Cyclosporine Interaction Risk Calculator
Cyclosporine interacts with many medications through CYP3A4 enzyme inhibition. This tool helps assess the risk of combining cyclosporine with other drugs. Select a medication below to see interaction details.
Interaction Information
Select a medication to see risk details.
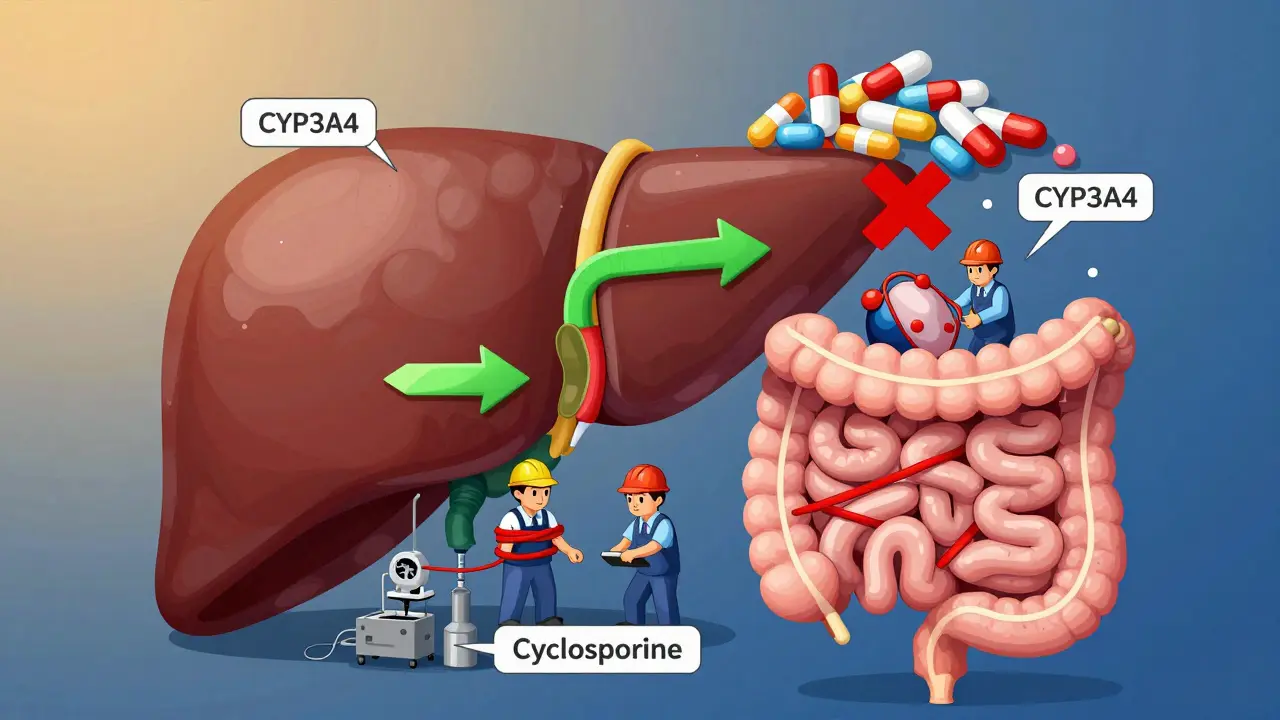
When you're taking cyclosporine after a transplant or for an autoimmune condition, the drug isn't just working on its own. It's playing a high-stakes game with dozens of other medications you might be on. The key player in this game is an enzyme called CYP3A4-and cyclosporine doesn't just get broken down by it, it actively shuts it down. This isn't a minor side effect. It's a clinical earthquake that can send your drug levels soaring-or crashing-without warning.
Why CYP3A4 Matters More Than You Think
CYP3A4 is the most common enzyme in your liver and gut. It handles about 60% of all prescription drugs you take. That means if you're on statins, blood pressure meds, antibiotics, or even some over-the-counter painkillers, CYP3A4 is likely trying to break them down. When cyclosporine comes in, it doesn't just sit there. It grabs hold of CYP3A4 and blocks it. Not temporarily. Not lightly. This is a deep, lasting interference.
