Women's Chest Pain Symptom Checker
This tool helps you assess if your chest symptoms match the red flag indicators for heart-related issues in women. Based on information from the article, it's designed to help you make informed decisions about seeking medical attention.
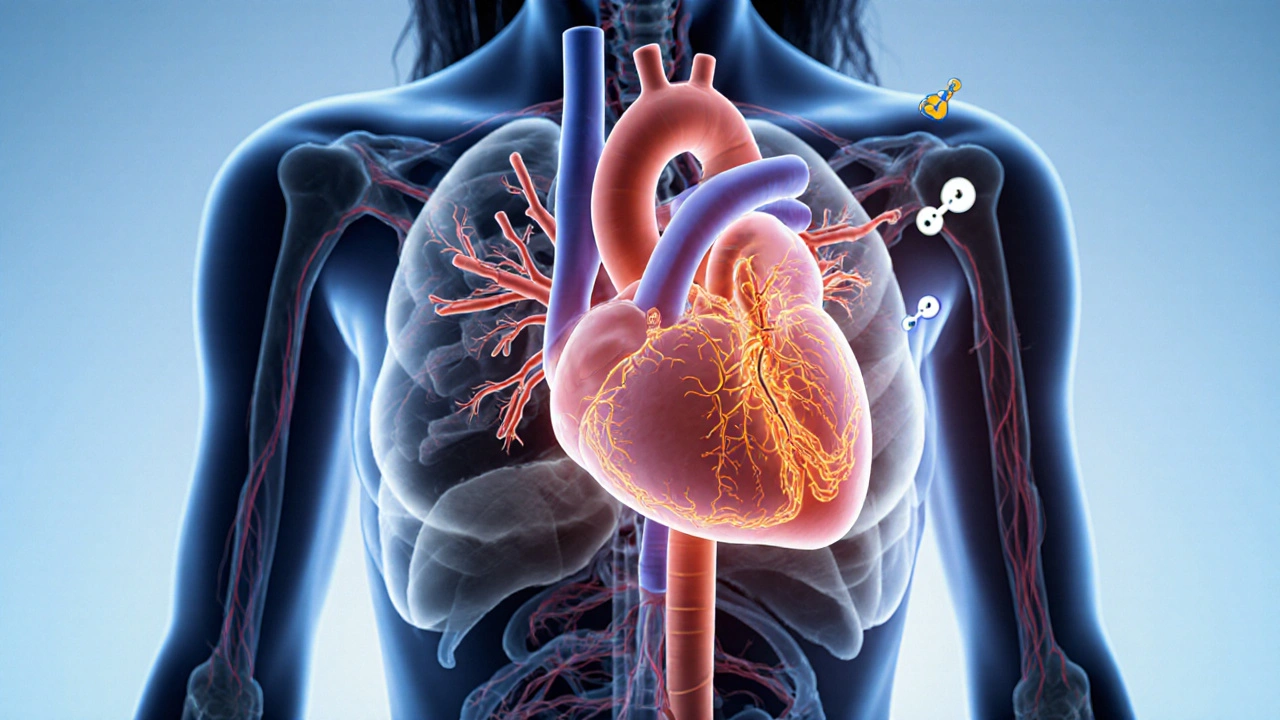
When a woman feels tightness, pressure, or any unusual sensation in her chest, the first thought is often “it’s just indigestion” or “it will pass”. But chest discomfort can signal something far more serious, and the warning signs often look different from the classic picture taught in textbooks. This guide breaks down the unique ways chest pain shows up in women, the most common underlying causes, and exactly what to do when you’re unsure.
What "Chest Pain" Really Means
Chest Pain in Women is a symptom, not a disease. It describes any uncomfortable feeling-pressure, burning, stabbing, or tightness-felt somewhere between the neck and the upper abdomen. The sensation can arise from the heart, lungs, esophagus, muscles, or even anxiety. Because many organs share the same nerve pathways, pinpointing the source often requires careful assessment.
Why Women Experience Different Symptoms
Women’s bodies process pain differently due to hormonal influences, smaller coronary arteries, and a higher prevalence of microvascular disease. Estrogen, for example, protects large vessels but can also cause subtle changes in blood flow that lead to atypical presentations. As a result, the classic “crushing chest pressure” that most men report may be replaced by vague discomfort in the back, jaw, or stomach.
Common Causes of Chest Pain in Women
Below are the most frequent culprits, each with its own hallmark features.
- Coronary Artery Disease (CAD): Buildup of plaque in the major arteries that supply the heart. Women often develop CAD later in life, and the pain may be less intense.
- Microvascular Angina: Also called cardiac syndrome X, this occurs when tiny vessels within the heart wall narrow, causing chest discomfort even though larger arteries appear clear on angiograms.
