. It has over 600 known interactions. Antibiotics, antifungals, even cranberry juice can throw off your INR (a blood clotting measure). One study found that 68% of patients on warfarin who started a new antibiotic had dangerous spikes in INR within days. That means a higher risk of internal bleeding. Many of these patients didn’t even know the new drug was a problem.
Digoxin, used for heart rhythm problems, interacts with over 300 substances. Diuretics can lower potassium levels, making digoxin more toxic. Certain antibiotics like clarithromycin can cause digoxin to build up to dangerous levels. And levothyroxine? Take it with calcium, iron, or even soy milk, and your body absorbs almost none of it. You’re paying for a pill your body never uses.
These aren’t edge cases. They’re everyday risks. And they’re often missed because doctors don’t have time to review every supplement a patient takes. Patients don’t always remember to mention them. And pharmacies? Most only check for the most obvious conflicts.
The Hidden Costs of Ignoring Interactions
It’s not just about hospital visits. It’s about money, stress, and wasted treatment.
In the U.S., medication-related problems-including interactions-cost the healthcare system $528 billion a year. That’s more than the entire budget of the Department of Defense. Of that, $30 billion comes from avoidable hospitalizations and emergency visits caused by interactions. And it’s not just the elderly. People with five or more chronic conditions have a 68% chance of experiencing at least one dangerous interaction. That’s not luck. That’s systemic.
Older adults are especially vulnerable. They take an average of 4.7 prescription drugs daily. And their bodies don’t process drugs the same way they did in their 30s. Liver and kidney function slow down. Muscle mass drops. Fat increases. All of this changes how drugs move through the body. Yet, most drug trials exclude older patients with multiple conditions. That means we’re prescribing based on data from healthy 40-year-olds. It’s like building a car for flat roads and then driving it up a mountain.
The FDA admits that only 25% of serious drug interactions are caught before a drug hits the market. The rest show up after thousands of people start taking it. And pharmaceutical companies? A 2022 study found they underreport interaction risks in clinical trials. That’s not negligence-it’s a structural flaw in how drugs are approved.
What You Can Do to Protect Yourself
You don’t need to be a doctor to prevent a dangerous interaction. You just need to be informed and proactive.
- Keep a complete list of everything you take. Not just prescriptions. Include over-the-counter meds, vitamins, herbs, and supplements. Even the ones you only take “once in a while.” Write down the dose and how often you take it.
- Use one pharmacy for all your prescriptions. Pharmacies have systems that check for interactions. If you spread your prescriptions across multiple pharmacies, those systems can’t help you.
- Ask your pharmacist about interactions. Pharmacists are trained to catch these things. In fact, they resolve 22% of all drug-related problems in the U.S. annually. But they can’t help if you don’t tell them what you’re taking.
- Time your doses. If you take levothyroxine and calcium, take them at least 4 hours apart. Same with iron and antibiotics. Even a small delay can make a big difference.
- Check grapefruit juice and other risky foods. If you’re on a statin, blood pressure med, or anti-anxiety drug, skip grapefruit. Also avoid Seville oranges, pomelos, and some types of tangerines.
- Use trusted tools. The FDA-approved GoodRx Drug Interaction Checker, Medscape’s tool, and NIH’s LiverTox database are free and reliable. Don’t rely on random apps or websites.
And if you’re on warfarin, digoxin, or any high-risk drug, ask your doctor or pharmacist: “Are there any foods, supplements, or new meds I should avoid?” Don’t wait for them to ask you. Take charge.
The Future of Medication Safety
The system is slowly improving. The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable database with over 12,000 verified interactions. AI tools like IBM Watson Health are now scanning millions of patient records to find patterns no human would spot. And pharmacogenomics-testing your genes to see how you metabolize drugs-is becoming more common. By 2026, testing for CYP450 enzyme variants may be standard before prescribing certain drugs.
But technology won’t fix everything. The biggest problem isn’t lack of data. It’s lack of communication. Patients don’t tell doctors about supplements. Specialists don’t talk to each other. Pharmacies are overwhelmed. And patients are left in the middle, guessing what’s safe.
The real solution isn’t a new app or a smarter algorithm. It’s a habit. A simple, consistent habit: Know what you’re taking. Ask about interactions. Keep a list. Share it.
Because when it comes to your medications, the safest choice isn’t always the one your doctor prescribes. It’s the one you understand.
Can over-the-counter medicines cause dangerous drug interactions?
Yes, absolutely. Many people assume OTC drugs are harmless, but that’s not true. Ibuprofen and other NSAIDs can reduce the effectiveness of blood pressure medications and increase the risk of kidney damage when taken with diuretics. Antihistamines like diphenhydramine (Benadryl) can cause dangerous drowsiness when mixed with sedatives or alcohol. Even common supplements like St. John’s Wort can make birth control pills, antidepressants, and heart medications less effective. Always check OTC meds and supplements the same way you check prescriptions.
