Hydroxychloroquine Dosage Calculator
Dosage Calculator
Enter your weight and condition to calculate appropriate hydroxychloroquine dosage. Always confirm with your prescriber.
Enter your details to calculate dosage.
Hydroxychloroquine is a synthetic antimalarial drug that also serves as an immunomodulator for autoimmune diseases. It works by interfering with lysosomal activity and reducing inflammation, making it useful for conditions like rheumatoid arthritis and systemic lupus erythematosus. Because the therapeutic window is narrow, getting the right hydroxychloroquine dosage is crucial for effectiveness and safety.
Why Correct Dosage Matters
Even a few milligrams off can tip the balance between benefit and harm. Over‑dosing raises the risk of retinal toxicity, cardiac arrhythmias, and severe gastrointestinal upset, while under‑dosing may leave the underlying disease active and cause flare‑ups. Patients often wonder how to take the pill correctly; this guide walks through the numbers, timing, and monitoring you need to stay safe.
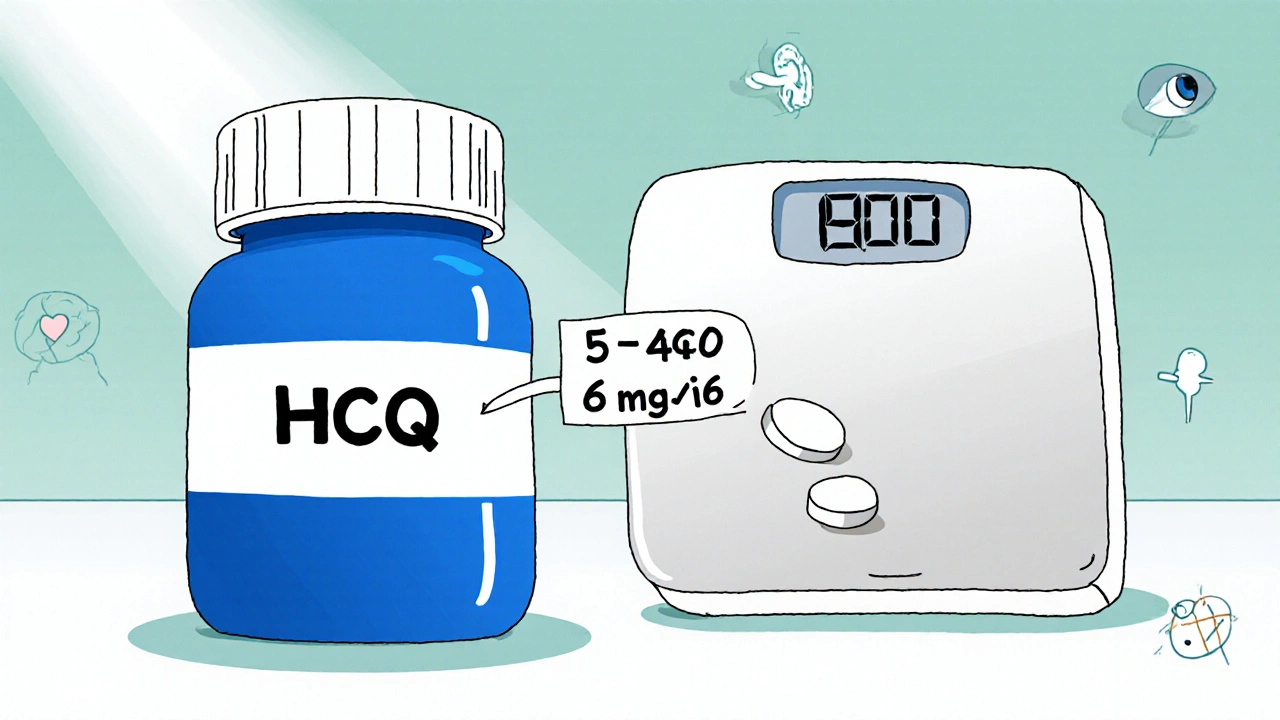
General Dosing Principles
- Weight‑based calculations: Most regimens start with a dose measured in mg per kilogram of body weight, typically 5‑6.5 mg/kg/day for chronic autoimmune therapy.