- Myocardial Infarction (heart attack): In women, a heart attack can manifest without the dramatic “wall‑of‑pain”. Symptoms may be mild, fleeting, or mistaken for indigestion.
- Gastroesophageal Reflux Disease (GERD): Acid reflux can create a burning sensation that mimics heart‑related pain, especially after meals.
- Panic Attack / Anxiety: Sudden bouts of intense fear trigger rapid breathing and chest tightness, often accompanied by palpitations.
- Pericarditis: Inflammation of the heart’s lining produces sharp pain that worsens when lying down.
- Pulmonary Embolism: A blood clot lodged in a lung artery causes sudden, severe chest pain and shortness of breath.
Atypical Symptoms Women Should Not Ignore
Because the pain can be subtle, women should treat the following signs as possible cardiac warnings:
- Discomfort in the jaw, neck, or upper back
- Nausea, vomiting, or a sudden urge to eat “something bland”
- Unexplained fatigue or light‑headedness lasting more than a few minutes
- Shortness of breath that feels out of proportion to activity level
- Cold sweats or a feeling of “being out of breath” even while resting
Risk Factors Unique to Women
Some conditions make women especially prone to chest pain that stems from heart disease.
- Hormonal shifts: Pregnancy, menopause, and oral contraceptives can alter cholesterol and blood‑clotting profiles.
- Diabetes: Women with diabetes lose the protective effect of estrogen on blood vessels faster, raising CAD risk.
- Autoimmune diseases like lupus and rheumatoid arthritis increase inflammation in blood vessels.
- Family history of early heart disease-especially a mother or sister-elevates personal risk.
When to Call an Ambulance: Red‑Flag Checklist
Even if you suspect the pain is non‑cardiac, it’s safer to err on the side of caution. Call emergency services (999 in the UK) if you experience any of the following:
- Chest pain lasting more than 5 minutes or recurring
- Sudden, severe shortness of breath
- Loss of consciousness or fainting
- Radiating pain to the arm, back, jaw, or neck
- Profuse sweating, nausea, or vomiting alongside the pain
Diagnostic Tools Doctors Use
Once you’re in a medical setting, clinicians rely on a series of tests to determine the cause.
- Electrocardiogram (ECG): Records the heart’s electrical activity. Certain pattern changes can hint at a heart attack even when pain is mild.
- Blood troponin levels: Elevated troponin indicates heart muscle damage.
- Coronary CT angiography: Gives a detailed view of both large and small coronary vessels, useful for spotting microvascular disease.
- Stress testing (exercise or pharmacologic): Reveals how the heart responds under load.
- Upper endoscopy or esophageal pH monitoring: Rules out GERD when cardiac tests are normal.
Prevention & Lifestyle Strategies
Much of the risk can be lowered with daily habits that support cardiovascular health.
- Heart‑healthy diet: Emphasize leafy greens, berries, whole grains, and omega‑3‑rich fish. Limit saturated fats and sugary drinks.
- Regular exercise: Aim for at least 150 minutes of moderate‑intensity activity per week-walking, cycling, or swimming all count.
- Stress reduction: Mindfulness, yoga, or even a short daily walk can curb anxiety‑related chest pain.
- Quit smoking and moderate alcohol intake-both dramatically cut CAD risk.
- Routine health checks: Blood pressure, cholesterol, and blood sugar screening every year, especially after age 40.
Quick Reference Checklist
- Know the women chest pain red‑flag symptoms (jaw pain, nausea, sudden fatigue).
- Call 999 if pain lasts >5 minutes, spreads, or is accompanied by breathlessness.
- Ask your doctor about a stress test if you have risk factors like diabetes or a family history.
- Track diet, exercise, and stress levels-small changes make big differences.
- Schedule annual cardiovascular screening, even if you feel fine.
Comparison: Typical Chest Pain Symptoms - Men vs. Women
| Symptom | Men (Typical) | Women (Typical) |
|---|---|---|
| Pain quality | Heavy, crushing pressure | Pressure, tightness, or burning |
| Radiation | Left arm, jaw, neck | Upper back, right arm, jaw, throat |
| Associated feelings | Sudden onset, intense | Nausea, shortness of breath, sweating |
| Duration | Minutes to hours | Short episodes, may come and go |
| Trigger | Physical exertion | Emotional stress, hormonal changes |
Final Thoughts
The bottom line is simple: if you’re a woman and you feel any kind of chest discomfort that feels out of the ordinary, trust your instincts and seek medical help. Early detection saves lives, and knowing the atypical ways heart disease shows up in women puts you one step ahead of a potentially serious event.
Can stress cause chest pain that feels like a heart attack?
