Every year, thousands of children end up in emergency rooms because of a simple mistake: the wrong dose of medicine. Not because parents are careless. Not because doctors are negligent. But because the system is built for adults - and kids aren’t just small adults. A child weighing 10 kilograms needs a completely different amount of medicine than a 30-kilogram child. Get it wrong, and you risk overdose, organ damage, or worse. In pediatric emergency departments, medication errors happen in up to 31% of cases - more than double the rate seen in adults. And most of these aren’t caught until it’s too late.
Why Pediatric Medication Errors Are So Common
It starts with weight. Unlike adults, where most pills come in standard doses, children’s medications are almost always calculated by kilograms. A child needs 10 mg per kg of body weight? That sounds simple - until you’re in a rush, the child is crying, and the scale says 22 pounds, not kilograms. Multiply that by 2.2 to convert? That’s a calculation many nurses and even some doctors do on the fly under pressure.
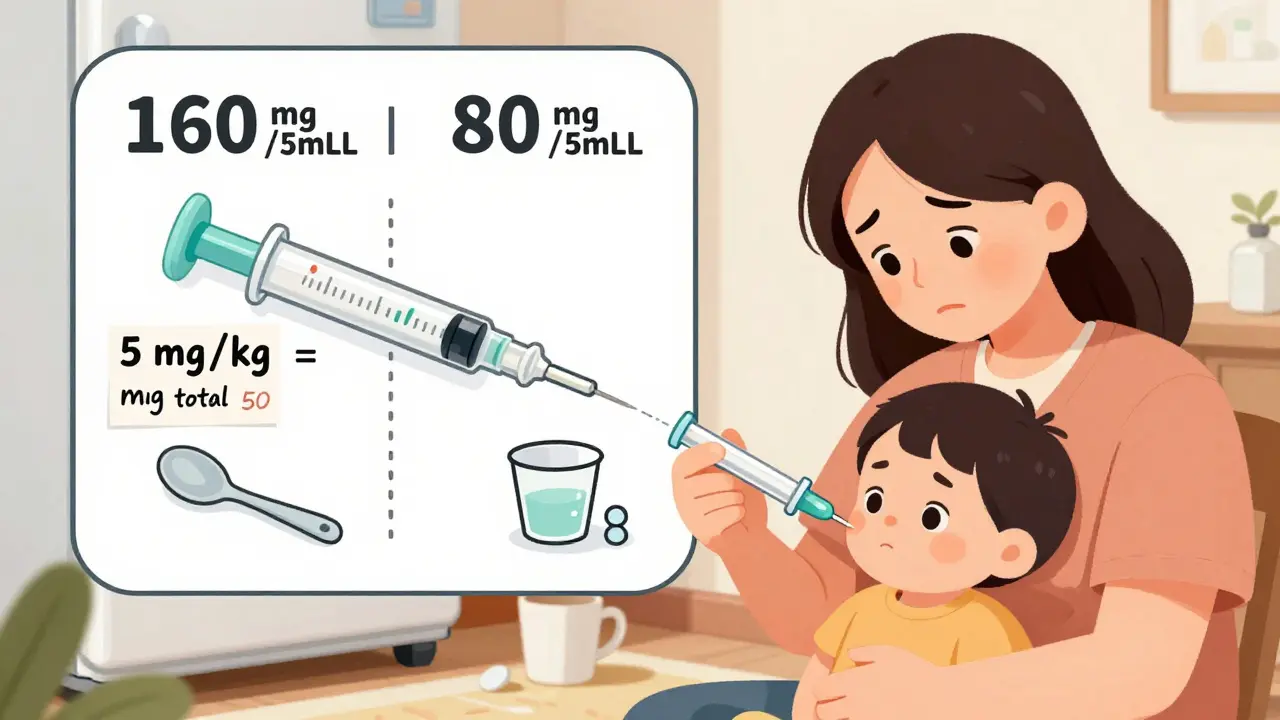
Then there’s the liquid. Over 60% of pediatric dosing errors involve liquid medications. Parents might grab a kitchen spoon because they lost the syringe. Or they confuse milligrams (mg) with milliliters (mL). One parent in a 2019 case report gave 5 mL of acetaminophen to a 10 kg child - thinking that was the dose - when the correct amount was 5 mg per kg, or 50 mg total. That’s a tenfold overdose. The child ended up in liver failure.
