MS Joint Pain Symptom Checker
Answer the following questions to identify likely causes of your joint pain in relation to MS:
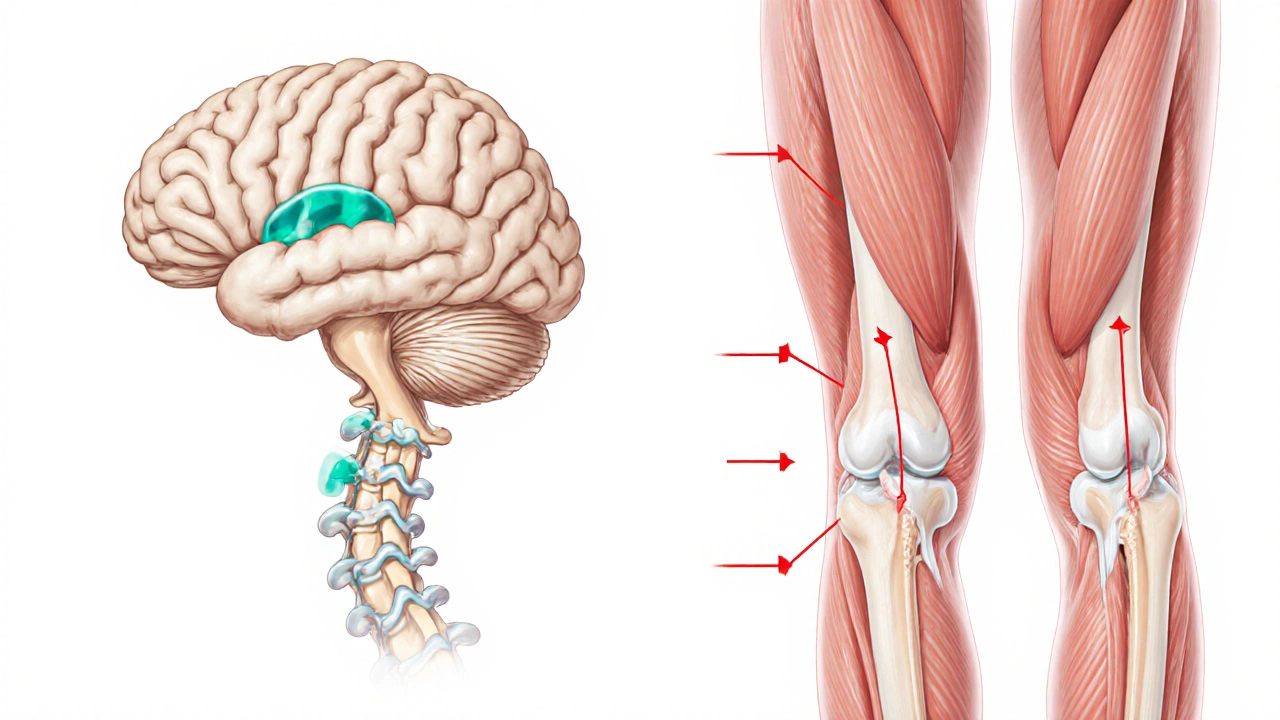
Ever wondered why some people with joint pain multiple sclerosis experience aching knees or wrists even though MS is a brain and spine disease? The link isn’t magic - it’s a mix of nerve damage, inflammation, and how the body moves. This article breaks down the science, shows how doctors figure out what’s going on, and gives practical tips to ease the discomfort.
Key Takeaways
- Joint pain in MS often stems from altered gait, spasticity, and secondary conditions like osteoarthritis.
- Distinguishing MS‑related pain from other joint disorders requires a careful medical history, neurological exam, and imaging such as MRI.
- Disease‑modifying therapies (DMTs) may lessen overall inflammation, but targeted pain management usually involves physical therapy, NSAIDs, and sometimes neuropathic pain meds.
- Early intervention with movement‑training and stretching can prevent long‑term joint damage.
- Seek specialist care if pain interferes with daily activities or is accompanied by new neurological symptoms.
