When someone vomits blood or passes black, tarry stools, it’s not just a scary moment-it’s a medical emergency. Upper GI bleeding can turn life-threatening in minutes, and knowing what’s happening-and what to do next-can save a life. This isn’t rare. Around 100 out of every 100,000 adults in the U.S. experience it each year. The most common culprits? peptic ulcers, esophageal varices, and erosive stomach lining. But here’s the truth: the biggest danger isn’t the bleeding itself-it’s the delay in getting the right care.
What Exactly Is Upper GI Bleeding?
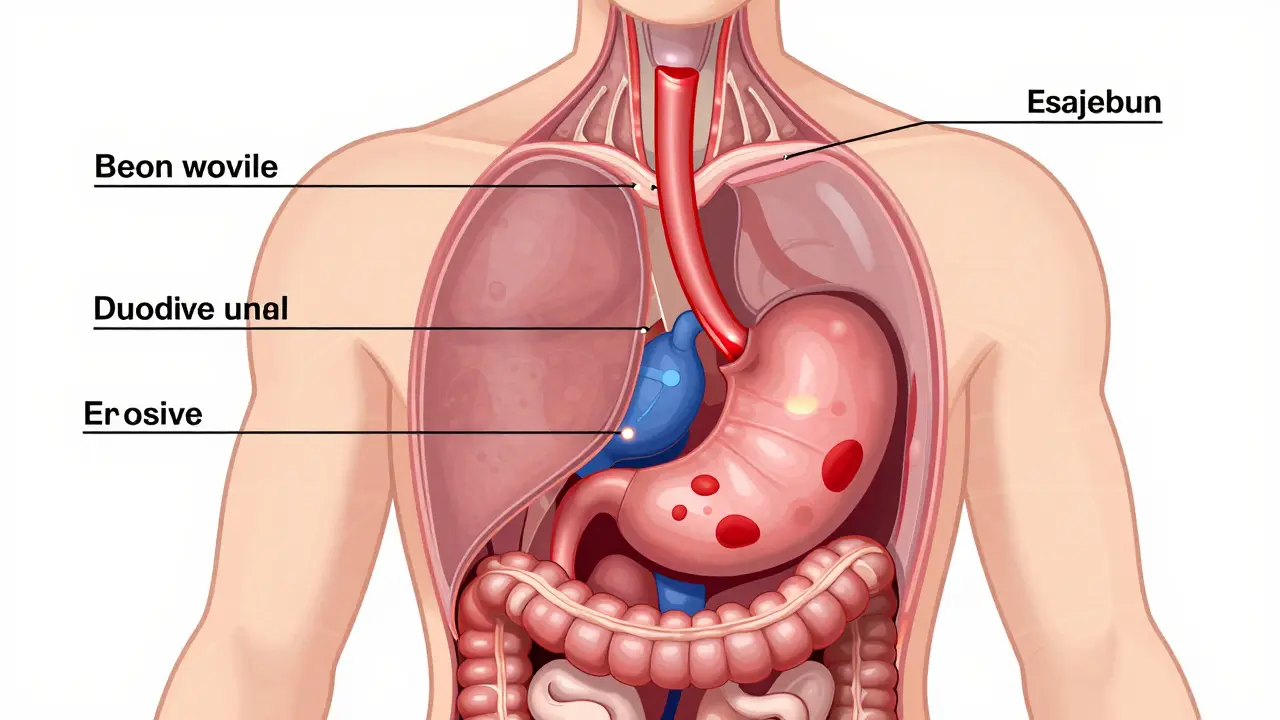
Upper gastrointestinal bleeding means blood is coming from somewhere above the ligament of Treitz-that’s the anatomical line that separates the duodenum from the rest of the small intestine. So we’re talking about the esophagus, stomach, or first part of the small intestine. The bleeding can be slow and subtle, or sudden and massive. Symptoms vary, but they’re hard to ignore: vomiting bright red blood, or material that looks like coffee grounds (that’s partially digested blood), passing black, sticky stools (melena), feeling dizzy, having a racing heart, or collapsing from low blood pressure.What makes this tricky is that some people don’t feel pain. A 78-year-old man might just feel weak and get admitted for low hemoglobin, only to find a bleeding ulcer on endoscopy. Others collapse with massive bleeding after taking an NSAID for back pain. The key is recognizing the signs before it’s too late.