Imagine a factory assembly line where CYP3A4 is the worker cleaning up leftover parts. Cyclosporine walks in, ties the worker’s hands, and says, "Don’t touch anything." Suddenly, everything else that needs cleaning piles up. That’s what happens to drugs like sirolimus, diltiazem, or even some cholesterol-lowering statins. Their levels jump-sometimes by 2 to 5 times. That’s not a small bump. It’s the difference between safe and toxic.
Cyclosporine Isn’t Just a Substrate-It’s a Saboteur
Many people think of cyclosporine as just another drug that gets metabolized. But it’s more than that. It’s both a passenger and a wrecking ball. While your body tries to clear cyclosporine using CYP3A4, cyclosporine is busy disabling that same enzyme. This dual role makes it uniquely dangerous. Unlike some drugs that only slow down metabolism, cyclosporine can cause what’s called mechanism-based inhibition. That means it doesn’t just block the enzyme-it damages it. The enzyme doesn’t just take a break; it needs to be replaced entirely. That takes days.
This is why interactions with cyclosporine don’t always show up right away. You might start a new antibiotic, feel fine for a few days, then suddenly feel dizzy, nauseous, or notice your kidneys struggling. By then, cyclosporine has already turned off enough CYP3A4 to let the other drug build up to toxic levels.
What Drugs Are Most at Risk?
Some medications are like walking into a crowded room and shouting. They’re so sensitive to CYP3A4 changes that even a small slowdown can cause serious problems. Here are the biggest red flags:
- Sirolimus: When taken with cyclosporine, sirolimus levels can jump by over 200%. Doses often need to be cut by 70% or more.
- Diltiazem and verapamil: These heart meds are moderate CYP3A4 inhibitors themselves, but when paired with cyclosporine, they create a double blockade. Blood pressure can drop dangerously low.
- Clarithromycin and ketoconazole: Strong inhibitors that can cause cyclosporine levels to spike even higher. One study showed kidney function dropping 40-60% in transplant patients within 72 hours of starting clarithromycin.
- Statins like simvastatin and atorvastatin: These can lead to muscle damage (rhabdomyolysis) when levels climb too high. Atorvastatin is safer than simvastatin, but still risky.
- Some cancer drugs: Like vinca alkaloids (vincristine) or tyrosine kinase inhibitors. These have narrow safety margins and can cause severe toxicity.
And it’s not just about what you take-it’s about what you stop. If you quit a CYP3A4 inducer like rifampin (used for TB), your cyclosporine levels can suddenly double. That’s a rejection risk waiting to happen.