Yes. Acute anxiety or a panic attack can trigger tightness, rapid heartbeat, and even shortness of breath that mimic cardiac pain. The key difference is that panic‑related pain usually resolves within minutes, while cardiac pain persists or worsens.
Why do women often have “silent” heart attacks?
Women’s smaller coronary arteries and the prevalence of microvascular disease can limit the classic crushing sensation. Hormonal effects also modify pain pathways, leading to milder or atypical symptoms such as nausea, back pain, or extreme fatigue.
When should I get a stress test even if my ECG looks normal?
If you have risk factors-diabetes, family history, or unexplained chest discomfort-your doctor may recommend a stress test to uncover hidden blockages or microvascular dysfunction that an ECG at rest can miss.
Can heart‑related chest pain be confused with GERD?
Absolutely. Both conditions can cause burning chest pain after meals. However, heart pain is more often triggered by exertion or emotional stress, while GERD pain worsens when lying flat and improves with antacids.
What lifestyle changes have the biggest impact on reducing chest pain risk?
Regular aerobic exercise, a Mediterranean‑style diet, quitting smoking, and managing blood pressure and cholesterol are the top three evidence‑based actions that lower the likelihood of heart‑related chest pain in women.







11 Comments
Danielle St. Marie
Honestly, if you still think this “chest tightness” is just indigestion you’re stuck in the Dark Ages 🇺🇸🚫💔. Women deserve cutting‑edge info, not outdated myths. The article finally gives us the real drill‑down, but let’s not forget how many people ignore the red‑flags because they were taught the male textbook. Wake up, ladies, and demand proper screening. 🩺✨
keerthi yeligay
Its a good reminder that our bodies talk in riddles; listening is key. pay attention to jaw or back pain, not just the chest. the guide hits the spot.
Bonnie Lin
Thanks for the clear checklist it helps me track symptoms without feeling overwhelmed
sara fanisha
Love how this breaks the scary stuff into doable steps – keep listening to your body and don’t be afraid to call for help.
Tristram Torres
People who skip the doctor because they think it’s just stress end up paying later. It’s better to check and be safe.
Jinny Shin
Oh dear, the tragedy of neglect! One moment you brush it off, the next you’re starring in a medical drama that could have been avoided.
Abhishek Kumar
Sounds solid.
hema khatri
Really, this guide is AMAZING, it covers EVERY angle, from micro‑vascular issues, to lifestyle tweaks, to that dreaded silent heart attack, and it does so with such clarity!!! You should all read it, it’s practically a lifesaver.
Jennell Vandermolen
Great summary – especially the part about tracking diet and stress. Small daily habits really add up, and having a quick reference makes it easier to stay on top of heart health.
Mike Peuerböck
First and foremost, I want to commend the authors for assembling such a comprehensive overview of women’s chest pain; the breadth of conditions covered demonstrates a deep understanding of cardiovascular nuance. The distinction between classic male‑centric symptomology and the subtler presentations in females is articulated with clarity that many clinicians still lack. By emphasizing microvascular angina alongside traditional CAD, the piece educates readers about the hidden arteries that can betray even the healthiest‑looking patient. Moreover, the inclusion of lifestyle interventions-dietary patterns rich in omega‑3s, regular aerobic activity, and stress‑reduction techniques-provides actionable steps that go beyond mere diagnosis. I particularly appreciate the practical red‑flag checklist; it serves as an immediate decision‑making tool in both home and clinical settings. The discussion of hormonal influences, such as estrogen’s dual role in vasoprotection and vascular remodeling, adds a layer of physiological insight that enriches the narrative. Highlighting risk factors unique to women, like autoimmune conditions, ensures that high‑risk groups are not overlooked. The diagnostic algorithm presented-starting with ECG, progressing to troponin, then advanced imaging-mirrors evidence‑based pathways and demystifies the often‑confusing work‑up process. Additionally, the clear differentiation between GERD‑related burning and cardiac ischemia equips patients to communicate more effectively with their providers. The article’s tone remains balanced, avoiding alarmism while still stressing the seriousness of delayed treatment. By integrating both preventative measures and acute response guidelines, the guide embodies a holistic approach to cardiovascular health. In sum, this resource stands as a valuable educational asset for patients, caregivers, and even seasoned practitioners seeking an updated refresher. I would encourage its dissemination across primary‑care offices, community health seminars, and online platforms to maximize its impact. Let us all champion the message that women’s heart health deserves equal attention, rigorous research, and proactive care. Thank you for shedding light on a topic that has long been under‑represented in mainstream discourse.
Simon Waters
While the guide looks thorough, I can’t help but wonder who funded this research and why certain lifestyle tips are emphasized over others.