How to Tell Influenza and COVID-19 Apart in 2026
It’s January 2026, and the coughing, fever, and fatigue you’re feeling could be the flu-or it could be COVID-19. For years, we treated them like the same illness with different names. But the 2024-2025 season changed everything. For the first time since the pandemic began, influenza caused more hospitalizations and deaths than COVID-19 in the U.S. That doesn’t mean COVID-19 is gone. It means we can’t treat them the same way anymore.
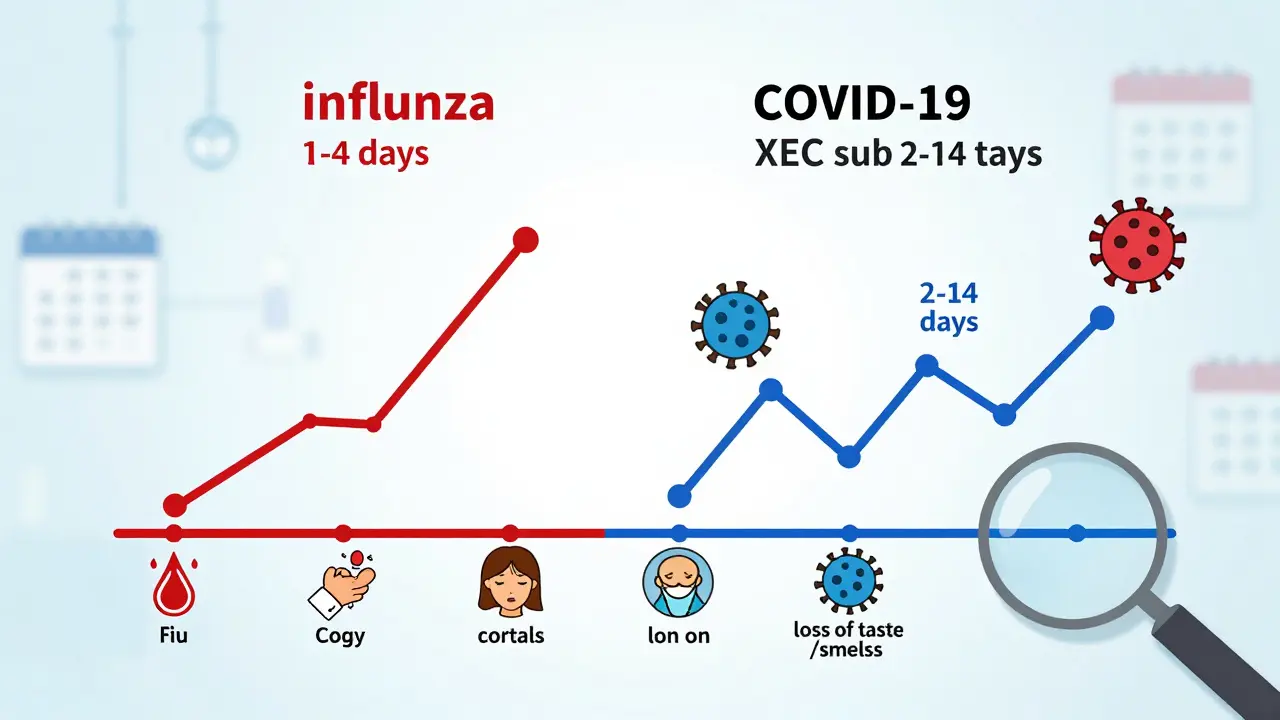
Both viruses attack your lungs and spread through the air. But they behave differently. Influenza hits fast. Symptoms show up in 1 to 4 days after exposure. COVID-19, especially the XEC subvariant, creeps in slower-2 to 14 days. You might feel fine one day, then wake up with a sore throat and body aches the next. The timing matters because it tells you when to test.
Testing: What Works, When, and Why
Most people still rely on rapid antigen tests bought at the pharmacy. They’re fast, cheap, and easy. But they’re not perfect. For influenza, these tests catch about 75% to 85% of cases. For COVID-19, they’re a bit better-80% to 90% accurate. That means a negative result doesn’t always mean you’re clean.