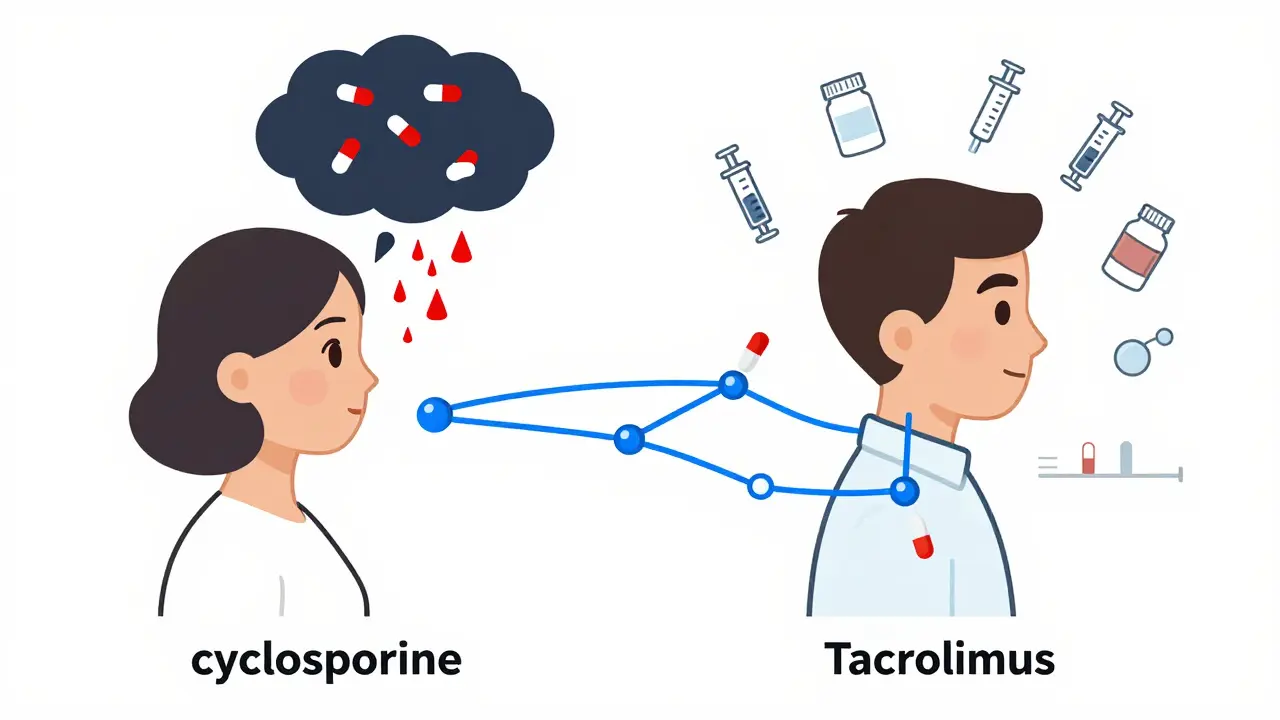
Cyclosporine vs. Tacrolimus: The Hidden Difference
Many patients get switched from cyclosporine to tacrolimus because it’s seen as "better." But here’s the catch: tacrolimus is mostly a target of CYP3A4, not an inhibitor. That means if you take a CYP3A4 inhibitor like grapefruit juice or clarithromycin, your tacrolimus levels will rise. But tacrolimus won’t cause the same ripple effect on other drugs.
Cyclosporine? It’s the one turning off the enzyme for everyone else. That’s why two patients on different immunosuppressants can have completely different interaction profiles-even if they’re on the same extra meds. One might be fine; the other could end up in the hospital.
What Happens When You Mix Cyclosporine With Other Drugs?
Real-world data from transplant centers tells a scary story. A 2021 study of over 1,200 kidney transplant patients found that more than 1 in 3 had a clinically significant drug interaction involving cyclosporine in their first year. Over 8% needed hospitalization because of it.
One case involved a man on cyclosporine after a liver transplant who started taking a common antifungal for a yeast infection. Within five days, his cyclosporine levels tripled. He developed tremors, confusion, and kidney failure. He was lucky-he was caught in time. Another patient on cyclosporine and a statin developed muscle breakdown so severe he needed dialysis.
On the flip side, if you start a CYP3A4 inducer like St. John’s wort, phenytoin, or rifampin, your cyclosporine levels can drop by 50-80%. That’s not just a tweak. That’s a rejection trigger. Acute rejection can happen within days, and it’s often irreversible.
How Doctors Manage These Interactions
There’s no magic pill to fix this. It’s all about control: monitoring, adjusting, and timing.
- Therapeutic drug monitoring is non-negotiable. Trough levels of cyclosporine are checked regularly-often weekly when starting or stopping another drug.
- Dose adjustments follow clear patterns: if you add a moderate inhibitor like diltiazem, reduce cyclosporine by 25-50%. If you add a strong one like clarithromycin, cut it by 50-75%.
- Timing matters. If you must take a CYP3A4 inhibitor, doctors may stagger doses or switch to a safer alternative like azithromycin instead of clarithromycin.
- Pharmacogenetic testing is becoming more common. Some people have genetic variants of CYP3A4 that make them slow metabolizers. For them, even low doses of cyclosporine can be risky.
