When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck-it’s the result of a rigorous scientific process called a bioequivalence study. These studies are the backbone of generic drug approval worldwide. They don’t test if a drug cures a disease-they prove it behaves the same way in your body as the original. Without them, generic drugs wouldn’t be safe or reliable. And without generic drugs, healthcare systems would be billions of dollars heavier each year.
Why Bioequivalence Studies Exist
The goal is simple: prove that a generic drug delivers the same amount of active ingredient into your bloodstream at the same speed as the brand-name drug. It’s not about whether the pill looks the same or tastes the same. It’s about what happens once it’s swallowed. If the body absorbs it differently, the drug might not work-or worse, it could cause side effects. That’s why regulators like the U.S. FDA, the European Medicines Agency (EMA), and Japan’s PMDA require this proof before any generic drug hits the market.The system was built on the 1984 Hatch-Waxman Act in the U.S., which created a faster, cheaper path for generics. Instead of running full clinical trials, manufacturers only had to show bioequivalence. Since then, over 95% of generic applications have passed this test. The FDA estimates that between 2010 and 2019, generic drugs saved the U.S. healthcare system $1.68 trillion. That’s the real-world value of bioequivalence studies.
The Standard Study Design: Crossover Trials
Most bioequivalence studies use a crossover design. Here’s how it works:- 24 to 32 healthy volunteers are enrolled. Sometimes more-up to 100-if the drug is highly variable.
- Each volunteer gets the brand-name drug (reference) in one period and the generic (test) in another.
- The order is randomized: half get the brand first, half get the generic first.
- There’s a washout period between doses-usually five times the drug’s elimination half-life. For example, if the drug clears the body in 12 hours, volunteers wait at least 60 hours before taking the second version.
This design cancels out individual differences. If one person naturally absorbs drugs slowly, they’re compared to themselves-not to someone else. That makes the results much more accurate.
For drugs with very unpredictable absorption (like warfarin or clopidogrel), regulators allow more complex designs: four-period replicate studies. These involve multiple doses of both products to better measure variability. The EMA and FDA have specific rules for these cases.
How Blood Samples Are Taken
After each dose, volunteers give blood samples at specific times. This isn’t random. It’s a precise schedule designed to capture the full journey of the drug through the body.At least seven time points are collected:
- Before dosing (time zero)
- Just before the peak concentration (Cmax)
- Two samples around the peak
- Three samples during the elimination phase
The last sample must be taken far enough out so that the area under the curve (AUCt) represents at least 80% of the total exposure (AUC∞). For most drugs, that means sampling for 3 to 5 half-lives. For long-acting drugs like some antidepressants or blood thinners, sampling can stretch over 72 hours or more.
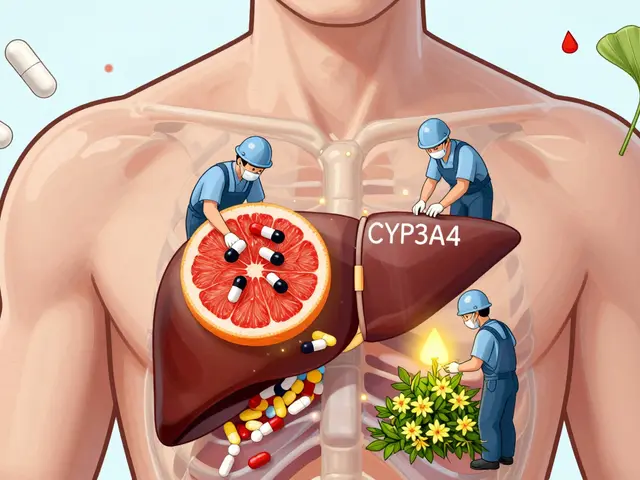
Plasma or serum is used-not whole blood. The samples are analyzed using LC-MS/MS (liquid chromatography-tandem mass spectrometry), the gold standard. The method must be validated to ensure accuracy within ±15% (±20% at the lowest detectable level), as required by the FDA’s Bioanalytical Method Validation Guidance.
The Key Numbers: Cmax and AUC
Two numbers tell the whole story:- Cmax: The highest concentration of the drug in the blood. This tells you how fast the drug is absorbed.
- AUC(0-t): The total exposure over time, from dose to last measurable concentration. AUC(0-∞) is used if the full elimination curve is captured.
These values are log-transformed before analysis. Why? Because drug concentrations in the blood don’t follow a straight line-they’re exponential. Log transformation makes the math work properly.
The data goes into a statistical model called ANOVA. It accounts for sequence (who got which drug first), period (when they got it), and individual differences between volunteers. The result? A 90% confidence interval for the ratio of test to reference.

The Acceptance Criteria: 80%-125%
This is the make-or-break rule:For both Cmax and AUC, the 90% confidence interval of the test/reference ratio must fall between 80.00% and 125.00%. If it doesn’t, the study fails.