Even when the right dose is written down, it’s often misread. Two similar-looking labels - infant Tylenol versus children’s Tylenol - have different concentrations. One is 160 mg per 5 mL. The other is 80 mg per 5 mL. Mix them up, and you’re giving a child twice the intended dose. Reddit threads from parents in 2024 are full of stories like this: “I gave my toddler 5 mL of children’s Tylenol thinking it was the same as infant, didn’t realize the difference until the pediatrician called.”
The Hidden Errors: What Isn’t Reported
Most medication errors never make it into official reports. Studies show that only 10% to 30% of actual errors are documented through incident logs. Why? Because many are caught before they reach the child - a nurse double-checks, a pharmacist spots the mistake, or a parent questions the dose. But those near-misses? They’re invisible to the system.
One 2004 study used syringe analysis to uncover hidden errors. They looked at the actual liquid left in syringes after administration and found dosing mistakes that no one had reported. The system was designed to catch only the obvious ones. The quiet mistakes - the ones that happen because a nurse was tired, or the EMR didn’t auto-calculate weight, or the parent didn’t understand the instructions - slip through.
And the consequences? One in eight medication errors in pediatric ERs causes real harm. Another 47% reach the child but don’t cause injury. The rest are caught in time. But even the “harmless” ones erode trust. Parents start second-guessing every dose. They stop asking questions because they’re afraid they’ll sound stupid.
Who’s Most at Risk?
It’s not just about the hospital. The biggest risk happens after discharge - at home. Parents are given prescriptions, instructions, and sometimes a syringe. But if they don’t speak English well, if they’re low-income, or if they have limited health literacy, the chances of error jump dramatically.
Studies show parents with low health literacy make medication errors 2.3 times more often than those with higher literacy. Spanish-speaking families have a 32% higher error rate than English-speaking ones. Medicaid-enrolled children experience 27% more dosing errors than kids with private insurance. Why? Because they’re more likely to get discharge instructions printed in small font, without pictures, and without follow-up. They’re more likely to use a kitchen teaspoon because they don’t have a dosing syringe. And they’re less likely to call back when confused.
Even parents of children with chronic conditions - like leukemia or epilepsy - make dosing mistakes at home. One study found 1 in 10 parents of kids on oral chemotherapy misread the dose. That’s not negligence. That’s a system failing them.
What’s Working: Real Solutions from the Front Lines
Some hospitals are fixing this. Nationwide Children’s Hospital in Ohio cut harmful medication events by 85% in five years. How? They didn’t just train staff. They changed the whole workflow.
- Every pediatric dose in the ER now goes through a double-check system - two trained staff verify weight, calculation, and medication before it’s given.
- All EMRs now auto-calculate doses based on weight in kilograms, with alerts if the dose exceeds safe limits.
- Pharmacists review every pediatric order before it leaves the pharmacy.
- High-alert medications like morphine or epinephrine are stored separately and labeled in bold red.
At home, simple changes make a huge difference. The MEDS intervention - a 90-second extra step at discharge - reduced dosing errors from 65% to 49%. Here’s what it included:
- Clear pictograms showing how to use the syringe.
- Verbal instructions followed by the parent repeating them back (teach-back method).
- Providing a dosing syringe - not a cup or spoon - and showing exactly how to use it.
- Writing the dose in both mg/kg and total mg, not just “give 5 mL.”
Parents who got this simple intervention were 25% less likely to make a mistake at home. And the best part? The effect lasted. Even after the program ended, error rates stayed lower than before.
The Tools That Should Be Standard - But Aren’t
By 2023, 68% of children’s hospitals had pediatric-specific dosing calculators in their electronic records. But in community ERs - the places most families go - only 32% did. That’s a dangerous gap. A child who has a seizure at a small-town ER might get the same dosing system as an adult. No weight-based alerts. No built-in safety checks. Just a doctor guessing.
