Heartburn Risk Calculator
This tool helps you understand your personal heartburn risk based on your food choices and medications. Based on clinical research, your risk is calculated by assessing:
- Type of spicy food consumed
- Medications you're taking
- Timing of food and medication intake
Your Personal Risk Assessment
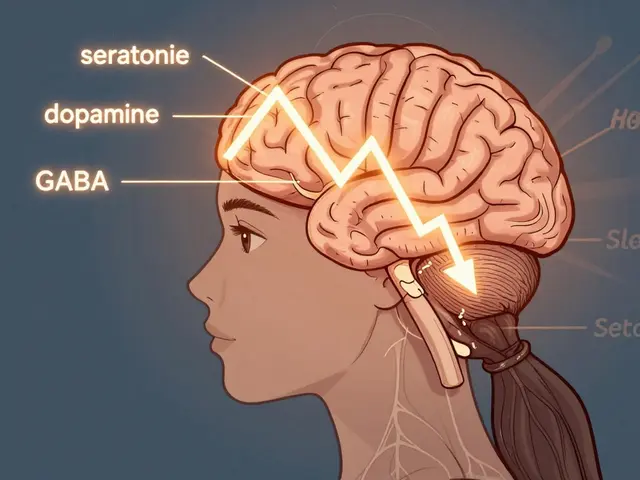
Heartburn isn’t just a nuisance after a spicy taco night-it’s a signal that something deeper is going on. If you’re taking medications like aspirin, beta blockers, or even common antacids, and you love your hot sauce, you might be setting yourself up for a cycle of discomfort that’s hard to break. The truth? Not everyone reacts the same way to spicy food or pills, but the risks are real-and manageable.
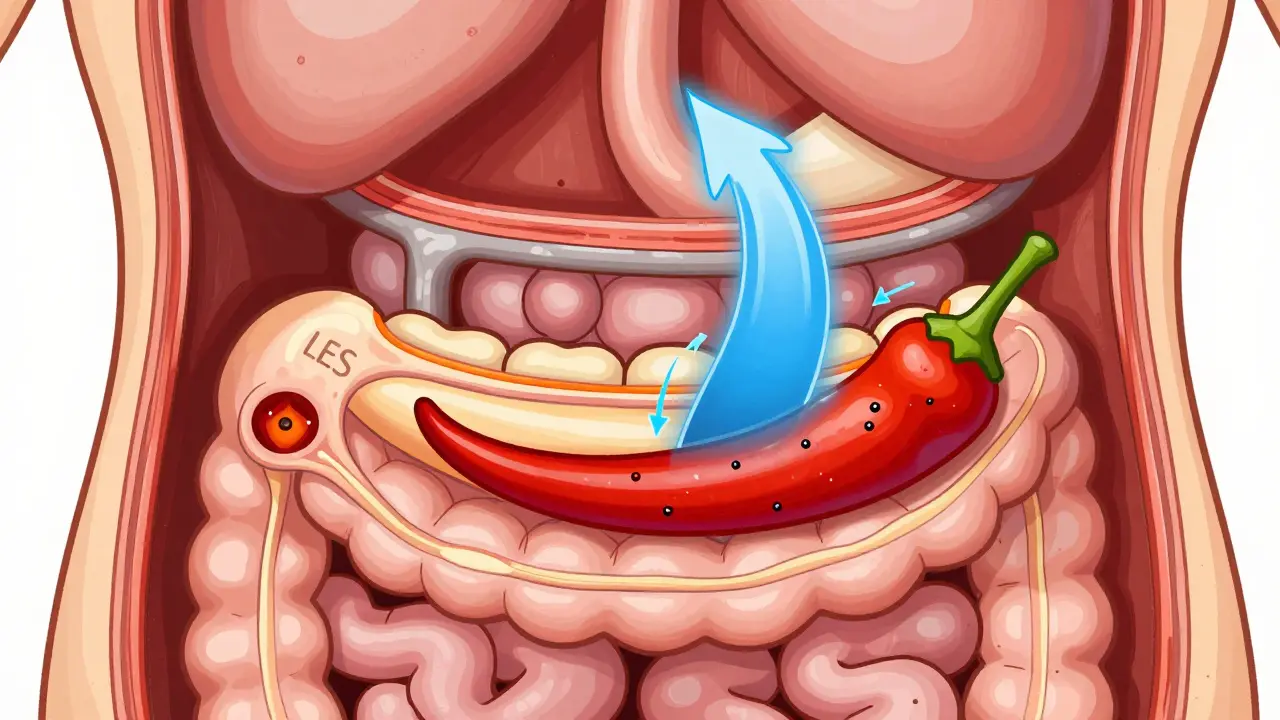
Why Spicy Food Makes Heartburn Worse
It’s not just the heat. The real culprit is capsaicin, the compound that makes chili peppers burn. Capsaicin doesn’t burn your esophagus-it relaxes the muscle that’s supposed to keep stomach acid where it belongs. That’s the lower esophageal sphincter (LES). When it loosens, acid sloshes back up, and that’s when the burning starts.
