Blood Thinner Bleeding Emergency Checker
Check Your Bleeding Symptoms
Select all symptoms you're experiencing. This tool will help determine if you need immediate emergency care or can manage at home.
Select symptoms and click "Check Symptoms" to get your results.
If you’re on a blood thinner, you’ve probably worried about bleeding. Maybe you nicked your finger and it kept dripping. Or you woke up with a huge bruise and wondered if it was normal. You’re not alone. About 61% of people taking blood thinners visit the emergency room at least once because of bleeding concerns. But here’s the truth: most of those visits aren’t emergencies. The real danger isn’t the bleeding itself-it’s stopping your medication out of fear.
What Blood Thinners Do (And Why They’re Necessary)
Blood thinners-also called anticoagulants-don’t actually thin your blood. They slow down the clotting process. That’s a good thing if you have atrial fibrillation, a deep vein clot, or a mechanical heart valve. Without them, clots can form and travel to your brain, heart, or lungs. In fact, these drugs cut stroke risk by 60-70% in people with atrial fibrillation.
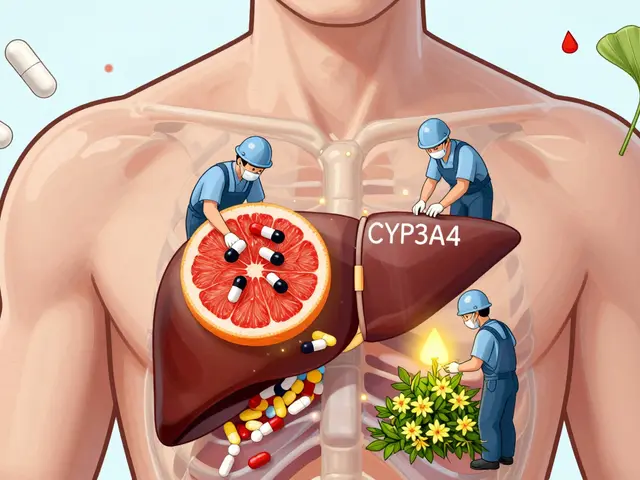
You might be taking one of these: warfarin (Coumadin), apixaban (Eliquis), dabigatran (Pradaxa), rivaroxaban (Xarelto), or enoxaparin (Lovenox). Newer ones, called DOACs, are now used in 65% of cases, replacing warfarin because they don’t need constant blood tests and have fewer food interactions. But even the safest ones carry a risk. About 3% of people on these drugs have a major bleeding event each year. That sounds scary, but it’s far less dangerous than the stroke they’re preventing.
What Counts as a Medical Emergency?
Not all bleeding is the same. Some is annoying. Some is life-threatening. Here’s what you need to know:
- Vomiting blood or coughing up blood? Go to the ER. This could mean bleeding in your stomach or lungs.
- Blood in your urine? Don’t wait. It could signal internal bleeding in your kidneys or bladder.
- Black, tarry stools? That’s digested blood from your gut. This is serious. Call 999 or get to the hospital now.
- Head injury, even if you feel fine? Go to the ER. Internal brain bleeding can take hours to show symptoms. A fall, a car accident, or even a hard bump on the head needs evaluation.
- Severe back or abdominal pain with sudden weakness? Could be bleeding behind the abdomen or into muscles. This is rare but deadly if missed.
- Uncontrolled bleeding from a cut or wound that won’t stop after 15 minutes of firm, continuous pressure? That’s your signal. Don’t check every 30 seconds. Press hard. Keep pressing. If it’s still flowing, get help.
Also, if you feel dizzy, light-headed, short of breath, or extremely tired after any bleeding-especially if you’ve lost a lot of blood-these are signs your body is going into shock. Time matters. In trauma, losing 15% of your blood volume can make you dizzy. At 30%, you’ll struggle to breathe. Don’t wait to feel worse.
What’s Just a Nuisance? (And What to Do About It)
Most bleeding on blood thinners isn’t dangerous. It’s just… messy. About 52% of ER visits by anticoagulant users are for things like nosebleeds, minor cuts, or bleeding gums. These are called “nuisance bleeding.” They’re not life-threatening, but they scare people-and that’s the problem.