What Is Joint Pain?
Joint Pain is a sensory discomfort arising from the structures that connect bones, such as cartilage, ligaments, or synovial fluid. It can feel sharp, throbbing, or achy and may worsen with movement. While it’s common in arthritis, many other factors-including nerve disorders-can trigger it.
Understanding Multiple Sclerosis
Multiple Sclerosis is a chronic autoimmune disease targeting the protective myelin sheath of nerves in the central nervous system. When myelin is damaged, electrical signals slow or stop, leading to symptoms ranging from fatigue to visual loss. MS is classified as an Autoimmune Disease that causes inflammation and scar tissue formation (sclerosis) within the brain and spinal cord.

How MS Can Spark Joint Pain
The connection isn’t direct-MS doesn’t attack joints-but several pathways create discomfort:
- Spasticity and Muscle Stiffness: Nerve lesions often cause muscles to stay tight. Persistent pull on tendons can overload joints, especially the knees, hips, and shoulders.
- Altered Gait and Mobility: To compensate for weakness or balance problems, patients may develop an abnormal walking pattern. This uneven loading stresses joint surfaces and can accelerate wear.
- Secondary Osteoarthritis: Years of compensatory movement increase the risk of degenerative joint disease, a common source of chronic pain in long‑term MS survivors.
- Inflammatory Spill‑over: Though the primary attack is on nerves, systemic immune activation can raise overall inflammatory markers, sensitizing pain pathways.
- Neuropathic Pain Overlap: MS‑related “neuropathic pain” (burning, tingling) can be felt near joints, blurring the line between joint‑origin and nerve‑origin pain.
Diagnosing Joint Pain in MS Patients
Because the causes overlap, clinicians use a stepwise approach:
- Medical History: Questions focus on pain onset, activity patterns, and any new neurological symptoms.
- Physical Examination: Neurologists assess spasticity, strength, and reflexes, while orthopedists test joint range of motion and tenderness.
- Imaging: Magnetic Resonance Imaging (MRI) provides detailed views of spinal cord lesions that might explain spasticity. X‑rays or joint‑specific MRI detect osteoarthritis or cartilage loss.
- Laboratory Tests: Blood work checks inflammatory markers like C‑reactive protein (CRP) to rule out rheumatoid arthritis.
- Specialist Referral: When pain patterns suggest neuropathic origins, a pain specialist may perform nerve conduction studies.
Management Strategies
Effective relief usually blends disease‑targeted therapy with symptom‑focused care.
Medical Options
- Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs): First‑line for mild‑to‑moderate joint inflammation.
- Acetaminophen: Safer for patients with contraindications to NSAIDs.
- Neuropathic Pain Medications: Gabapentin or pregabalin can calm burning sensations that aggravate joint discomfort.
- Disease‑Modifying Therapies (DMTs): While not designed for pain, agents like interferon‑β and dimethyl fumarate reduce overall immune activity, which may indirectly lessen inflammatory pain spikes.
- Corticosteroid Injections: For isolated, severe joint inflammation, a single intra‑articular steroid can provide weeks of relief.
Rehabilitation and Lifestyle
- Physical Therapy: A Physical Therapist designs stretching routines to reduce spasticity, strengthens stabilizing muscles, and teaches gait training to distribute forces evenly across joints.
- Assistive Devices: Canes, orthotic shoes, or ankle‑foot orthoses improve alignment and lower joint stress.
- Weight Management: Extra pounds increase load on knees and hips; modest weight loss often cuts pain scores in half.
- Low‑Impact Exercise: Swimming, stationary cycling, and yoga keep joints moving without pounding impact.
- Heat/Cold Therapy: Warm packs relax tight muscles; ice packs reduce acute swelling.
When to Escalate Care
If pain persists despite these measures, consider:
- Referral to a rheumatologist to rule out co‑existing autoimmune arthritis.
- Evaluation for surgical options (e.g., joint replacement) when structural damage is evident.