During the 2024-2025 surge, hospitals switched to multiplex PCR panels that test for flu, COVID-19, and RSV all at once. These tests are more sensitive and can detect low levels of virus. If you’re in a hospital or have a high-risk condition, ask for one. At-home combo tests like BinaxNOW now exist, with 89% accuracy for both viruses. But they still miss early infections.
Here’s the key: if your rapid test is negative but symptoms stick around, get a PCR test. Especially if you’re over 65, pregnant, or have heart or lung disease. A 2025 study from Massachusetts General Hospital found that 30% of patients with flu-like symptoms had COVID-19-even after a negative rapid test.
Treatment: Antivirals Are Your Best Bet
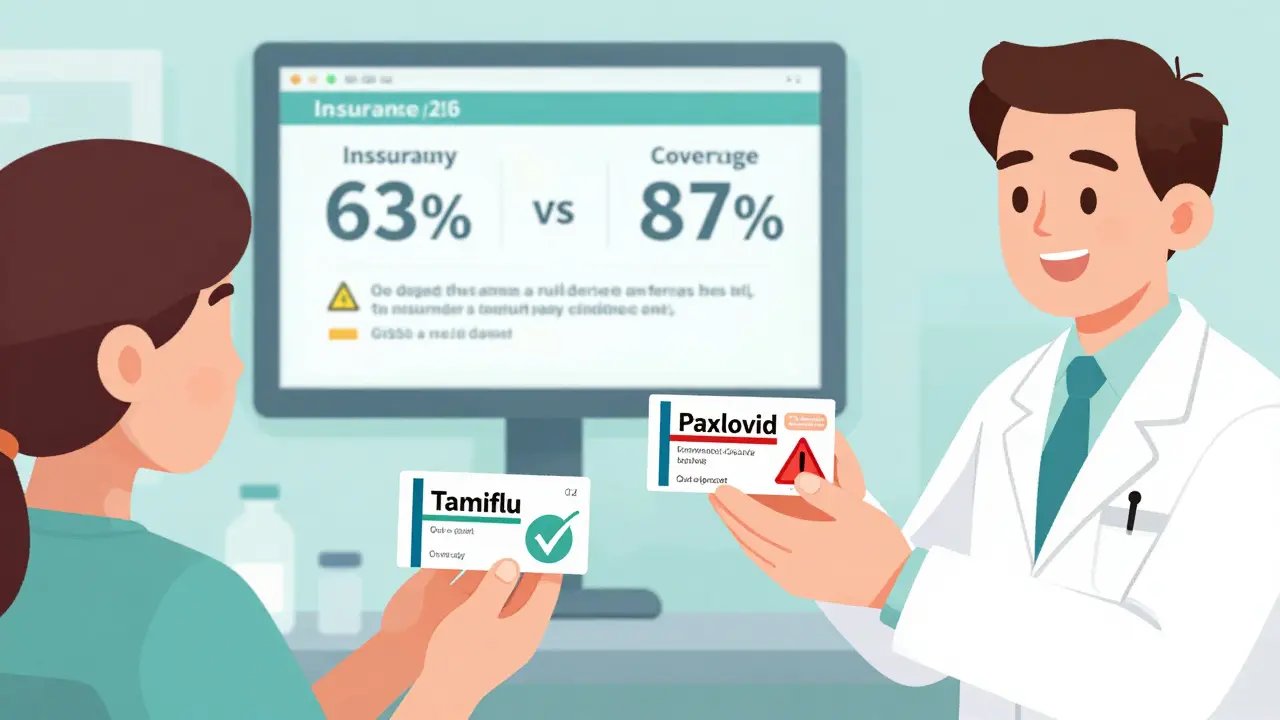
Antivirals work best when taken early. For flu, oseltamivir (Tamiflu) is still the go-to. If you take it within 48 hours of symptoms, it cuts your risk of hospitalization by 70%. For COVID-19, Paxlovid (nirmatrelvir/ritonavir) is the standard. It reduces hospitalization by 89% if taken within 5 days.