Transplant centers now use electronic alerts built into their systems. When a doctor tries to prescribe a risky combo, the system flags it and asks for pharmacist review. One study showed this cut adverse events by 45%.
What You Can Do Right Now
If you’re on cyclosporine, here’s your action plan:
- Make a full list of every medication you take-including supplements, herbs, and OTC drugs.
- Bring it to every appointment. Don’t assume your doctor knows what you’re taking.
- Ask: "Could this interact with my cyclosporine?" Especially if it’s a new prescription.
- Never start or stop anything without checking first. Even something as simple as grapefruit juice can be dangerous.
- Know your cyclosporine target range. For most transplant patients, it’s between 100 and 400 ng/mL. If your level is outside that, ask why.
And if you’re on other meds, ask if they’re metabolized by CYP3A4. A quick search for "[drug name] CYP3A4" will usually show you. If it’s a substrate, and you’re on cyclosporine, proceed with extreme caution.
The Future: Personalized Dosing and Real-Time Monitoring
Scientists are now building algorithms that predict your cyclosporine levels based on your genes, your other meds, your age, and even your diet. Early models are 85-90% accurate. That’s not perfect-but it’s a huge leap from guessing.
Some hospitals are testing handheld devices that can measure cyclosporine levels from a drop of blood in minutes. Right now, you wait days for lab results. In the future, you might check your level before breakfast.
For now, though, the rule stays simple: cyclosporine doesn’t play well with others. And if you’re taking it, you need to treat every new medication like a potential bomb. Check it. Test it. Adjust it. Don’t assume it’s safe.
Can I take grapefruit juice with cyclosporine?
No. Grapefruit juice is a strong CYP3A4 inhibitor. Even one glass can increase cyclosporine levels by 30-50%. This can lead to kidney damage, high blood pressure, or nerve toxicity. Avoid it completely while on cyclosporine.
Is cyclosporine still used today, or has it been replaced?
It’s still widely used, especially in pediatric transplants, certain autoimmune diseases like psoriasis and nephrotic syndrome, and in patients who can’t tolerate tacrolimus. While tacrolimus is now first-line for most adult transplants due to better long-term outcomes, cyclosporine remains a vital tool because it’s effective, affordable, and well-studied.
How often should cyclosporine levels be checked?
When you first start cyclosporine or change your dose, levels are checked daily or every other day. Once stable, checks may drop to weekly or monthly. But anytime you start or stop another medication, or if you get sick, levels must be rechecked within 3-5 days.
Can herbal supplements interact with cyclosporine?
Yes. St. John’s wort can drop cyclosporine levels by up to 50%, risking rejection. Echinacea, garlic, and green tea extract can also interfere with CYP3A4. Always tell your doctor about every supplement-even if you think it’s "natural" or "harmless."
What should I do if I miss a dose of cyclosporine?
If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Never double up. Missing doses can cause your levels to drop, increasing rejection risk. If you’re unsure, call your transplant team. Don’t guess.
Final Thought: It’s Not About Avoiding Drugs-It’s About Managing Them
Cyclosporine saves lives. But it demands respect. You can’t avoid all drug interactions-you can’t stop taking antibiotics if you get an infection. But you can control how they interact. With the right checks, the right monitoring, and the right communication, cyclosporine can still be a safe, powerful tool. The key isn’t fear. It’s awareness. And action.





13 Comments
Prachi Chauhan
So cyclosporine doesn't just sit there-it’s like a bouncer at a club, kicking out every other drug trying to get processed. I never thought of it that way. Makes sense why my nephrologist freaks out when I even mention turmeric supplements. Natural doesn't mean harmless when your body’s already on high alert.
Cecelia Alta
Oh wow. So that’s why my cousin went into kidney failure after taking that ‘miracle’ anti-inflammatory from the health food store? She swore it was ‘just herbs.’ No one told her cyclosporine turns your liver into a hostage situation. This post should be mandatory reading for anyone on immunosuppressants. Or maybe just printed and taped to every pharmacy counter. Like a warning label on a pack of cigarettes, but for your life.