Studies show that in sensitive people, capsaicin can drop LES pressure by 30-40% within 30 minutes of eating. That’s enough for acid to creep upward, even if your stomach isn’t overfilled. And it’s not just hot peppers. Anything with cayenne, jalapeños, curry powder, or even some types of salsa can trigger this response.
But here’s the twist: not everyone is affected. A 2023 NIH review found no strong evidence that spicy food should be banned for all GERD patients. Some people eat buffalo wings daily with zero issues. Others can’t even handle a dash of paprika. The key isn’t blanket avoidance-it’s personal discovery.
Medications That Make Heartburn Worse
You might not realize your daily pills are working against you. Several common drugs directly interfere with the LES or irritate the esophagus:
- Aspirin and NSAIDs (ibuprofen, naproxen): These can cause tiny tears in the esophagus lining, leading to erosive esophagitis. Regular users see a 40-60% higher risk of GERD symptoms.
- Beta blockers (for high blood pressure): Linked to a 22% increase in heartburn in the Framingham Heart Study update.
- Anticholinergics (for allergies, overactive bladder, motion sickness): Reduce LES pressure by 25% in two-thirds of users.
- Nitrates (for chest pain): Can drop LES pressure by 35-45%.
- Bisphosphonates (for osteoporosis): Can stick to the esophagus and cause chemical burns if not taken with enough water.
Even your heartburn meds can be undermined. Pantoprazole, a proton pump inhibitor (PPI), works best when taken 30-60 minutes before breakfast. But if you eat spicy, fatty, or acidic food within two hours of taking it, your body absorbs up to 23% less of the drug. That means less acid control-and more burning later.
How Antacids Can Backfire
When heartburn hits, most people reach for Tums or Rolaids. They work fast-often in under five minutes. But they’re like putting a bandage on a leaky pipe.
Antacids neutralize acid temporarily, but they don’t fix the leak. And overuse? It can cause problems. Taking them more than 2-3 times a week can throw off your electrolytes. Aluminum-based antacids can block absorption of antibiotics like tetracycline by half. Fluoroquinolones? Up to 90% less effective.
Timing matters. If you take an antacid and then a pill for high blood pressure or thyroid issues, you risk making the drug useless. The Cleveland Clinic recommends taking antacids either one hour before or four hours after other meds. Most people don’t know this. That’s why so many end up thinking their meds “aren’t working.”
What Actually Works: A Realistic Plan
Forget extreme diets. You don’t have to quit spicy food forever. Here’s what works based on clinical data and patient outcomes:
- Track your triggers for 14 days. Write down everything you eat, every pill you take, and when you get heartburn. Look for patterns. Maybe it’s not the salsa-it’s the salsa with your evening aspirin.
- Test one food at a time. Eliminate spicy food for 3-7 days. If symptoms improve, reintroduce it slowly. Start with mild peppers. See if your body reacts. Repeat with other suspects: coffee, chocolate, citrus.
- Time your meds right. Take PPIs like pantoprazole before breakfast. Wait at least two hours before eating anything fatty, spicy, or acidic. Take antacids only after meals or at bedtime-not as a daily crutch.
- Don’t lie down after eating. Gravity helps. Stay upright for at least three hours after meals. This cuts nighttime reflux by 60%.
- Elevate your head. Put 6-8 inches of blocks under the head of your bed. Not just pillows-those slide. This reduces reflux by 45%.
Patients who follow this kind of personalized plan see a 78% success rate in controlling symptoms, according to the American Gastroenterological Association. Those who rely only on pills? Only 42% get lasting relief.