There’s one exception: narrow therapeutic index (NTI) drugs. These are medicines where even a small difference can be dangerous-think warfarin, levothyroxine, or phenytoin. For these, the window tightens to 90.00%-111.11%, as specified in the FDA’s 2019 guidance.
These numbers aren’t arbitrary. They’re based on decades of clinical data and statistical modeling. Dr. Donald Schuirmann’s 1992 paper laid the foundation for this approach, and it’s now used globally.
What Happens If the Study Fails?
Failure is more common than you think. Around 35% of early attempts don’t pass, especially for complex formulations like extended-release tablets or injectables.Common reasons for failure:
- Washout period too short-residual drug from the first dose interferes with the second.
- Sampling schedule misses the peak concentration.
- Statistical analysis uses the wrong model or doesn’t account for carryover.
- The analytical method isn’t sensitive enough to detect low concentrations.
One Reddit user, a clinical trial vet, shared that a study they managed had to be restarted because the washout period for a 72-hour half-life drug was only 48 hours. It cost $250,000 and three months of work.
Contract research organizations (CROs) report that 22% of studies face delays due to bioanalytical method issues. A single delay can cost over $187,000.
Success often comes down to preparation. Experts say pilot studies-small versions of the main study-are non-negotiable. When used, they cut failure rates from 35% to under 10%.
Other Ways to Prove Bioequivalence
While pharmacokinetic studies (blood tests) are used in 95% of cases, there are alternatives:- Pharmacodynamic studies: Measure the drug’s effect, not its concentration. For example, measuring blood clotting time for anticoagulants.
- Clinical endpoint studies: Directly compare outcomes, like pain relief or tumor shrinkage. Required for topical creams and inhalers under FDA 2020 guidance.
- In vitro dissolution testing: For certain drugs (BCS Class I), if the tablet dissolves the same way in lab conditions, you might skip human trials entirely. This is called a biowaiver.
The FDA says you must use “the most accurate, sensitive, and reproducible approach available.” For systemic drugs, that’s almost always blood sampling.
What Makes a Good Generic Product?
It’s not just about the active ingredient. The formulation matters too.The test product must come from a commercial-scale batch-at least 1/10th of full production or 100,000 units, whichever is larger. The reference product is usually chosen from the batch with the middle dissolution profile out of three lots.
Dissolution testing is required too. The generic must dissolve similarly to the brand across pH levels 1.2 to 6.8 (mimicking the stomach and intestines). The similarity factor (f2) must be above 50, with at least 12 tablets tested per condition.
Even if the blood levels match, if the tablet doesn’t break down the same way, it might not work reliably in patients with different gut conditions.
Real-World Success and Failure
Teva’s generic version of Januvio (sitagliptin) got approved in 2021 after a single successful study with 36 subjects. That’s a win.Alembic Pharmaceuticals, however, had its generic version of Trulicity (dulaglutide) rejected in 2022. Why? Inconsistent Cmax values across multiple studies. The drug’s delivery system was too complex for the initial formulation to match.
These cases show that bioequivalence isn’t just a checkbox. It’s a deep science. A small change in excipients, particle size, or coating can throw off absorption.
What’s Changing in Bioequivalence?
The field is evolving:- Modeling and simulation (PBPK) are growing. The FDA reported a 35% increase in their use since 2020.
- Biowaivers for BCS Class I drugs now cover 27% of approvals.
- New guidance is coming for inhalers, topical products, and complex injectables.
- The FDA’s 2024-2028 plan aims to reduce study requirements by 30% using real-world data.
But regulators still stand by the current system. A 2023 FDA meta-analysis of 1,200 approved generics found no safety signals tied to bioequivalence approval. The method works.
Who Runs These Studies?
They’re run by contract research organizations (CROs) with specialized teams:- Clinical staff need 6-12 months of BE study experience.
- Biostatisticians must be trained in BE-specific ANOVA models.
- Bioanalytical labs need LC-MS/MS experts who can validate methods to FDA standards.
The FDA receives about 2,500 bioequivalence submissions each year. The median review time is just over 10 months. Companies can get feedback through GDUFA meetings-over 1,200 were held in 2022 alone.
The global bioequivalence market was worth $1.87 billion in 2022 and is growing at 7.3% per year. With over $66 billion in branded drugs set to lose patent protection between 2023 and 2025, demand will only rise.
For patients, this means more affordable options. For manufacturers, it means a clear, science-backed path to market. For regulators, it means confidence that every generic pill is as good as the original.
What is the main purpose of a bioequivalence study?
The main purpose is to prove that a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand-name drug. This ensures the generic will work the same way in the body, making it a safe and effective substitute.
Do bioequivalence studies use patients or healthy volunteers?