- Loading dose: Some clinicians use a short‑term higher dose (e.g., 400 mg twice daily for 1 week) to achieve therapeutic blood levels faster. This is followed by a lower maintenance dose.
- Maintenance dose: After the loading phase, the dose is reduced to a steady‑state level, usually 200‑400 mg once daily for most adults.
- Maximum daily limit: Do not exceed 6.5 mg/kg/day or 400 mg total, whichever is lower, to keep retinal risk under control.
All calculations should be confirmed by your prescriber, especially if you have a low body weight or are taking other medications that affect drug clearance.
Condition‑Specific Dosing
Below is a quick look at how dosing varies by the most common indications. The table uses typical adult values; pediatric dosing follows a similar weight‑based approach but requires pediatric‑specific guidelines.
| Indication | Loading Dose (if used) | Maintenance Dose | Notes |
|---|---|---|---|
| Rheumatoid arthritis | 400 mg twice daily for 1 week (optional) | 200‑400 mg once daily | Adjust for renal impairment; monitor liver enzymes. |
| Systemic lupus erythematosus | 400 mg twice daily for 1 week (optional) | 200‑400 mg once daily | Often combined with low‑dose steroids. |
| COVID‑19 (off‑label) | 400 mg twice daily for 5 days | 400 mg twice daily for 5 days total (no maintenance) | Use only under clinical trial or physician supervision; risk/benefit still debated. |
How to Take Hydroxychloroquine
- Take the tablet with a full glass of water.
- Preferably swallow after a meal to minimize stomach upset.
- If you miss a dose, take it as soon as you remember unless it’s close to the next scheduled dose - then skip the missed one and continue as normal. Do not double‑dose.
- Avoid antacids containing aluminum or magnesium within two hours of dosing, as they can reduce absorption.
- Do not stop abruptly without consulting your doctor; tapering may be needed after long‑term use.
Monitoring & Safety Checks
Because hydroxychloroquine can accumulate in pigmented tissues, regular monitoring is a must.
- Eye exams: Baseline retinal screening with optical coherence tomography (OCT) or fundus photography, then yearly exams after five years of use or sooner if you have risk factors.
- Kidney function: Kidney function tests (eGFR) guide dose adjustments. If eGFR falls below 30 mL/min, reduce the dose by 50 %.
- Blood work: Periodic complete blood count (CBC) and liver function tests to catch early toxicity.
- Cardiac monitoring: ECG is recommended for patients on concurrent QT‑prolonging drugs or with a history of arrhythmia.
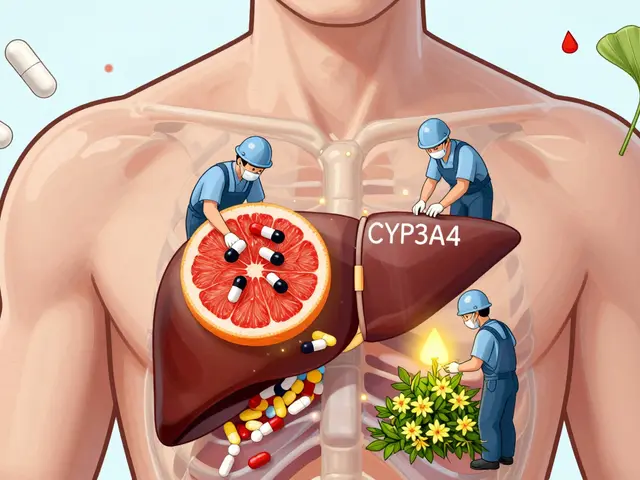
Drug Interactions to Watch
Hydroxychloroquine shares metabolic pathways with several common meds. Inform your pharmacist or prescriber about all of the following:
- Digoxin: Increases serum digoxin levels - monitor for digitalis toxicity.
- Antacids and sucralfate: Reduce absorption; separate dosing by at least two hours.