The Big Three Causes: Ulcers, Varices, and More
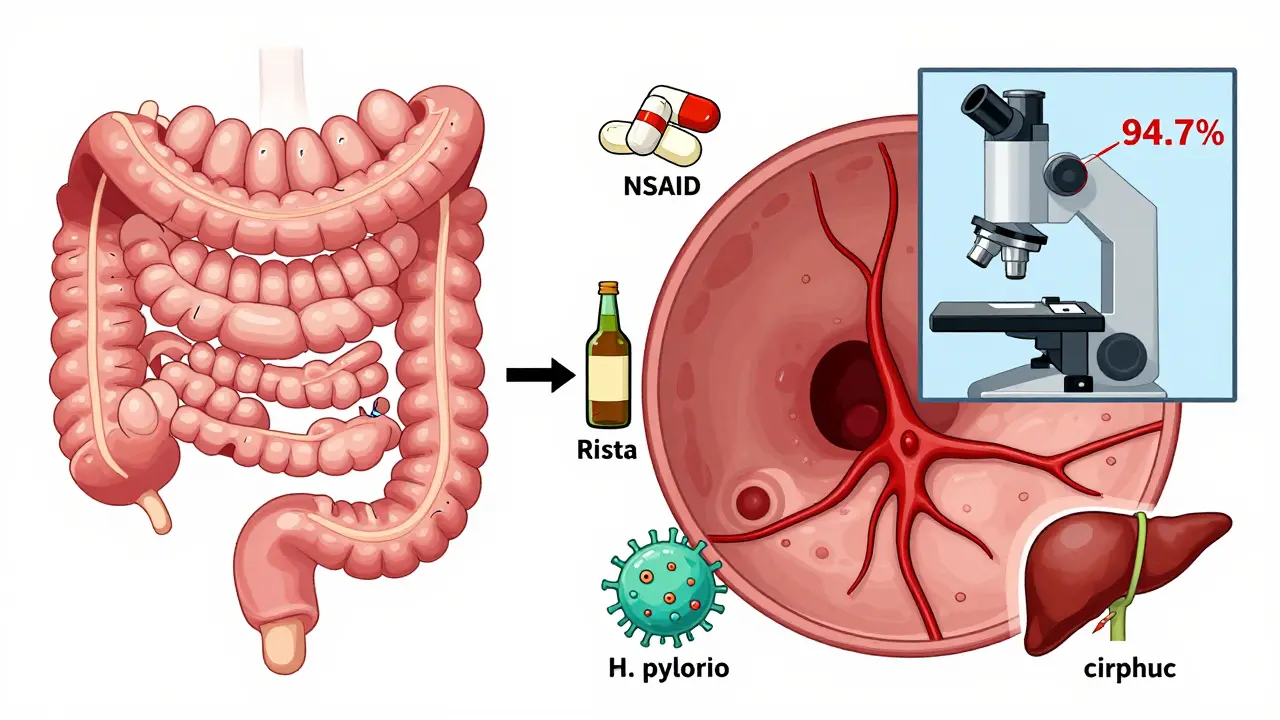
- Peptic ulcers cause 40-50% of all upper GI bleeds. These are open sores in the stomach or duodenum, often from H. pylori infection or long-term use of NSAIDs like ibuprofen or aspirin. Duodenal ulcers bleed more often than gastric ones, but both are dangerous. Studies show that patients on SSRIs have double the risk of bleeding ulcers compared to those not taking them.
- Esophageal varices account for 10-20% of cases. These are swollen veins in the esophagus, usually from advanced liver disease and portal hypertension. They’re like time bombs-thin-walled, high-pressure, and prone to rupture. Once they bleed, 20% of patients die within six weeks without treatment. Cirrhosis patients are at the highest risk.
- Erosive gastritis (15-20%) and Mallory-Weiss tears (5-10%) are also common. Gastritis comes from alcohol, stress, or bile reflux. Mallory-Weiss tears happen when violent vomiting or retching causes a tear at the junction of the esophagus and stomach.
- Other causes include tumors (2-5%), hiatal hernias (5%), and portal hypertensive gastropathy (seen in half of all advanced liver disease patients).
It’s not just about the cause-it’s about how fast you act. A bleeding ulcer can be fixed with a clip during endoscopy. A ruptured varix? Without immediate drugs and banding, the chance of dying within days skyrockets.