And yet, the tools exist. The technology is cheap. The American Academy of Pediatrics has pushed for standardized pediatric dosing protocols since 2015. But adoption is slow. Why? Because changing systems costs money. Because staff are overworked. Because no one’s holding hospitals accountable for pediatric medication safety the way they are for surgical errors or infections.

What Parents Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what works:
- Always ask: “Is this dose based on my child’s weight?” If they say yes, ask them to show you the calculation.
- Get a dosing syringe - not a cup or spoon. Buy one at the pharmacy if they don’t give you one.
- Write down the dose in both mg/kg and total mg. Keep it on your phone.
- Use the teach-back method: “So I give 5 mL of this, twice a day, right?” Then repeat it back to the nurse.
- If the medicine looks different from last time - ask why. Concentrations change.
- Keep a list of all medications your child takes - including over-the-counter ones - and bring it to every visit.
One mother in Perth told me her son had a fever after a vaccination. The nurse gave her a bottle of children’s ibuprofen. She read “5 mL” on the label and gave it. Later, she saw a different bottle at home with “2.5 mL” for the same weight. She called the clinic. Turned out the first bottle was for older kids. She’d almost given a double dose. She said, “I didn’t know there were different strengths. No one told me.”
The Bottom Line
Medication errors in children aren’t accidents. They’re system failures. They happen because we treat kids like mini-adults. Because we assume parents know how to measure milligrams. Because we don’t invest in the tools that make safety easy.
But change is possible. Hospitals that use double-checks, auto-calculators, and teach-back methods see real drops in harm. Parents who ask questions, use syringes, and write things down protect their children better than any policy ever could.
The next time you’re handed a bottle of medicine for your child, don’t just say “thank you.” Ask: “How did you calculate this? Can you show me?” That one question could save a life.
Why are pediatric medication errors more common than adult ones?
Pediatric errors are more common because children’s doses must be calculated by weight (mg/kg), not fixed amounts. Adults usually get standard doses, but kids need precise calculations based on their size - which introduces more room for math mistakes. Liquid medications, which make up most pediatric doses, are harder to measure accurately than pills. Emergency settings add pressure, time limits, and verbal orders - all of which increase the chance of error. Studies show pediatric error rates are 31% compared to 13% in adults.
What’s the most common type of pediatric medication error?
The most common error is wrong dose - accounting for 13% of all reported pediatric medication safety events. This often happens due to incorrect weight conversion (pounds to kilograms), confusion between milligrams and milliliters, or using the wrong concentration of liquid medicine. For example, giving 5 mL of children’s Tylenol instead of infant Tylenol can result in a double dose because the concentrations differ.
How can parents prevent dosing mistakes at home?
Parents can prevent mistakes by always using a dosing syringe (not a spoon or cup), writing down the dose in both mg/kg and total mg, asking staff to explain how the dose was calculated, and using the teach-back method - repeating instructions back to the provider. Keep a list of all medications, including over-the-counter ones, and check labels for concentration differences. If something looks different from last time, ask why.
Do hospitals have systems to catch these errors before they happen?
Some do - especially children’s hospitals. Leading centers use double-check systems for high-risk meds, automated weight-based dosing calculators in electronic records, and pharmacy verification of all pediatric orders. But many community emergency departments still rely on manual calculations and lack these safeguards. Only 68% of children’s hospitals had these tools in 2023; far fewer general ERs did.
Are language barriers a factor in pediatric medication errors?
Yes. Families with limited English proficiency have a 45% dosing error rate compared to 28% for English-speaking families. Language barriers lead to misunderstandings about dosage, timing, and concentration. Hospitals that provide translated pictograms, trained interpreters, and simplified written instructions reduce these errors significantly. The MEDS intervention showed Spanish-speaking families had 32% fewer errors when given visual aids and teach-back.
What should I do if I think I gave my child the wrong dose?