- Other QT‑prolonging agents (e.g., azithromycin, fluoroquinolones): Heightened risk of arrhythmia.
- Cytochrome P450 inhibitors (e.g., erythromycin, ketoconazole): May raise hydroxychloroquine concentrations.
Common Side Effects & What to Do
Most patients tolerate the drug well, but be on the lookout for:
- Nausea or stomach cramps: Take with food, consider a lower initial dose.
- Skin rash or itching: Discontinue and seek medical advice; could signal an allergic reaction.
- Vision changes (blurred vision, difficulty reading): Stop the medication immediately and schedule an urgent eye exam.
- Muscle weakness or tingling: Report to a clinician; may indicate neuropathy.

Special Populations
Pregnant or breastfeeding women should discuss risks versus benefits with their obstetrician. The drug crosses the placenta but is generally considered safe in standard doses for lupus. Pediatric dosing follows strict weight‑based charts and requires close ophthalmologic surveillance.
Quick Checklist for Patients
- Know your prescribed dose (mg per day) and whether you have a loading phase.
- Take the pill with food and a full glass of water.
- Schedule baseline eye exam and yearly follow‑ups.
- Get renal and liver labs every 6‑12 months.
- Carry a list of all medicines you’re taking, especially those that affect heart rhythm or digoxin.
- Report any visual changes or cardiac symptoms right away.
Frequently Asked Questions
Can I take hydroxychloroquine with food?
Yes. Taking it with a meal reduces stomach upset and helps absorption. Avoid antacids within two hours of the dose.
How often should I have eye examinations?
A baseline exam is needed before starting therapy. After five years of continuous use, yearly retinal scans are recommended, or sooner if you develop visual symptoms.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember unless the next scheduled dose is less than 4 hours away. In that case, skip the missed dose and continue with your regular schedule. Never double‑dose.
Is hydroxychloroquine safe for pregnant women?
For conditions like lupus, the benefits often outweigh the risks, and many obstetricians continue the drug at standard doses under close monitoring. Discuss any concerns with your healthcare provider.
Can hydroxychloroquine cause heart problems?
In rare cases, it can prolong the QT interval, especially when combined with other QT‑prolonging drugs. An ECG is advised if you have a heart history or are on such medications.
Do I need dose adjustments if I have kidney disease?
Yes. When eGFR is below 30 mL/min, the dose should be cut by about half, and renal function should be checked every 3‑6 months.
What are the signs of retinal toxicity?
Early signs include difficulty reading fine print, altered color perception, and seeing flashes of light. Any change should prompt an urgent ophthalmology referral.
Next Steps for Patients
If you’ve just started hydroxychloroquine, schedule your baseline eye exam within the next month and arrange a blood test to check liver and kidney function. Keep a medication diary for the first two weeks to note any side effects. And always have a copy of your dosing schedule handy-mistakes often happen when the pill bottle is out of sight.
Sticking to the plan, staying informed about monitoring, and maintaining open communication with your prescriber will help you get the most benefit from hydroxychloroquine while keeping risks low.

13 Comments
Deja Scott
Take the tablet with food and a full glass of water.
Natalie Morgan
When calculating the dose, start with the patient's weight in kilograms and aim for 5 to 6.5 mg per kilogram per day. The loading phase, if used, typically involves 400 mg twice daily for a week to reach therapeutic levels faster. After that, drop to a maintenance dose of 200 to 400 mg once daily, never exceeding 6.5 mg/kg or 400 mg total. Renal and hepatic function should be checked before adjusting the regimen.
Mahesh Upadhyay
Loading doses sound aggressive, but the risk of retinal toxicity spikes with any excess.
Rajesh Myadam
It's true that the eyes are vulnerable; regular OCT scans every year after five years can catch early changes before vision is affected.
Alex Pegg
Off‑label COVID use ignored the narrow therapeutic window and exposed patients to unnecessary cardiac risks.
laura wood
Patients should keep a detailed medication list and schedule baseline eye exams, as early detection prevents irreversible damage.
Kate McKay
Starting a new medication can feel overwhelming, especially when the dosing schedule involves loading phases and regular monitoring.