But here’s the problem: doctors don’t always prescribe them. In 2025, only 41% of hospitalized COVID-19 patients got antivirals on time. For flu, it was 63%. Why? Some providers still think COVID-19 is “just a bad cold.” It’s not. And insurance doesn’t always cover Paxlovid. KFF found that 63% of patients with commercial insurance paid out of pocket for it, compared to 87% who got full coverage for Tamiflu.
New options are coming. In January 2025, the FDA approved a new flu antiviral-a prodrug of zanamivir-with 92% effectiveness against the H1N1 strain dominating this season. It’s already in some pharmacies. Ask your doctor if it’s right for you.
Antibiotics won’t help. Both are viral. But bacterial pneumonia often follows flu. About 38% of flu patients in hospitals got antibiotics. Only 22% of COVID-19 patients did. That’s because flu more often leads to secondary bacterial infections. If your fever comes back after improving, or your cough turns thick and green, tell your doctor. You might need antibiotics.
Isolation: The Rules Are Different Now
The CDC says isolate for 5 days for both illnesses. Sounds simple. But the details matter.
For flu: You can stop isolating after 24 hours without fever-no fever-reducing meds needed. You’re still contagious, but the risk drops sharply after day 5. Kids might shed the virus for up to 14 days, so keep them home from school if they’re still coughing or tired.
For COVID-19: You need a negative rapid test on day 5 to end isolation. Why? The virus sticks around longer. Even if you feel fine, you could still spread it. That’s why healthcare workers still wear N95 masks around COVID-19 patients-92% of hospitals require it. For flu, only 68% do.
And here’s something most people don’t realize: you can be contagious before you feel sick. With flu, you’re most infectious the day before symptoms start. With COVID-19, it’s 2 to 3 days before. That’s why masking in crowded places during peak season still makes sense-even if you feel fine.
Who’s at Highest Risk?
Not everyone gets equally sick. In 2025, hospitalized COVID-19 patients were more likely to have chronic conditions: kidney disease, cancer, autoimmune disorders, or were on immunosuppressants. Flu patients? More often, they were otherwise healthy. About 42% of flu hospitalizations were in people with no underlying illness. Only 28% of COVID-19 hospitalizations were.
That doesn’t mean healthy people are safe. But it does mean if you have a chronic condition, you need to be extra careful. Vaccines help. In 2025, 52.6% of Americans got the flu shot. Only 48.3% got the updated COVID-19 vaccine. That gap helped flu spread faster.
Loss of taste or smell? That’s still a strong clue for COVID-19. It happens in 40% to 80% of cases. In flu? Only 5% to 10%. If you lose your sense of taste and your throat hurts, assume it’s COVID until proven otherwise.

What You Can Do Right Now
- Get tested if you have symptoms. Don’t wait. Use a combo test if you can.
- Call your doctor within 24 hours of symptoms. Ask about antivirals. Don’t wait for a prescription-ask for it.
- Stay home for at least 5 days. Wear a mask around others, even after isolation ends.
- Check your insurance. If Paxlovid isn’t covered, ask for a generic or patient assistance program. Some pharmacies offer it for under $30.
- Get vaccinated. Flu and COVID vaccines are still the best defense. They don’t prevent all infections, but they cut hospitalization risk by 60-70%.
What’s Changing in 2026?
The CDC’s 2025-2026 guidelines now use a single clinical framework for both viruses. That means one set of rules for when to test, when to treat, and who to prioritize. But isolation rules stay separate. Why? Because the viruses behave differently.
Hospitals are using AI tools to predict outbreaks based on ER visits, test results, and weather patterns. One system in Texas reduced unnecessary antiviral prescriptions by 35% by flagging low-risk cases. It’s not magic-it’s data.
At-home testing is getting smarter. New kits can tell you which virus you have and whether it’s likely to be severe based on your age and health history. They’re not perfect, but they’re getting closer.
The big takeaway? We’re moving away from treating flu and COVID-19 as separate problems. They’re part of the same respiratory threat. But you still need to know the differences to protect yourself and others.
Can I have both flu and COVID-19 at the same time?