Are herbal supplements safe to take with prescription drugs?
No, not without checking. Herbal supplements are not regulated like drugs, so their ingredients and potency can vary. St. John’s Wort can reduce the effectiveness of antidepressants, birth control, and even some cancer drugs. Garlic and ginkgo biloba can increase bleeding risk when taken with warfarin or aspirin. Turmeric may interfere with blood sugar control in diabetics. Just because something is “natural” doesn’t mean it’s safe with your meds. Always tell your pharmacist or doctor what herbal products you use.
Why do some drug interactions only show up after years of use?
Because the body changes over time. Your liver and kidneys don’t work the same at 70 as they did at 40. You might start a new medication, and for months or years, nothing happens. Then, your kidney function dips slightly due to aging or dehydration. Suddenly, a drug you’ve taken safely for years starts building up in your system. That’s why regular medication reviews are critical-even if you feel fine. What’s safe today might not be safe next year.
Do electronic health records catch all drug interactions?
No. While 89% of U.S. hospitals use electronic systems with basic interaction alerts, only 42% have advanced systems that rank severity and give clinical guidance. Many systems miss interactions with supplements, OTC drugs, or foods. They also don’t always update in real time. If you see a warning pop up, don’t ignore it-but don’t assume it’s the full picture. Always double-check with your pharmacist.
What should I do if I think I’m having a drug interaction?
Stop taking the new medication or supplement immediately, and contact your doctor or pharmacist right away. Don’t wait for symptoms to get worse. Signs of a serious interaction include unexplained dizziness, confusion, rapid heartbeat, muscle pain or weakness, unusual bleeding, or sudden swelling. If you’re on warfarin and notice blood in your urine or stool, or if you have a severe headache, go to the ER. These can be signs of internal bleeding. Your life could depend on acting fast.






15 Comments
Jocelyn Lachapelle
This is the kind of post that should be mandatory reading before you get your first prescription. I used to think supplements were harmless until my grandma ended up in the ER over St. John’s Wort and her blood thinner. Simple habits save lives.
Nupur Vimal
People in the US are so lazy they dont even read the leaflets that come with their pills and then wonder why they feel weird. In India we just take what the doctor says and dont mess around with juice or herbs
Sai Nguyen
This is why America is falling apart. You let people take whatever they want and then act shocked when they get sick. No wonder your healthcare costs are insane.
RONALD Randolph
I’ve been warning people for years: grapefruit juice is a silent killer. It’s not a myth-it’s a biochemical betrayal. The FDA should ban it from hospitals. Period.
Benjamin Glover
Fascinating. Though I suspect most of these interactions are only documented because Americans overprescribe everything. In the UK, we’re far more restrained.
Michelle M
It’s not just about drugs-it’s about how we treat our own bodies as machines we can plug and play with. We forget we’re living systems, not smartphones. A pill isn’t a button press.
Cassie Henriques
CYP3A4 inhibition is the silent epidemic. The pharmacokinetic cascade from furanocoumarins to rhabdomyolysis is terrifyingly elegant. And yet, we still don’t mandate genetic screening before prescribing statins. Why?
Jake Sinatra
I work in a pharmacy. I see this every day. People bring in 12 different bottles and say, ‘I think I’m fine.’ You’re not fine. You’re one grapefruit away from ICU.
Mike Nordby
The real issue isn’t the interactions-it’s the lack of coordination between specialists. One doctor prescribes warfarin, another prescribes an antibiotic, and no one talks. Electronic records don’t fix human silence.
Raj Kumar
I'm from India and we dont have access to all these tools but we do have one thing: we ask our elders. My aunty always said, 'If you dont know, ask the pharmacist. They know more than the doctor sometimes.'
Melissa Taylor
I keep a little notebook. Prescriptions, supplements, even the ginger tea I drink daily. I show it to every provider. It’s not fancy, but it’s saved me twice.
Lisa Davies
I used to think my multivitamin was harmless 😅 Then I found out it had vitamin K and I was on warfarin. My INR went nuts. Now I check everything. You’re not being paranoid-you’re being smart 💪
John Brown
I get it. We’re busy. We trust our doctors. But if you’re on more than three meds, you owe it to yourself to be the detective. You’re the only one who knows your whole story.
Christina Bischof
i just started taking levothyroxine and i drink soy milk every morning... should i be worried?
John Samuel
As a clinical educator, I’ve trained hundreds of patients on medication safety. The single most effective tool? A handwritten list. Not an app. Not a note on your phone. A piece of paper you carry. It’s tactile, it’s unbreakable, and it forces you to confront what you’re actually taking. When patients do this, their hospitalizations drop by 40%. Not because of technology-but because of intentionality. The system is broken, but your awareness isn’t. You hold the power to be the outlier. Not the statistic.