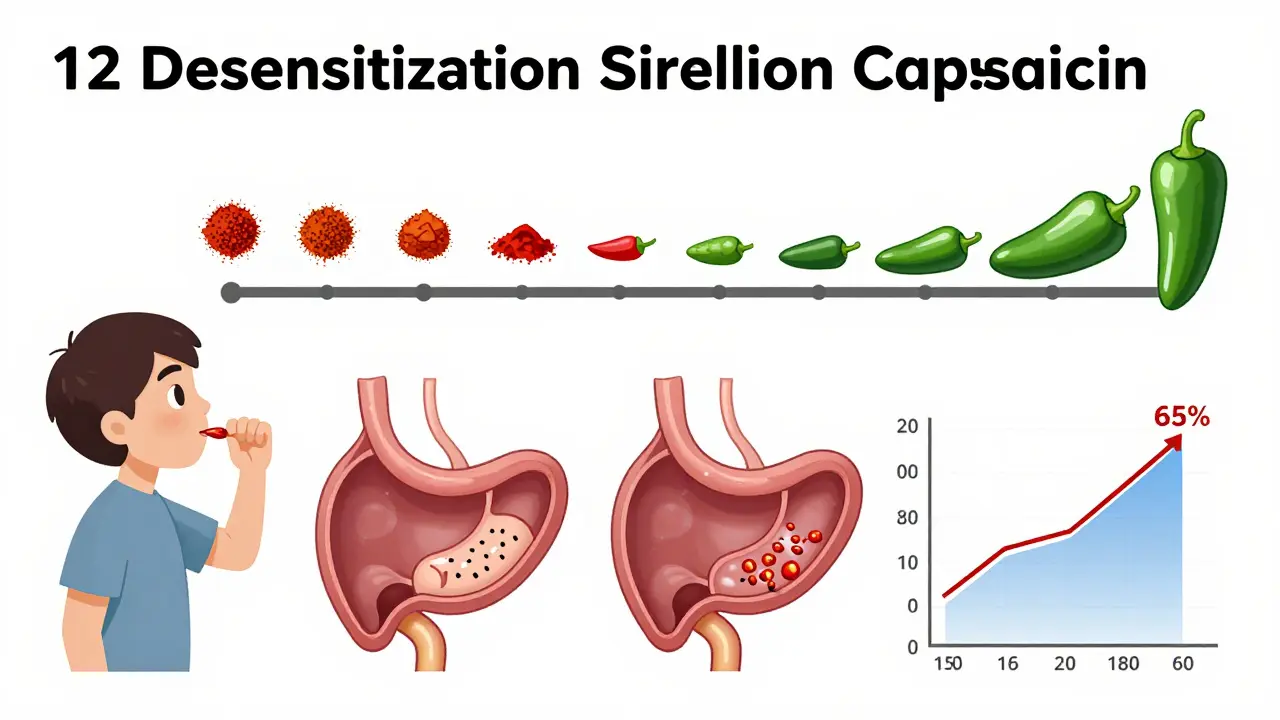
The New Science: Tolerance and Desensitization
There’s good news if you love spicy food: your body can adapt. A 2023 Johns Hopkins trial showed that 65% of participants who slowly increased their capsaicin intake over 12 weeks ended up tolerating spicy meals without symptoms. The trick? Start small. Add a pinch of chili powder to eggs or soup. Increase the amount every few days. Your nerves get used to it.
This isn’t about toughness. It’s about nerve sensitivity. Some people’s nerves overreact to capsaicin. Repeated, gentle exposure can calm that response. It’s like building a tolerance to caffeine-but for your gut.
What’s Changing in GERD Treatment
The medical world is shifting. The old rule-“avoid all spicy food”-is fading. New guidelines from the American Gastroenterological Association (June 2023) now support “precision nutrition.” That means tailoring advice to your body, not your recipe book.
Also, new drugs are coming. Vonoprazan (Voquezna), approved by the FDA in August 2023, blocks acid more reliably than traditional PPIs. It works even in people whose bodies break down older drugs too quickly. And it’s not affected by what you eat.
Meanwhile, the market is changing. Sales of prescription PPIs are slowing as doctors push lifestyle changes. Meanwhile, dietitian-led programs in hospitals are cutting medication costs by 27% and improving outcomes by 33%. That’s not magic-it’s science.
When to Worry
Heartburn that comes and goes? Probably manageable. But if you notice:
- Difficulty swallowing
- Unexplained weight loss
- Vomiting blood or black stools
- Heartburn that wakes you up at night
-it’s time to see a doctor. Antacids can mask serious conditions like Barrett’s esophagus or a hiatal hernia. These don’t cause pain until they’re advanced. Don’t let temporary relief delay a real diagnosis.
Final Takeaway
You don’t have to give up flavor to protect your gut. You just need to understand how your body responds. Spicy food isn’t the enemy. Medications aren’t the enemy. The enemy is ignoring the signals your body sends.
Start with a food and symptom diary. Time your meds. Test one trigger at a time. And if you’re still struggling after 4 weeks, talk to a dietitian or gastroenterologist. The goal isn’t to live without spice-it’s to enjoy it without the burn.