First, write down the exact milligrams you are prescribed and keep the bottle in a visible spot.
Pair each dose with a meal and a full glass of water to minimize stomach upset.
If you miss a dose, take it as soon as you remember unless the next dose is less than four hours away, then skip it.
Never double up on pills; doing so raises the chance of retinal toxicity and cardiac arrhythmias.
Schedule a baseline eye exam within the first month of therapy; this creates a reference point for future comparisons.
After five years of continuous use, plan yearly retinal scans, or sooner if you notice any visual changes.
Blood work for liver and kidney function should be drawn every six to twelve months to guide dose adjustments.
If your eGFR falls below 30 mL/min, cut the dose by about half and monitor renal labs more frequently.
When you are also taking drugs like digoxin, azithromycin, or any QT‑prolonging agents, let your doctor know so they can assess the combined risk.
Avoid antacids containing aluminum or magnesium within two hours of taking the tablet, as they can reduce absorption.
Keep a medication diary for the first two weeks; noting any nausea, rash, or visual disturbances helps your clinician fine‑tune therapy.
Remember that hydroxychloroquine can accumulate in pigmented tissues, so long‑term vigilance is key.
If you become pregnant or are planning a pregnancy, discuss the benefits and risks with your obstetrician; most specialists consider it safe at standard doses for lupus.
Children require weight‑based dosing and more frequent ophthalmologic checks, so never extrapolate adult doses for them.
Sticking to this plan, staying informed, and maintaining open communication with your healthcare team will give you the best chance of disease control with minimal side effects.
Demetri Huyler
While the checklist is thorough, seasoned clinicians know that individual variability often renders rigid protocols obsolete.
Tailoring therapy to the patient’s comorbidities supersedes any generic guideline.
JessicaAnn Sutton
Prescribing without diligent monitoring betrays the Hippocratic oath and endangers vulnerable patients.
Israel Emory
Hydroxychloroquine, when used correctly, offers substantial benefits for autoimmune patients; however, the margin between therapeutic effect and toxicity is narrow, demanding vigilant oversight.
Sebastian Green
I keep a simple spreadsheet with dates for labs and eye exams; it reduces anxiety.
Staying organized helps me stick to the monitoring schedule.
Vijaypal Yadav
Pharmacokinetic studies show that hydroxychloroquine has a half‑life of approximately 40‑50 days, which explains why dose adjustments take weeks to reflect in serum levels.
Steady‑state concentrations are typically achieved after 3‑6 months of consistent dosing.
Ron Lanham
Understanding the drug’s half‑life is crucial because it impacts both efficacy and toxicity monitoring.
A long half‑life means that accumulation can occur silently, especially in patients with reduced renal clearance.
Therefore, checking eGFR before initiating therapy and periodically thereafter helps prevent inadvertent overdose.
Moreover, the drug’s distribution into melanin‑rich tissues such as the retina accounts for the delayed onset of ocular toxicity.
Regular OCT imaging can detect subtle changes before the patient experiences visual symptoms.
If early signs appear, dose reduction by 25‑50 % often halts progression of retinal damage.
Cardiac monitoring, including baseline ECG, is advisable for anyone on concurrent QT‑prolonging medications.
The interaction with digoxin is pharmacodynamic, increasing serum levels and risk of digitalis toxicity.
Antacids, on the other hand, affect absorption and should be spaced at least two hours apart.
Patients with hepatic impairment may require lower initial doses, as metabolism is likewise compromised.
Pregnant patients should be counseled about the placental transfer, though the consensus leans toward continuation when benefits outweigh risks.
Pediatric dosing follows the same weight‑based principles but necessitates more frequent ophthalmologic surveillance.
Adherence can be bolstered by setting alarms and keeping the medication in a visible pill organizer.
Education about the importance of not abruptly stopping therapy prevents disease flare‑ups and potential rebound inflammation.
In summary, a comprehensive approach that integrates pharmacokinetic knowledge, regular monitoring, and patient education optimizes outcomes while minimizing hazards.