Autoimmune Amenorrhea Risk Calculator
Risk Assessment Results
| Disorder | Typical Autoantibody | How It Triggers Amenorrhea | Prevalence of Cycle Issues |
|---|---|---|---|
| Hashimoto's thyroiditis | Anti-TPO, anti-TG | Hypothyroidism lowers estrogen, raises prolactin | 30-45% |
| Type 1 diabetes | Islet cell antibodies (IA-2, GAD) | Hyperglycemia disrupts LH/FSH pulsatility | 20-35% |
| Celiac disease | Anti-tTG, anti-EMA | Malabsorption reduces leptin, impairing GnRH | 15-25% |
| Addison's disease | 21-hydroxylase antibodies | Adrenal insufficiency lowers cortisol, altering estrogen metabolism | 10-20% |
| Systemic lupus erythematosus (SLE) | ANA, anti-dsDNA | Inflammation and steroid treatment suppress ovarian function | 25-40% |
Missing periods can feel like a mystery, but for many women the culprit isn’t just stress or weight changes-it’s the immune system acting up. Understanding the link between amenorrhea and autoimmune disorders helps you spot warning signs early and take steps that protect both reproductive and overall health.
What Is Amenorrhea?
Amenorrhea is a condition where a woman of reproductive age experiences an absence of menstrual bleeding for three or more consecutive months, without pregnancy or other obvious causes. It signals a disruption in the hypothalamic‑pituitary‑ovarian (HPO) axis, the hormonal circuit that regulates the menstrual cycle. When the HPO axis falters, estrogen levels drop, fertility can decline, and bone health may suffer.
Autoimmune Disorders: A Quick Overview
Autoimmune disorders occur when the immune system mistakenly attacks the body’s own tissues, producing antibodies that damage organs or interfere with normal function. Common examples include thyroid disease, type 1 diabetes, celiac disease, and systemic lupus erythematosus. Over 80 million Americans live with an autoimmune condition, and women are disproportionately affected.
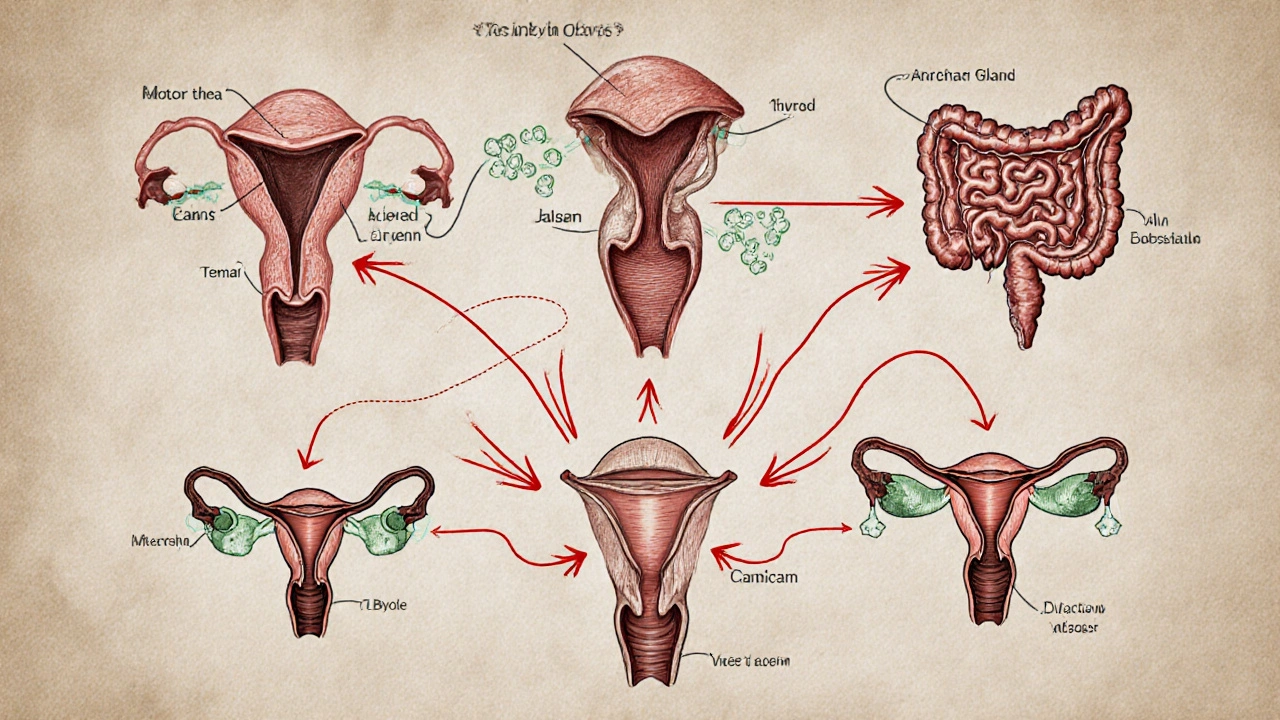
Why the Immune System Messes with the Menstrual Cycle
The connection isn’t vague-there are clear biochemical pathways linking immunity and reproduction.