Sona Chandra
How is this even legal? People are dying because doctors don’t warn them about grapefruit juice? I’m not even mad-I’m just disappointed. This isn’t medicine, it’s Russian roulette with a prescription. And don’t get me started on how pharma companies profit off this chaos while patients pay the price in dialysis bills and broken kidneys.
Alice Elanora Shepherd
Therapeutic drug monitoring is non-negotiable-but so is patient education. Too many patients assume their pharmacist knows their full regimen. They don’t. And even when they do, systems aren’t integrated. I’ve seen patients on cyclosporine prescribed azithromycin instead of clarithromycin, but then refill the wrong one because the label didn’t change. This isn’t just about science-it’s about systems failing people.
Amanda Eichstaedt
I’m a transplant nurse in Chicago. I’ve watched people lose grafts because they took St. John’s wort for ‘anxiety.’ One guy thought it was ‘just tea.’ He didn’t even know it was an herb. We’ve started handing out laminated cards with the top 5 dangerous interactions. Grapefruit juice, garlic pills, turmeric, St. John’s wort, and-surprise-red yeast rice. It’s not enough. But it’s a start. If you’re on this med, treat every new pill like a grenade with a 72-hour fuse.
laura manning
It is imperative to underscore that mechanism-based inhibition of CYP3A4 by cyclosporine is not merely a pharmacokinetic anomaly; it constitutes a profound, irreversible, and time-dependent alteration of hepatic metabolic capacity. Consequently, the concomitant administration of substrates of CYP3A4-particularly those with narrow therapeutic indices-must be subjected to rigorous, evidence-based risk stratification protocols, including serial plasma concentration monitoring, pharmacogenetic screening, and pharmacist-led intervention. Failure to adhere to these standards constitutes a breach of the standard of care.
Jay Powers
My sister’s on cyclosporine after her kidney transplant and she’s been fine for years. But she stopped taking her statin because she was scared after reading this. She’s not dumb-she just didn’t know what to do. Maybe the real issue isn’t the drugs, it’s that we don’t give people clear, simple rules. Like: ‘If it’s not on your transplant team’s approved list, don’t take it.’ End of story. No guesswork. No ‘maybe it’s okay.’ Just say no unless they say yes.
Lawrence Jung
They say tacrolimus is better but honestly it’s just a different flavor of the same poison. Everyone’s obsessed with ‘newer equals safer’ but the truth is both drugs are landmines. The real villain is the medical system that lets you walk out with a $2000/month pill and no real plan to keep you alive. And don’t even get me started on how they push these meds on kids who don’t even understand what they’re taking.
Windie Wilson
So let me get this straight… I can’t have my morning grapefruit smoothie, my turmeric latte, my garlic supplements, my OTC cold medicine, my CBD gummies, or my ‘natural’ anxiety tea… but I can take a drug that makes me shake, sweat, and look 20 years older? Thanks, medicine. You really know how to treat people like humans.
Cassie Widders
My dad’s been on cyclosporine since 2010. He doesn’t even read the labels anymore. Just takes what the doctor says. I wish I’d known this sooner. We’ve had three ER trips because of ‘random’ side effects. Turns out one was from a new brand of ibuprofen. Simple stuff. Big consequences. I’m printing this out and putting it on the fridge.
Konika Choudhury
Why do Americans make everything so complicated? In India we just take what the doctor gives and don’t ask questions. If your body can’t handle it then maybe you weren’t meant to live. This overthinking about enzymes and interactions is just fearmongering. People die from car accidents every day. Why worry about a pill?
Alex Fortwengler
Big Pharma designed this. They know cyclosporine messes with everything so they sell you more drugs to fix the side effects. That’s why your levels go up and down. They want you dependent. They don’t care if you live or die as long as you keep buying. And the FDA? They’re in the pocket. That’s why grapefruit juice is still on the market. They’d rather kill you slowly than admit the system’s broken.
Christina Widodo
One sentence: I’ve been on cyclosporine for 12 years. Never had a problem. Always asked. Always checked. Always listened. It’s not the drug-it’s the silence.