How Doctors Decide What to Do: The Glasgow-Blatchford Score
Not every person with melena needs an emergency endoscopy. That’s where the Glasgow-Blatchford score comes in. Developed in 2000 and updated in 2019, it’s a simple tool that uses six objective numbers to predict who needs hospitalization and urgent care:
- Hemoglobin level (below 12.9 g/dL for men, 11.9 g/dL for women)
- Systolic blood pressure (below 100 mmHg)
- Pulse rate (above 100 bpm)
- Presence of melena
- History of syncope (fainting)
- History of liver or heart disease
A score of 2 or higher means you need to go to the hospital. A score of 0? You might be safe to go home after a quick check-up. In a 2019 study of over 3,000 patients, this score correctly identified 85% of those who needed intervention. It’s not perfect, but it’s the best tool we have to avoid overtreating low-risk cases.
One study found that 15% of upper GI bleed patients can be safely managed as outpatients using this score. That means fewer hospital beds used, lower costs, and less stress for patients who don’t need them.
Diagnosis: Blood Tests and the Gold Standard-Endoscopy
When someone walks in with suspected upper GI bleeding, the first thing doctors do is check vital signs and run basic labs:
- CBC to see how low the hemoglobin is
- INR to check clotting function
- BUN-to-creatinine ratio-if it’s above 30:1, it’s 68.8% likely the bleeding is from the upper GI tract
But none of these confirm the source. That’s where esophagogastroduodenoscopy (EGD) comes in. It’s not optional-it’s mandatory. Major guidelines now say: get the scope done within 24 hours. The best outcomes? When it’s done within 12 hours. A 2022 study showed that early endoscopy cuts mortality by 25% for high-risk patients.
During the scope, doctors use the Forrest classification to grade bleeding risk:
- Class Ia - spurting blood → 90% chance of rebleeding without treatment
- Class Ib - oozing blood → 50% rebleeding risk
- Class IIa - visible vessel → 50% rebleeding risk
- Class IIb - adherent clot → 20% rebleeding risk
- Class III - no active bleeding → low risk
These aren’t just labels-they guide treatment. A Class Ia bleed needs immediate action. A Class III might just need a PPI and observation.

Treatment: What Works for Ulcers vs. Varices
There’s no one-size-fits-all treatment. The approach depends entirely on the cause.
For Non-Variceal Bleeding (Ulcers, Gastritis)
- High-dose IV PPI: An 80mg bolus, then 8mg/hour infusion. The COBALT trial showed this cuts rebleeding from 22.6% down to 11.6%.
- Endoscopic therapy: Epinephrine injection + either thermal coagulation or hemoclips. Together, they stop bleeding in 90-95% of cases.
- Hemospray: A newer option-a powder sprayed directly onto the bleeding site. It’s especially useful when the source is hard to reach. In the 2022 STOP-UGIB trial, it worked in 92% of difficult cases.
For Variceal Bleeding
- Vasoactive drugs: Terlipressin (2mg IV bolus, then every 4-6 hours) or octreotide (50mcg bolus, then 50mcg/hour). These reduce blood flow to the varices.
- Antibiotics: Ceftriaxone 1g daily. Prevents infections, which are common and deadly in cirrhosis patients.
- Band ligation: The gold standard. Rubber bands are placed around the varices during endoscopy. It cuts rebleeding from 60% to 25% compared to older methods like sclerotherapy.
Transfusion? Only if hemoglobin drops below 7g/dL or the patient is symptomatic. Don’t overdo it. Target 7-9g/dL. Each unit of packed red cells raises hemoglobin by about 1g/dL. Too much transfusion can actually worsen outcomes in liver disease.
The Stabilization Bundle: How Top Hospitals Do It Right
At Massachusetts General Hospital, they created a simple 5-step protocol called the Upper GI Bleed Bundle. Hospitals that adopted it saw dramatic improvements:
- Assess the patient within 30 minutes of arrival
- Calculate the Glasgow-Blatchford score
- Give IV PPI to high-risk patients within 1 hour
- Perform endoscopy within 12 hours for high-risk cases
- Arrange follow-up within 72 hours
Before this bundle, the average time to endoscopy was 24.5 hours. After? It dropped to 9.2 hours. Mortality fell from 8.7% to 5.3%. This isn’t magic-it’s consistency. Every step is evidence-based. Every delay costs lives.