Call your pediatrician or poison control immediately - don’t wait for symptoms. In Australia, call Poison Help at 13 11 26. Have the medicine bottle ready so you can tell them the name, concentration, amount given, and your child’s weight. Even if your child seems fine, some overdoses take hours to show signs. It’s better to be safe. Most poison centers have 24/7 support for medication errors.






13 Comments
Christina Bilotti
Oh wow, a whole article about how doctors can’t do basic math? Groundbreaking. I’m sure the 31% error rate is just because nurses forgot to use their phones’ calculators. Maybe if hospitals stopped hiring people who still think ‘10 kg’ is ‘10 pounds’ we wouldn’t need a 12-page manifesto on this. At this point, I’m just waiting for the study that proves water is wet.
brooke wright
I gave my daughter Tylenol once and she got sick and I didn’t know if it was the medicine or the fever or if I used the wrong syringe and now I cry every time I see a bottle and I just want someone to tell me what to do please I’m so scared I’m going to kill my kid
vivek kumar
The systemic failure here is not merely logistical-it is epistemological. We treat pediatric dosing as a computational problem when it is, in fact, a communication crisis. The math is trivial. The language, the trust, the cultural context-those are the real variables. No algorithm fixes a parent who doesn’t understand ‘mg’ versus ‘mL’ because their primary language lacks precise medical lexicon. The solution isn’t better calculators. It’s better translators. Not just of words, but of intent.
Nick Cole
This is the most important thing I’ve read all year. I work in a community ER and we don’t have auto-calcs. We use paper forms. Last week, a mom brought her 8-month-old in with a fever. She had given 7 mL of children’s Tylenol because the bottle said ‘for babies 6-12 months’ and she thought that meant ‘one dose fits all.’ We caught it before it went in, but I still think about it. We need to stop assuming parents know this stuff. We need to show them. Not tell. Show.
Isabella Reid
My cousin’s kid had a seizure last year because the nurse mixed up the concentrations. She’s fine now, but the trauma? Unspoken. The real tragedy isn’t the math-it’s that we’ve normalized this. We’ve turned pediatric safety into a checklist instead of a culture. And then we blame parents when things go wrong. We need to stop treating families like liabilities and start treating them like partners. Simple. But hard. Because it costs money. And humility.
Rob Deneke
Use a syringe not a spoon dont guess the dose write it down ask them to show you how they calculated it if it looks different ask why keep a list of meds and if you think you gave too much call poison control dont wait
evelyn wellding
YESSSS this!! 💪 I used to be terrified of giving meds to my twins 😭 But once I got the syringe and wrote the dose on my hand with a marker? Game changer. Now I even remind other parents at the park. You got this! 🙌❤️
Chelsea Harton
we dont need more tech we need more care
Corey Chrisinger
It’s funny how we build skyscrapers with precision but still let kids get dosed with kitchen spoons. We’ve mastered quantum computing but can’t standardize a liquid medicine label. Is it because children don’t vote? Or because their suffering doesn’t make headlines? We optimize for profit, not for the smallest among us. And that’s not a system failure-it’s a moral one.
Bianca Leonhardt
Of course it’s 31%. Anyone who lets a non-pediatric-trained nurse handle a child’s meds deserves what they get. And parents? If you can’t read a label or use a syringe, maybe you shouldn’t be in charge of a human being’s life. This isn’t rocket science. It’s basic. And yet here we are.
Travis Craw
im just glad i found this before i had to give my niece meds last night. i was gonna use the cup but now im gonna get a syringe. thanks for the reminder
Corey Sawchuk
Canada’s doing better with standardized labels but we still have gaps in rural clinics. Same story. Same mistakes. Same scared parents. We need a national pediatric dosing protocol. Not just recommendations. Mandates. And funding. It’s not a luxury. It’s a right
Riya Katyal
Wow. So the solution to systemic failure is... asking nicely? That’s it? You really think a mom who works two jobs and doesn’t speak English is gonna stop and say ‘can you show me the math’ while her kid’s screaming and the nurse’s on the phone with another patient? Wake up. This isn’t a parenting blog. It’s a crime scene.