Here’s how to handle common minor bleeding:
- Nosebleeds: Pinch the soft part of your nose (not the bridge) for 10-15 minutes straight. Sit up, lean slightly forward. Don’t lie down or tilt your head back. If it’s still bleeding after 30 minutes, call your doctor or go to urgent care.
- Cuts and scrapes: Apply firm pressure with a clean cloth or bandage for at least 10 minutes. Elevate the area if it’s on an arm or leg. Most will stop within 5-7 minutes. If it doesn’t, it’s time for help.
- Bleeding gums: Brush gently with a soft toothbrush. Use dental floss carefully. If it happens often, talk to your dentist. Don’t stop your blood thinner.
- Heavy menstrual bleeding: If you’re soaking through a pad or tampon every hour for several hours, call your doctor. It’s not normal and may need treatment.
- Bruising: Large, painful bruises without a clear cause? That’s common on blood thinners. But if you have bruising on your back, abdomen, or around your eyes after a minor bump, get checked.
And here’s what NOT to do: don’t use hydrogen peroxide on cuts. It damages healing tissue. Don’t take aspirin or ibuprofen for pain-those can make bleeding worse. Use paracetamol (acetaminophen) instead.
Why Stopping Your Medication Is Riskier Than the Bleeding
This is the most dangerous myth: “I had a nosebleed, so I’ll skip my pill for a few days.”
Here’s what happens when you stop: your body starts clotting again within 24-48 hours. The risk of a stroke or pulmonary embolism spikes. A study from the Michigan Anticoagulation Quality Improvement Initiative found that 68% of patients who stopped their blood thinner after minor bleeding had a clot-related event within 30 days. One Reddit user put it bluntly: “I stopped my blood thinner after a bad cut and had a PE two weeks later-don’t be like me.”
Meanwhile, the European Heart Journal found that stopping your blood thinner for just one week increases your stroke risk by 300%. That’s not a risk you can afford to take.
Instead of quitting, call your doctor or anticoagulation clinic. They can give you clear instructions. Most nuisance bleeding can be managed with a quick phone call. A 2022 study showed that patients who got structured education cut unnecessary ER visits by 37%.
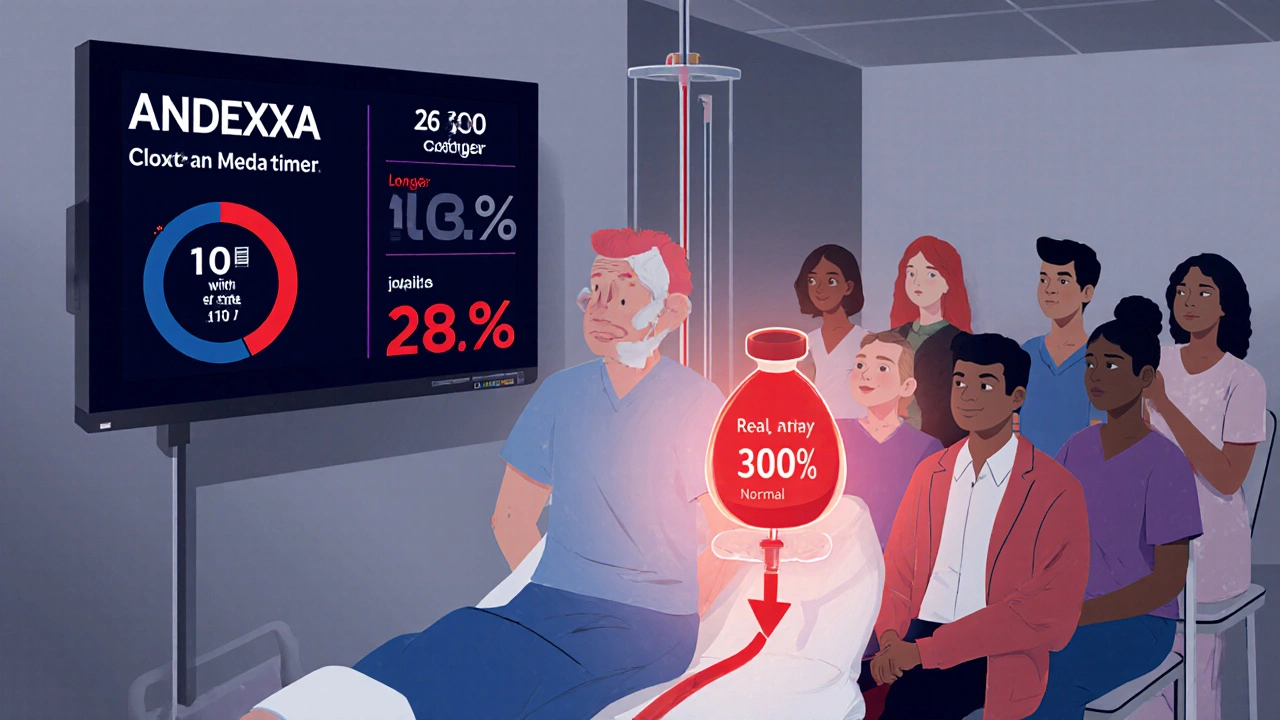
What’s New in Bleeding Management
There’s good news on the horizon. In 2023, the FDA approved andexanet alfa (Andexxa), a reversal agent that stops bleeding from apixaban and rivaroxaban in under an hour. Before this, doctors had to wait hours for the drug to wear off. Now, in emergency rooms, they can reverse the effect in 30-60 minutes.
Even better: a universal reversal agent called ciraparantag is in phase 3 trials and could be approved by 2024. It works on all blood thinners, not just one type. That’s a game-changer.