What Patients Say: Real Stories Behind the Stats
Behind every number is a person. On Reddit’s r/GIhealth forum, users share harrowing experiences:
- u/GIwarrior99: “Woke up at 3AM coughing up coffee grounds. Went to ER. Three units of blood. Eight-day hospital stay. Ulcer from years of ibuprofen.”
- u/StomachSOS: “Doctor said my black stools were from iron pills. Two weeks later, I collapsed. Hemoglobin was 5.8.”
A 2022 University of Michigan study found that 68% of patients feared another bleed within 30 days of discharge. Nearly half changed their diet-cutting caffeine, alcohol, spicy food. A third stopped NSAIDs on their own, without asking a doctor. That’s dangerous. Self-management without guidance can lead to complications.
What’s New in 2025: AI and Personalized Risk Models
Technology is changing how we treat this. In 2023, the FDA approved Hemospray for tricky cases. In 2024, the American College of Gastroenterology will update guidelines to include AI-assisted endoscopy. In the ENDOSCAPE trial, AI detected bleeding signs with 94.7% accuracy-far better than human endoscopists at 78.3%.
But there’s a catch. AI models trained mostly on data from white patients are 15% less accurate in Black and Hispanic populations. That’s not just a technical flaw-it’s a health equity issue.
The NIH-funded UGIB-360 study, launched in early 2024, is tracking 10,000 patients to build personalized risk models using genetics, gut microbiome, and clinical history. Results are expected by late 2025. This could mean future treatments tailored not just to the bleeding source-but to the individual’s biology.
Why Timing Is Everything
Here’s the bottom line: upper GI bleeding is treatable-but only if you act fast. A delay of even 12 hours can double your risk of death. The tools are here: the Glasgow-Blatchford score, early endoscopy, targeted drugs, and AI-assisted scopes. The problem isn’t lack of knowledge-it’s lack of speed.
If you or someone you know has vomiting blood, black stools, or sudden dizziness with a racing heart-don’t wait. Don’t assume it’s indigestion. Don’t brush it off as ‘just stress.’ Go to the ER. Ask for an endoscopy. Demand a Glasgow-Blatchford score. Your life depends on it.
What does coffee-ground vomit mean?
Coffee-ground vomit means blood has been in the stomach long enough to be partially digested by stomach acid. It’s a classic sign of upper GI bleeding, often from ulcers or gastritis. It’s not a minor issue-it requires urgent medical evaluation.
Can you have upper GI bleeding without pain?
Yes. Many people, especially older adults or those on blood thinners, have no abdominal pain before a major bleed. Symptoms like dizziness, fatigue, rapid heartbeat, or black stools may be the only warning signs. Don’t wait for pain to seek help.
Is a GI bleed an emergency?
Absolutely. Upper GI bleeding can lead to shock, organ failure, or death within hours. Even slow bleeding can cause severe anemia. If you see blood in vomit or black, tarry stools, go to the emergency room immediately.
What’s the difference between melena and hematochezia?
Melena is black, sticky, tar-like stool from digested blood in the upper GI tract. Hematochezia is bright red or maroon blood in stool, usually from the lower GI tract. But in massive upper GI bleeds, blood can move too fast to be digested, so you might see hematochezia even with an upper source. Always get checked.
Can you prevent upper GI bleeding?
Yes, in many cases. Avoid long-term NSAID use without a PPI. Get tested and treated for H. pylori. Limit alcohol. Manage liver disease. If you’re on blood thinners, work with your doctor to balance risks. For those with cirrhosis, regular endoscopic screening for varices can prevent catastrophic bleeds.
How long does recovery take after an upper GI bleed?
It varies. After a simple ulcer treated with endoscopy and PPIs, most people feel better in 1-2 weeks. But full healing takes 6-8 weeks. For variceal bleeding, recovery is longer and requires ongoing treatment for liver disease. Follow-up endoscopy and medication adherence are critical to prevent rebleeding.
What Comes Next?
If you’ve had an upper GI bleed, your job doesn’t end when you leave the hospital. You need to:
- Take your PPI exactly as prescribed-don’t stop early
- Get tested for H. pylori if you haven’t already
- Stop NSAIDs unless your doctor says it’s safe
- Limit alcohol and quit smoking
- Attend all follow-up appointments, including repeat endoscopy if recommended
- Know the warning signs of rebleeding and act immediately
Rebleeding happens in 10-20% of cases within 7 days. Most of those are preventable with proper follow-up. Don’t ignore the quiet warnings-fatigue, pale skin, or mild dizziness. They’re not ‘just tiredness.’ They’re your body screaming for help.