- Inflammatory cytokines such as IL‑6 and TNF‑α can suppress GnRH (gonadotropin‑releasing hormone) secretion, lowering LH and FSH levels needed for ovulation.
- Autoantibodies (e.g., anti‑thyroid peroxidase) can interfere with hormone synthesis, leading to estrogen deficiency.
- Genetic factors like HLA‑DQ2/8 increase the risk of both autoimmune thyroid disease and menstrual irregularities.
When any of these mechanisms are active, the menstrual cycle can stall, resulting in amenorrhea.
Autoimmune Conditions Most Often Linked to Amenorrhea
Not every autoimmune disease affects the menstrual cycle, but several have strong epidemiological ties.
| Disorder | Typical Autoantibody | How It Triggers Amenorrhea | Prevalence of Cycle Issues* |
|---|---|---|---|
| Hashimoto's thyroiditis | Anti‑TPO, anti‑TG | Hypothyroidism lowers estrogen, raises prolactin | 30‑45% |
| Type 1 diabetes | Islet cell antibodies (IA‑2, GAD) | Hyperglycemia disrupts LH/FSH pulsatility | 20‑35% |
| Celiac disease | Anti‑tTG, anti‑EMA | Malabsorption reduces leptin, impairing GnRH | 15‑25% |
| Addison's disease | 21‑hydroxylase antibodies | Adrenal insufficiency lowers cortisol, altering estrogen metabolism | 10‑20% |
| Systemic lupus erythematosus (SLE) | ANA, anti‑dsDNA | Inflammation and steroid treatment suppress ovarian function | 25‑40% |
*Numbers reflect pooled data from recent cohort studies (2022‑2024).
How Doctors Diagnose the Overlap
When a patient presents with amenorrhea, clinicians follow a stepwise approach that now includes screening for hidden autoimmunity.
- Rule out pregnancy, breastfeeding, and obvious hormonal causes (PCOS, hyperprolactinemia).
- Order baseline labs: FSH, LH, estradiol, TSH, free T4, and cortisol.
- If thyroid or adrenal values are abnormal, test for specific antibodies (anti‑TPO, 21‑hydroxylase).
- When gastrointestinal symptoms exist, request tissue transglutaminase IgA for celiac disease.
- Consider a full autoimmune panel (ANA, anti‑dsDNA, GAD) if clinical suspicion remains high.
Imaging (pelvic ultrasound) helps rule out structural issues, while bone density scans assess long‑term estrogen deficiency effects.
Managing Amenorrhea When Autoimmunity Is the Root
Treatment targets two fronts: correcting the hormonal gap and taming the immune attack.
- Hormone replacement: Low‑dose estrogen‑progestin therapy restores menstrual bleeding and protects bone health.
- Autoimmune control: Levothyroxine for Hashimoto’s, insulin for type1 diabetes, a gluten‑free diet for celiac disease, and glucocorticoids for adrenal insufficiency all normalize hormone production.
- Lifestyle tweaks: Adequate calories, balanced micronutrients (especially iron, vitaminD, zinc), and regular moderate exercise improve leptin signaling, which supports GnRH release.
- Monitoring: Repeat menstrual calendars, quarterly hormone panels, and annual antibody titers keep progress in check.
In refractory cases, consulting an endocrinologist or a reproductive immunologist can uncover rare antibodies (e.g., anti‑ovarian) that may need immunosuppressive therapy.
Practical Tips for Women Who Suspect an Autoimmune Link
- Track your cycle with a simple app or calendar; note any sudden gaps longer than three months.
- Watch for extra‑reproductive clues: unexplained fatigue, weight fluctuations, skin changes, or gastrointestinal upset.
- Ask your primary care doctor for a thyroid panel and, if indicated, a basic autoimmune screen.
- If you already have a diagnosed autoimmune disease, discuss menstrual health during routine visits-many specialists overlook gynecologic side effects.
- Consider a nutrition consult; eliminating gluten or optimizing iodine intake can make a noticeable difference for some.
Early detection not only restores periods but also reduces long‑term risks such as osteoporosis, cardiovascular disease, and infertility.
Frequently Asked Questions
Can amenorrhea be the first sign of an autoimmune disease?
Yes. About one‑third of women with newly diagnosed Hashimoto’s thyroiditis report menstrual irregularities before any thyroid symptoms appear.
Do all autoimmune disorders cause missed periods?
No. The impact depends on how the disease interferes with hormone production or metabolism. For example, vitiligo rarely affects the menstrual cycle, while celiac disease often does due to nutrient malabsorption.
Is hormone replacement safe if I have an autoimmune condition?
In most cases, low‑dose estrogen‑progestin is well tolerated and can even improve quality of life. However, women with a history of thromboembolic events should discuss risks with their doctor.
Can lifestyle changes reverse amenorrhea caused by autoimmunity?
Lifestyle alone rarely cures the underlying immune attack, but proper nutrition, stress management, and adequate sleep can boost hormonal balance and may reduce the severity of menstrual disruptions.
Should I get screened for all autoimmune diseases if I have amenorrhea?