Yes. Co-infections happen, especially during peak season. A 2025 study in the Journal of Infectious Diseases found that 3% to 5% of people with respiratory symptoms tested positive for both viruses. Symptoms are worse when both are present-higher fever, longer recovery, greater risk of pneumonia. If you’re hospitalized and your condition doesn’t improve after starting antivirals, ask for a multiplex PCR test to check for both.
Do I need to isolate if I’m vaccinated?
Yes. Vaccines reduce severity but don’t stop transmission. You can still catch and spread either virus-even if you’re fully vaccinated. Isolation rules apply to everyone, regardless of vaccination status. The goal is to protect others, especially those at high risk.
Why is Paxlovid harder to get than Tamiflu?
Paxlovid has stricter eligibility rules. It’s approved for people with risk factors-like age, diabetes, heart disease, or obesity. Tamiflu is approved for anyone over 2 weeks old. Insurance coverage is also uneven. Many plans cover Tamiflu automatically. For Paxlovid, you often need prior authorization. Ask your pharmacist or doctor to help you navigate this.
Can I use the same mask for flu and COVID-19?
Yes. N95, KN95, or surgical masks work for both. The virus spreads the same way-through respiratory droplets. The CDC doesn’t differentiate mask types based on the virus. What matters is fit and filtration. A well-fitted N95 reduces transmission risk by over 80% for both flu and COVID-19.
When should I go to the ER?
Go to the ER if you have trouble breathing, chest pain, confusion, bluish lips or face, or severe dehydration (no urine for 12+ hours). These signs can happen with either virus. Don’t wait. Early treatment saves lives. Also, if you’re immunocompromised and have any symptoms, seek care immediately. You’re at higher risk for complications.
Are at-home tests reliable enough?
They’re good for screening, not diagnosis. If you feel fine but test positive, you’re likely contagious. If you feel sick but test negative, test again in 24-48 hours. Viral load rises over time. A single negative test doesn’t rule out infection, especially in the first 2 days of symptoms. Use them as a tool, not a final answer.
Final Advice: Don’t Guess-Test and Act
Flu and COVID-19 are no longer interchangeable. They’re two different viruses with different rules. The best way to protect yourself is to know which one you have-and act fast. Test early. Take antivirals when prescribed. Isolate properly. And don’t wait for symptoms to get worse before doing something.
This isn’t about fear. It’s about being smart. The tools are here. The data is clear. The next time you feel sick, don’t just wait it out. Test. Talk to your doctor. And take the right steps for the virus you’re facing-not the one you assume you have.






15 Comments
Selina Warren
This is exactly why we need to stop treating flu and COVID like the same monster. One hits like a freight train, the other creeps up like a ghost. I got tested twice last month because I felt fine but knew I’d been exposed. First test negative, second one positive for COVID. No fever, just a weird fatigue. Don’t wait until you’re coughing up a lung. Test early, act faster.
And yes, Paxlovid is a nightmare to get. My doctor had to call three pharmacies before one had it in stock. Insurance acted like it was a luxury drug. Tamiflu? Easy. Just say the word. Why is that still a thing?
Robert Davis
The CDC’s new guidelines are just bureaucratic noise. They say 'one framework' but still keep isolation rules separate? That’s not logic, that’s confusion dressed up as policy. And don’t get me started on AI predicting outbreaks. Sounds like a tech bro fantasy. Real doctors still have to make calls with half the info. We’re automating guesswork.
Eric Gebeke
Let’s be real. The reason Paxlovid is hard to get is because Big Pharma doesn’t want you taking it unless you’re rich or desperate. Tamiflu’s been around since the 90s. Cheap. Generic. Easy. Paxlovid? Patent protected. Price gouging. And now they’re pushing combo tests like they’re miracle wands. They’re not. They’re just more expensive. You’re being sold a solution that benefits them, not you.
Chuck Dickson
Hey everyone - I’m not a doctor, but I’ve been helping my 78-year-old mom navigate this mess since last fall. She’s got COPD. Got the flu shot. Got the updated COVID shot. Still caught both in December. Here’s what saved her: calling her doctor the *second* she felt off. Got Tamiflu within 12 hours. Got Paxlovid after a second test confirmed COVID. No hospital. No oxygen. Just rest, fluids, and meds.