Emergency departments are also moving toward point-of-care testing. Soon, they’ll be able to check your blood’s clotting speed in minutes-not hours. This means faster, safer treatment tailored to your specific drug and dose.
But access isn’t equal. A 2022 study found Black and Hispanic patients wait 23-28% longer for reversal agents than white patients. That delay increases death risk by 15%. This isn’t just a medical issue-it’s a systemic one.
What to Do Right Now
Don’t panic. But do prepare.
- Keep a list of your blood thinner, dose, and when you last took it. Save it in your phone and carry a card.
- Know your doctor’s after-hours number or your anticoagulation clinic’s phone line.
- Have gauze, clean towels, and medical tape at home.
- Never stop your medication without talking to your provider-even if you’re scared.
- If you’re unsure whether it’s an emergency, call 111 or your GP. They can help you decide.
Most people on blood thinners live full, active lives. The key isn’t avoiding all bleeding-it’s knowing when to act, when to wait, and when to call for help. The goal isn’t to never bleed. It’s to bleed safely-and never stop taking your medicine.
Can I still get a bruise if I’m on a blood thinner?
Yes, bruising is very common on blood thinners. You might get a large, painful bruise from a bump that wouldn’t leave a mark on someone else. That’s normal. But if you have bruises on your back, abdomen, or around your eyes without a clear cause, or if they’re getting bigger and painful, get checked. It could be internal bleeding.
Should I stop my blood thinner before a dental procedure?
No, unless your doctor or dentist specifically tells you to. Most dental work-even extractions-can be done safely while you’re on blood thinners. Stopping increases your risk of stroke or clotting more than the small amount of bleeding from the procedure. Your dentist can use special techniques to control bleeding. Always tell them you’re on anticoagulants.
How long should I press on a cut before calling for help?
Apply firm, continuous pressure for at least 10 minutes. Don’t lift the bandage to check. That interrupts clotting. If it’s still bleeding after 15 minutes, go to the ER. Most cuts stop within 5-7 minutes with proper pressure. If it takes longer, you need professional help.
Is it safe to take ibuprofen or aspirin with a blood thinner?
No. Both ibuprofen and aspirin interfere with platelets and can increase bleeding risk. Use paracetamol (acetaminophen) for pain or fever instead. Always check with your doctor before taking any new medication-even over-the-counter ones.
What if I have a minor head injury but feel fine?