A targeted screen based on symptoms is more practical. Start with thyroid tests, then consider celiac serology and diabetes antibodies if other clues arise.
Understanding the immune‑reproductive crossover turns a puzzling absence of periods into a clue you can act on. By checking hormones, testing key antibodies, and partnering with the right specialists, you regain menstrual regularity and safeguard long‑term health.


14 Comments
Aparna Dheep
The disappearance of a period is more than a calendar glitch. It whispers of a body whose defenses have turned inward. Autoimmunity is a rebellion of the immune army against its own citadel. When that rebellion reaches the hormonal citadel, the HPO axis falters. Estrogen becomes a scarce resource and the cycle stalls. Thyroid antibodies act like saboteurs in the endocrine workshop. Their presence signals that the immune system is already rewriting the script of health. In Hashimoto’s the low thyroid output cranks up prolactin, a known suppressor of ovulation. Type 1 diabetes injects chaos with erratic glucose spikes that scramble LH and FSH pulses. Celiac disease steals nutrients, leaves leptin low, and gnaws at GnRH release. The adrenal glands, when attacked in Addison’s, lower cortisol and disturb the estrogen metabolism pathway. Lupus drags steroids and inflammation into the ovarian arena, muffling follicular growth. The pattern is clear: immune misdirection leads to hormonal miscommunication. Recognizing the pattern early can turn a mystery into a manageable condition. So the next time a period vanishes, ask the immune system if it is sending a covert signal.
Nicole Powell
The article tries to sound scientific but it drowns in jargon that most readers can’t parse. It pretends that every autoimmune link is a groundbreaking revelation. In reality the connections have been documented for decades. The writer should cut the fluff and give plain advice. Readers deserve clear facts, not a pretentious lecture.
Ananthu Selvan
Enough with the textbook fluff. This is just another way to scare women into endless testing. If you’re not already on meds, stop worrying.
Nicole Chabot
Wow this really opened my eyes to how the immune system can hijack the menstrual cycle. I never thought thyroid issues could raise prolactin that much. The stepwise diagnostic list is super helpful. Thanks for breaking it down in a friendly way.
Sandra Maurais
From a clinical standpoint the outlined algorithm aligns with current endocrine guidelines; however, the omission of bone density assessment is a significant oversight 🧐. Integrating DXA scans early could preempt osteopenia in this cohort. Additionally, the risk stratification could benefit from a weighted scoring system rather than a binary threshold. 📊
Michelle Adamick
Team, crank up that gluten‑free protocol and watch those leptin levels bounce back! 🚀 Optimization mode: activated.
Edward Glasscote
I’ve seen a few friends deal with this and a steady diet helped more than pills sometimes. Just keep an eye on your cycle and get labs when something feels off.
Gaurav Joshi
Actually, relying on diet alone is a myth; without immunosuppression the underlying autoimmunity persists and cycles will keep stalling.
Jennifer Castaneda
The medical community conveniently downplays the role of environmental toxins in triggering autoimmunity, yet they bombard us with chemicals that masquerade as hormones. Secret agendas push pharmaceuticals while silencing natural interventions. It’s no coincidence that the rise in amenorrhea aligns with increased industrial waste. Stay vigilant and question the sources of your supplements.
Annie Eun
Oh the intrigue! Imagine a hidden network pulling strings behind every missed period, turning bodies into battlegrounds. Yet amidst the drama, science still offers tangible steps: test, treat, and trust your body’s whispers.
Jay Kay
Here’s the quick rundown: check TSH, anti‑TPO, fasting glucose, and tissue transglutaminase. If any are off, that’s your cue to start targeted therapy. Nothing more complicated than that.
Franco WR
I totally get how overwhelming it feels when your body stops its monthly rhythm and the doctors throw a laundry list of tests at you 😔. First, breathe and remember you’re not alone; many women walk this path and emerge stronger. Start with a comprehensive hormone panel – FSH, LH, estradiol, TSH, free T4, and cortisol – to map out the endocrine landscape 📈. Parallel to that, request an autoimmune screen focusing on anti‑TPO, anti‑TG, GAD antibodies, and tissue transglutaminase, because catching the silent culprits early makes a huge difference 🧪. If you’re diagnosed with a condition like Hashimoto’s, proper levothyroxine dosing can restore thyroid balance and often rescues the cycle 🚀. Nutrition plays a starring role too; ensure adequate calories, iron, vitamin D, and zinc, and consider a gluten‑free trial if celiac is suspected 🍞❌. Gentle, consistent exercise supports leptin signaling without triggering cortisol spikes – think yoga or brisk walks rather than HIIT marathons 🧘♀️. Keep a detailed menstrual diary and track symptoms; patterns will emerge that guide your provider. Follow up every three months with hormone rechecks and adjust therapy as needed. Remember, patience and a multidisciplinary team are your allies on this journey 🌟.
Rachelle Dodge
Life’s symphony pauses when hormones falter, but mindful tuning can restore the melody.
Gaurav Joshi
I appreciate the thorough overview and wonder how often clinicians incorporate patient‑reported stress levels into the autoimmune workup. Including psychosocial factors might enhance early detection and tailor interventions.