13 Comments
Dylan Smith
Anyone else notice how they never mention that NSAIDs are often pushed by doctors as 'safe' for chronic pain when they're literally ticking time bombs for GI bleeds? I had a friend collapse after taking ibuprofen for a backache for months. No one warned him. It's not negligence, it's systemic.
Kitty Price
Thank you for this. My grandma had a bleed last year and they didn't do the endoscopy until 20 hours later. She almost didn't make it. This needs to be common knowledge 😔
Ron Williams
As someone who's worked in ER for 18 years, I can tell you the Glasgow-Blatchford score is the unsung hero here. We used to just guess who was high risk. Now we have a tool that's simple, fast, and saves lives. The fact that 15% of these patients can go home? That's huge. Less stress, less cost, better outcomes. We need more protocols like this.
Cassandra Collins
They say AI is 94% accurate but did you know the training data was mostly white people? That's why Black patients get misdiagnosed more. This isn't science-it's racism with a computer. The NIH study? Just PR. They don't want to fix the system, they want to make it look like they're trying. I've seen it. The ER won't even check for H. pylori if you're on Medicaid.
Randolph Rickman
This is gold. I'm a med student and this is exactly what we need to hear. I was just reading about Hemospray last week-it's wild that a powder can stop bleeding without clipping or cauterizing. And the fact that you don't need to transfuse unless Hb is below 7? So many docs still over-transfuse. You're right, less is more here. Keep sharing this stuff.
Josias Ariel Mahlangu
In South Africa, we don't have endoscopy machines in half the clinics. People die waiting for transport. This article reads like a luxury guide. What about those of us without access? The tools exist, but not for everyone.
sue spark
My dad had a bleed after taking aspirin daily for his heart. They told him it was fine. He didn't know it could cause this. I wish this was on every pharmacy shelf next to the painkillers. People need to know
Andrew Sychev
Of course they're pushing AI now. Big Pharma doesn't want you to know that PPIs are overprescribed and cause bone loss, kidney damage, and dementia. The real cure is gut health and stopping acid blockers. But who profits from that? Not the hospital. Not the drug companies. So they keep you scared and dependent on endoscopies and IV meds. Wake up.
Billy Poling
While the clinical guidelines presented are generally sound and evidence-based, one must not overlook the potential confounding variables inherent in observational studies cited, particularly selection bias in the COBALT and STOP-UGIB trials, as well as the lack of multivariate adjustment for comorbidities in the Glasgow-Blatchford validation cohort. Furthermore, the emphasis on early endoscopy may inadvertently lead to resource misallocation in low-volume centers where operator expertise is suboptimal, potentially increasing procedural complications. A more nuanced, risk-stratified approach to timing and resource deployment is warranted.
Mike Smith
Let me say this clearly: if you're reading this and you've ever had black stools or vomited anything resembling coffee grounds-go to the ER. Don't text your friend. Don't Google it. Don't wait until morning. Go now. This isn't hype. This isn't fearmongering. This is medicine. And the difference between acting fast and waiting is the difference between life and death. I've seen both outcomes. Choose wisely.
James Rayner
It's strange, isn't it? We have the tools to save lives, yet we still treat this like it's a mystery. We're so focused on the technical fix-the endoscopy, the clip, the band-it's easy to forget the human part. The fear. The shame. The loneliness of realizing your body betrayed you. The guilt of ignoring the warning signs. The article gives us the science. But the real work? That's in the quiet conversations after the lights dim in the ER. That's where healing begins.
Colleen Bigelow
They're hiding the truth. NSAIDs are banned in Europe for seniors over 65. But here? We're told to take them daily. Why? Because the FDA is bought by Big Pharma. And the GI bleed stats? They're underreported because hospitals don't want to admit how many patients they kill with careless prescriptions. This is a cover-up. And the AI? Just another distraction so we don't ask who's really responsible.
Kim Hines
I'm a nurse. I've seen this too many times. The worst part isn't the bleeding. It's the patients who come back a month later because they stopped their PPI because they 'felt fine.' You don't feel fine. You're just not bleeding yet. Please. Don't do that.