Go to the ER. Even if you’re not dizzy, confused, or vomiting, internal bleeding in the brain can take 24-72 hours to show symptoms. A fall, a car accident, or even a hard bump can cause a slow bleed. Better safe than sorry. Emergency scans can catch it early.
Can I still exercise or play sports on blood thinners?
Yes, but choose wisely. Avoid high-contact sports like football or boxing. Swimming, walking, cycling, and yoga are safe. Use protective gear if you’re skiing, skating, or doing anything with fall risk. Talk to your doctor about your activity level-they can help you balance safety and fitness.


8 Comments
Frank Dahlmeyer
Look, I’ve been on Xarelto for five years now, and I’ve had more nosebleeds than I can count-some so bad I thought I was dying. But here’s the thing: I’ve never had a stroke, and I won’t stop taking it just because my sinuses decided to throw a tantrum. That 68% stat? Real. My buddy stopped his meds after a minor cut and ended up with a pulmonary embolism. He’s lucky he’s alive. Don’t be that guy. Your blood thinner isn’t the enemy. Clots are. Stay calm, press hard, and keep taking your pills.
Dion Hetemi
Let’s be real-this post is just fear-mongering dressed up as medical advice. 3% major bleeding? That’s still 1 in 33 people. And you’re telling me to just ‘keep taking it’? What about quality of life? I’m not dying of a stroke-I’m dying of anxiety every time I sneeze too hard. And don’t get me started on the ER wait times. You think I’m gonna sit in a hospital for 6 hours because I nicked my thumb? Nah. I’ll just take a nap and hope for the best.
Christopher Robinson
Just wanted to add-my dad’s on Eliquis and had a huge bruise on his thigh after a bump that didn’t even hurt. We called his anticoagulation clinic, and they said ‘not unusual, monitor for swelling or pain.’ He did, and it faded in a week. Also, keep a small first aid kit with gauze and medical tape in your car and by your bed. Seriously, it’s saved me twice. And yes, paracetamol over ibuprofen. Always. 🙏
Kara Binning
Oh wow. Another ‘trust your doctor’ pamphlet. 🙄 Let me guess-you’ve never had to explain to your boss why you’re late because you were at the ER for the third time this month because your gums bled for 40 minutes? Or maybe you’ve never had to choose between paying rent or your blood test co-pay? This isn’t just ‘be careful’-it’s a financial and emotional burden wrapped in a white coat. And don’t even get me started on how long it takes to get reversal agents if you’re not white. 🤦♀️
harenee hanapi
My aunt in Delhi was on warfarin and had a nosebleed that lasted 3 hours. She panicked and stopped her meds. Two weeks later, she had a stroke. She’s now paralyzed on one side. I know this isn’t just ‘medical advice’-it’s life or death. Please, if you’re reading this and you’re thinking of skipping a dose… don’t. Call your doctor. Text them. Email them. Do anything but stop. Your life matters more than your fear.
Codie Wagers
There is a fundamental epistemological flaw in the assumption that ‘stopping the medication is riskier than bleeding’-because this presumes that the individual has perfect information, access to care, and psychological stability. In reality, most people are not rational agents in medical crises; they are terrified, sleep-deprived, and economically constrained. The system fails them long before the clot forms. The real crisis isn’t the anticoagulant-it’s the lack of accessible, compassionate, culturally competent emergency care. Until we fix that, telling people to ‘press for 15 minutes’ is just moral laziness dressed as medicine.
James Ó Nuanáin
As a British medic with 22 years in A&E, I’ve seen it all. And let me tell you: the most dangerous patients aren’t the ones bleeding-they’re the ones who stop their meds because they saw a TikTok video. 61% ER visits? Most of those could’ve been avoided with a 10-minute phone call to the anticoagulation clinic. We don’t need more panic. We need better public education. And yes-press for 15 minutes. No peeking. No checking. Just pressure. And if it doesn’t stop? Go. Don’t ‘wait and see.’ Your life isn’t a Netflix documentary. 🇬🇧🩹
Paige Lund
I just took my pill. I’m fine. ✨