- Exploring advanced pain‑modulation techniques such as transcranial magnetic stimulation (TMS) for refractory neuropathic pain.

Future Directions in Research
Scientists are investigating whether early, aggressive DMT use can curb the cascade that leads from nerve injury to joint overload. Ongoing trials examine:
- Anti‑inflammatory biologics that target cytokines common to both MS and arthritis.
- Wearable gait‑analysis technology to predict joint stress before symptoms appear.
- Regenerative approaches, like stem‑cell injections, aimed at repairing damaged cartilage in MS patients with co‑existing osteoarthritis.
Quick Checklist for Patients
- Track when pain starts and what activities worsen it.
- Report any new numbness, weakness, or vision changes immediately.
- Maintain a regular physiotherapy schedule.
- Use appropriate footwear and consider orthotics.
- Discuss medication side‑effects with your neurologist and GP.
| Cause | MS‑Specific Factors | Typical in Non‑MS |
|---|---|---|
| Spasticity‑Induced Stress | High - muscle rigidity pulls joints | Low - absent in healthy individuals |
| Altered Gait Mechanics | Common - compensatory walking pattern | Occasional - due to injury or obesity |
| Secondary Osteoarthritis | Increased risk after years of altered movement | Age‑related wear and tear |
| Inflammatory Joint Disease | Possible overlap with other autoimmune conditions | Rheumatoid arthritis, gout, etc. |
| Neuropathic Pain Referral | High - nerve lesions mimic joint ache | Rare - usually peripheral neuropathy |
Frequently Asked Questions
Can MS directly damage my joints?
No. MS primarily attacks the central nervous system. Joint pain usually arises from secondary effects such as spasticity, altered gait, or co‑existing arthritis.
What’s the best first‑line medication for joint pain in MS?
Most clinicians start with an NSAID like ibuprofen, unless there are contraindications. If the pain has a strong neuropathic component, adding gabapentin may be advised.
Should I see a rheumatologist or a neurologist?
Begin with your neurologist, who can refer you to a rheumatologist if the joint symptoms suggest an independent joint disease.
Can exercise worsen my joint pain?
Low‑impact, guided exercise usually helps by strengthening supporting muscles and improving gait. High‑impact activities without proper technique can aggravate pain.
Do disease‑modifying therapies help with pain?
DMTs primarily target immune activity in the brain and spine. Some patients notice reduced overall inflammation, which may lessen secondary joint discomfort, but they are not a direct pain remedy.
Is joint replacement safe for someone with MS?
Yes, when medically appropriate. Surgeons coordinate with the neurologist to manage spasticity and postoperative rehab to ensure a smooth recovery.

16 Comments
Dilip Parmanand
Stay active, stretch regularly, and keep that joint pain in check!
Sarah Seddon
Hey there! I totally get how frustrating joint pain can be when you’re already dealing with MS. Think of your body like an orchestra – every instrument (or joint) needs to be tuned just right. Try adding a splash of low‑impact cardio, like swimming, to keep the rhythm smooth, and sprinkle in some gentle yoga to soothe those stiff muscles. Remember, a little color in your routine can brighten the whole day!
Ari Kusumo Wibowo
Yo, if your gait’s off, you gotta fix it now or you’ll be stuck with that ache forever. Grab a physio and get those movement patterns straight – no more excuses.
Hannah Gorman
It is a common misconception that joint pain in multiple sclerosis patients is merely a peripheral nuisance; in reality, the pathophysiology is profoundly complex. The spasticity‑induced stress on peri‑articular structures creates micro‑trauma that, over time, precipitates degenerative changes akin to secondary osteoarthritis. Moreover, altered gait biomechanics redistribute load across weight‑bearing joints, accelerating cartilage wear. One must also consider the systemic inflammatory milieu, which, while primarily directed at central nervous tissue, can sensitize nociceptive pathways, thereby amplifying perceived joint discomfort. Neuropathic pain referral further muddies the diagnostic waters, as patients often misattribute burning sensations near joints to arthritic origins. Consequently, a multidisciplinary assessment-combining neurological examination, musculoskeletal imaging, and inflammatory marker panels-is indispensable for accurate attribution. Only through such rigorous evaluation can clinicians tailor interventions that address both neurogenic and orthopedic contributors, rather than applying a one‑size‑fits‑all analgesic regimen that fails to mitigate the underlying biomechanical stressors.