15 Comments
Mussin Machhour
Man, I used to eat ghost pepper wings every Friday and wonder why my chest felt like a campfire. Then I started timing my ibuprofen and realized I was taking it right after the spicy stuff. Now I wait 3 hours. Game changer. No more midnight panic.
Michael Dillon
So you’re telling me my daily Tums habit is making my blood pressure med useless? That’s wild. I’ve been popping them like candy since college. Guess I’m due for a reality check.
Bailey Adkison
Stop blaming the food. The real problem is the pharmaceutical industry pushing PPIs like they’re vitamins. You don’t need to avoid spice you need to stop trusting corporations that profit from your suffering
Justin James
Did you know the FDA approved vonoprazan without a single long-term study on esophageal cancer risk? The same people who told us PPIs were safe for 10 years are now selling this new drug like it’s magic. Wake up. They’re just replacing one profit machine with another. Your gut isn’t broken-it’s being exploited.
Zabihullah Saleh
I grew up in Afghanistan where every meal had chili. No one talked about heartburn. Then I moved here and started taking blood pressure meds. Suddenly, my favorite curry felt like acid rain. It’s not the spice-it’s the combo. We used to eat spicy food with plain yogurt and water. Maybe the answer isn’t avoidance. Maybe it’s balance.
Our ancestors didn’t have PPIs. They had culture. They had rituals. Maybe we’ve lost that. Not every problem needs a pill. Sometimes it needs a meal shared slowly.
I’ve started adding a spoon of plain yogurt after spicy food. It doesn’t cure anything. But it calms the fire. And I feel less alone in it.
Sophie Stallkind
Thank you for this comprehensive and evidence-based overview. The emphasis on personalized nutrition aligns with current clinical guidelines and reflects a commendable shift away from one-size-fits-all dietary dogma. I particularly appreciate the clarification regarding antacid timing and its interaction with pharmacokinetics. This is precisely the kind of patient-centered information that should be disseminated more widely.
Lindsay Hensel
I cried reading this. Not because it was sad-but because I finally feel seen. For years I thought I was just ‘too sensitive.’ I avoided parties, skipped family dinners, hid my spice rack. But it wasn’t me. It was the timing. The meds. The lying down too soon. I started tracking. I waited two hours. I elevated my bed. I’m not cured-but I’m living again. Thank you.
Terry Free
Wow. So we’re supposed to believe that capsaicin is the villain now? Funny how the same people who told us fat was evil now say spice is evil. Next they’ll say gravity causes reflux. Just take your PPI and chill. Your body’s not a chemistry set. It’s a miracle. Stop overthinking it.
Harbans Singh
I’m from India. We eat chili with every meal. My dad had GERD for 20 years. He stopped taking antacids. Started eating jaggery after meals. No more burning. No pills. Just simple things. Maybe the answer isn’t in labs-it’s in kitchens.
Also-did you know turmeric helps? Not as a cure-but as a gentle healer. Mix a pinch in warm milk. Try it. No side effects. Just calm.
Oluwatosin Ayodele
You missed the real issue. The FDA approved vonoprazan because Big Pharma bribed the reviewers. The NIH study on capsaicin was funded by a company that sells PPIs. And why do you think antacids are so cheap? Because they’re designed to fail so you keep buying more drugs. Wake up. This isn’t medicine. It’s a scam.
Rick Kimberly
Interesting point about desensitization. Has there been any research on whether this works for people with autoimmune conditions? I have Hashimoto’s and wonder if nerve adaptation could interfere with immune signaling. Would love to see a follow-up study.
Jason Jasper
I tried the 14-day log. Turned out my heartburn only happened on days I ate pizza with aspirin. I stopped doing that. Done. No meds needed. Sometimes the answer’s just… not mixing two things you thought were fine.
Ben Harris
Wait wait wait-so you’re saying I can’t have my spicy ramen after my beta blocker? That’s like asking me to stop breathing. I’ve been doing this for 15 years. You’re telling me my whole life is wrong? I’m not changing. I’ll just take more Tums. And maybe a nap after dinner. And a second pillow. And a humidifier. And a new bed. And a therapist. And-
Carlos Narvaez
Desensitization? Please. Capsaicin doesn’t ‘calm nerves.’ It destroys them. You’re just numbing the signal. That’s not adaptation. That’s damage. And you call that progress?
Zabihullah Saleh
It’s not destruction. It’s recalibration. Like learning to tolerate loud music. You don’t stop listening-you just adjust your ears. Same with your gut. Start small. One grain of cayenne. Wait. Observe. Your body isn’t your enemy. It’s trying to tell you something. Listen.