Don’t wait for symptoms to get ‘bad enough.’ If you’re over 60 or have any chronic condition, treat every sniffle like a red flag. And if your doctor hesitates? Push. Politely. But firmly. Your life isn’t a waiting game.
rachel bellet
The multiplex PCR panel adoption rate remains suboptimal in community clinics due to cost-benefit asymmetries and reimbursement inertia. While sensitivity metrics are statistically superior (p < 0.01), the marginal utility diminishes in low-risk populations. The 30% false-negative rate for rapid antigen tests in the MGH cohort is confounded by viral load kinetics and timing of sampling. A Bayesian decision-theoretic model would better inform triage protocols than current algorithmic guidelines.
Pat Dean
They’re lying. They say flu is worse now but don’t tell you why. It’s because the CDC stopped tracking the real numbers. The hospitals are pressured to call everything ‘flu’ to make COVID look less scary. I work in a lab. We’ve seen the data. COVID’s still spreading like wildfire. They just don’t want to panic people. You think they care if you die? They care about the stock market.
Joni O
I just want to say thank you to whoever wrote this. I’m a single mom of two kids under 5. Last winter, I waited too long to test. Both kids got sick, I got sick, and we were all in bed for 10 days. This time? Day 1: test. Day 1: called doctor. Got Tamiflu. Kids are back at school. I’m not perfect, but I’m trying. If you’re tired of feeling like a zombie every winter - test. Don’t wait. You’ve got this.
Max Sinclair
I appreciate the clarity here. A lot of people don’t realize that isolation rules aren’t arbitrary - they’re based on how long each virus sheds. Flu clears faster, so 24 hours fever-free makes sense. COVID lingers, so the test requirement isn’t bureaucracy, it’s science. And masks? N95s work because they filter particles, not because they’re labeled for one virus. Fit matters more than the brand.
christian Espinola
AI predicting outbreaks? Yeah right. The same AI that told us the pandemic was over in 2021? The same system that missed the surge in 2023? Don’t trust algorithms built by people who’ve never held a thermometer. This is all just PR. They want you to think they’re in control. They’re not. We’re just lab rats in a giant experiment.
Dayanara Villafuerte
Paxlovid = $$$ 💸 Tamiflu = 💰
Same symptoms. Different price tags. Welcome to American healthcare 🤡
Also, if you lose taste? Assume it’s COVID. No debate. I lost mine last year. Took 3 weeks to come back. Felt like my soul got deleted. Don’t play with this stuff.
kenneth pillet
Used to think flu was just a bad cold. Got sick in 2024. Stayed in bed for a week. Couldn’t breathe climbing stairs. Now I test every time I sneeze. Got the combo test last month. Flu. Took Tamiflu. Back to work in 3 days. Don’t be dumb. Test. Don’t wait.
Kristin Dailey
Stop lying to people. Flu isn’t worse. COVID is still killing more. They just changed how they count. You think the hospitals want to admit more COVID patients? They’re overwhelmed. So they label it flu. It’s a numbers game. Don’t fall for it.
Jay Clarke
We’re not fighting viruses anymore. We’re fighting narratives. One side says ‘flu is back.’ The other says ‘COVID is still the real threat.’ The truth? Both are here. Both are dangerous. But nobody wants to say that because it doesn’t fit their agenda. We’re not patients. We’re content. And the real virus? It’s the lie we keep feeding each other.
Jake Moore
Just got my first combo test at CVS. Paid $15. Worked great. Tested positive for flu, negative for COVID. Took Tamiflu same day. Felt better in 36 hours. My neighbor had the same symptoms, waited 3 days, ended up in the ER with pneumonia. Don’t be her. Test. Talk. Take the meds. It’s not that hard.
Praseetha Pn
You think this is about health? Nah. This is about control. The government, Big Pharma, WHO - they want you dependent on tests and pills. They don’t want you strong. They want you scared. I stopped taking vaccines. I eat turmeric, garlic, ginger. My immune system is a fortress. You think a pill can replace your body’s wisdom? Wake up. The real pandemic is fear. And they sold it to you in a box labeled 'protection'.