Tatiana Akimova
Listen up, you need to attack that spasticity head‑on with targeted stretching and maybe a low dose of baclofen – don’t let those tight muscles wreck your joints!
Calandra Harris
MS doesn't bite joints; it simply redirects forces.
Dan Burbank
One must appreciate the subtle interplay between neurogenic spasticity and biomechanical load distribution; it is not merely a footnote in the annals of neurology but a pivotal factor that dictates the trajectory of joint integrity over decades of disease progression.
Anna Marie
I understand your concerns and recommend a coordinated approach: schedule a visit with your neurologist to discuss potential adjustments in disease‑modifying therapy, and simultaneously arrange for a physiotherapist who can implement gait‑training and muscle‑relaxation protocols. This dual strategy often yields the best outcomes for managing joint discomfort in MS.
Abdulraheem yahya
Observing the literature, we notice that many long‑term MS patients develop secondary osteoarthritis as a consequence of chronic compensatory movement patterns. When muscle spasticity forces the limb into an abnormal alignment, the joint surfaces experience uneven pressure, which over years leads to cartilage degradation. It is therefore essential to integrate regular low‑impact aerobic activity, targeted stretching, and strength training to balance muscular forces. Moreover, weight management plays a crucial role; even modest weight loss can reduce joint load substantially. Patients should also be counseled on the importance of appropriate footwear and possibly orthotic devices to correct gait irregularities. In practice, a multidisciplinary team-neurologist, physiotherapist, rheumatologist, and nutritionist-offers the most comprehensive care plan to mitigate joint pain while addressing the core neurological disease.
Preeti Sharma
Perhaps the link between MS and joint pain is overemphasized; after all, correlation does not imply causation, and many individuals with MS live pain‑free, suggesting other variables-like lifestyle or concurrent arthritis-might be the true culprits.
Ted G
What they don't tell you is that the pharmaceutical industry often downplays the role of hidden toxins that exacerbate both neuroinflammation and joint degeneration, keeping us in the dark while they profit.
Miriam Bresticker
thats realy helpful :)
Claire Willett
Integrate PT, NSAIDs, and gait analysis.
olivia guerrero
Wow, great summary, really helpful, thank you!
Dominique Jacobs
Got any tips for balancing exercise intensity with fatigue levels so we don’t overdo it?
Claire Kondash
When one contemplates the intricate tapestry of multiple sclerosis and its unforeseen reverberations upon the musculoskeletal realm, it becomes evident that the dialogue between neural degeneration and joint integrity is not a mere coincidence but a choreographed duet of pathophysiological forces. 🧠➡️🦴 The relentless demyelination that characterizes MS precipitates aberrant motor signals, which in turn manifest as spasticity-an involuntary tightness that tugs relentlessly at tendons and ligaments. This chronic tensile stress, over months and years, becomes a silent sculptor, reshaping joint architecture and prompting the cartilage to wear prematurely. Moreover, the compensatory gait adaptations that patients adopt to counterbalance weakness serve as a secondary catalyst, redistributing load patterns to previously unburdened joint surfaces. Add to this the systemic inflammatory milieu, wherein cytokines spill over beyond the central nervous system, sensitizing nociceptors and amplifying pain perception. Consequently, a patient may experience a burning, neuropathic sensation that masquerades as arthritic pain, further complicating clinical assessment. The therapeutic implication is clear: a holistic management plan must address not only the neuroinflammatory cascade with disease‑modifying agents but also the peripheral sequelae through targeted physiotherapy, orthotic support, and judicious use of analgesics. Only by acknowledging this multifaceted interplay can clinicians hope to alleviate the insidious joint discomfort that shadows many living with MS. 🌟