Most bioequivalence studies use healthy volunteers, not patients. This is because the goal is to measure how the drug behaves in the body under controlled conditions, without interference from disease. Healthy subjects provide cleaner, more consistent data for pharmacokinetic analysis.
Why is the 80%-125% range used for bioequivalence?
The 80%-125% range is based on decades of clinical data and statistical modeling. It represents the level of variation that regulators have determined won’t affect safety or effectiveness for most drugs. This range was established by experts like Dr. Donald Schuirmann and has been adopted globally because it balances scientific rigor with practicality.
Can a generic drug be approved without a human study?
Yes, for certain drugs-specifically those classified as BCS Class I (highly soluble and highly permeable). These drugs can qualify for a biowaiver, meaning they only need to pass strict in vitro dissolution testing. The FDA and EMA allow this because their absorption is predictable and not affected by formulation changes.
How long does a typical bioequivalence study take?
A standard crossover study usually takes 3 to 6 weeks from start to finish. This includes screening, dosing periods, washout, and follow-up. However, for drugs with long half-lives, the study can extend to 2-3 months. The entire approval process-from study completion to regulatory decision-typically takes 10-12 months.
What happens if a bioequivalence study fails?
If a study fails, the manufacturer must revise the formulation or study design and run another trial. Common fixes include adjusting the dosage form, changing excipients, extending the washout period, or improving sampling timing. Many companies run pilot studies first to reduce the risk of failure in the main trial.
Are bioequivalence studies the same worldwide?
The core principles are the same, but rules vary slightly. The U.S. FDA allows reference-scaled bioequivalence for highly variable drugs, while the EMA requires replicate designs. Japan’s PMDA often asks for extra dissolution testing. Still, most agencies follow ICH guidelines, so differences are narrowing.


11 Comments
Conor McNamara
they say its all science but i bet the labs just tweak the numbers till it fits 80-125%... i seen a guy get fired for saying the same thing at my cousins pharma job... they dont want you to know how much is guesswork
Leilani O'Neill
Of course the Irish system is superior. The FDA’s 80-125% rule is a joke. We’ve been doing this properly since the 1970s with actual clinical outcomes, not some statistical wizardry that ignores real-world physiology. The Americans are still stuck in the 80s.
Riohlo (Or Rio) Marie
Let’s be real - this whole bioequivalence circus is a glorified placebo test dressed up in LC-MS/MS lab coats. They don’t care if you absorb the drug differently in a gut full of inflammation or with a high-fat meal. They just want the curve to look pretty on the graph. And don’t get me started on the ‘washout’ periods - half the time volunteers are still half-drugged when they take the second dose. It’s a farce. A beautifully funded, peer-reviewed farce.
steffi walsh
This is actually so cool to read! I never realized how much science goes into making generics work. It’s like the quiet hero of affordable medicine 🙌 Keep sharing stuff like this - it makes me feel smarter just reading it!
Gabriella Jayne Bosticco
Really appreciate the breakdown. I work in clinical ops and this is one of those topics that sounds dry until you see how meticulously it’s designed. The crossover design is genius - controlling for individual variability like that is elegant science.
Sarah Frey
The rigor of this process is precisely why generic medications remain a cornerstone of global public health. The adherence to statistically validated thresholds, coupled with stringent bioanalytical validation, ensures that patient safety is never compromised in the pursuit of cost-efficiency. This is a model of regulatory excellence.
Katelyn Sykes
People don’t realize how hard it is to nail Cmax and AUC. I’ve seen studies fail because someone used the wrong centrifuge speed or the samples sat too long before freezing. It’s not magic it’s meticulous work
Also the 80-125% thing? Totally legit. If your drug’s out of range by 1% you’re basically gambling with someone’s kidneys
Gabe Solack
Big respect to the CROs and bioanalytical teams pulling this off. LC-MS/MS isn’t easy and the validation requirements are brutal 😅
Also shoutout to the volunteers - 72 hours of blood draws? That’s next level dedication 🫡
Yash Nair
USA thinks its so smart with its FDA but in India we make better generics without all this math nonsense. We use real people not lab rats. You think your 80-125% means anything when people in Mumbai take the same pill and feel different? You are blind
Bailey Sheppard
It’s wild how much goes into something most people just grab off the shelf. I used to think generics were just cheaper copies but now I see they’re basically clones with a science license. Kinda beautiful when you think about it.
Girish Pai
Per ICH Q6A and EMA Guideline on Bioequivalence, the Cmax and AUC metrics are anchored in the log-normal distribution model and require a two-way crossover ANOVA with fixed effects for sequence, period, and subject. The 90% CI must be calculated via the Satterthwaite approximation for heterogeneous variance. Failure to adhere to these specifications results in regulatory rejection under 21 CFR 320.24. The 80-125% range is not arbitrary - it’s the convergence of pharmacokinetic theory and empirical clinical outcomes across 12,000+ studies since 1992.