Getting the medicine you need shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only thing standing between them and going without life-saving drugs. But getting into these programs isn’t simple. The rules change depending on who you are, how much you earn, what insurance you have-or don’t have-and even which drug you’re taking.
Who Qualifies for Patient Assistance Programs?
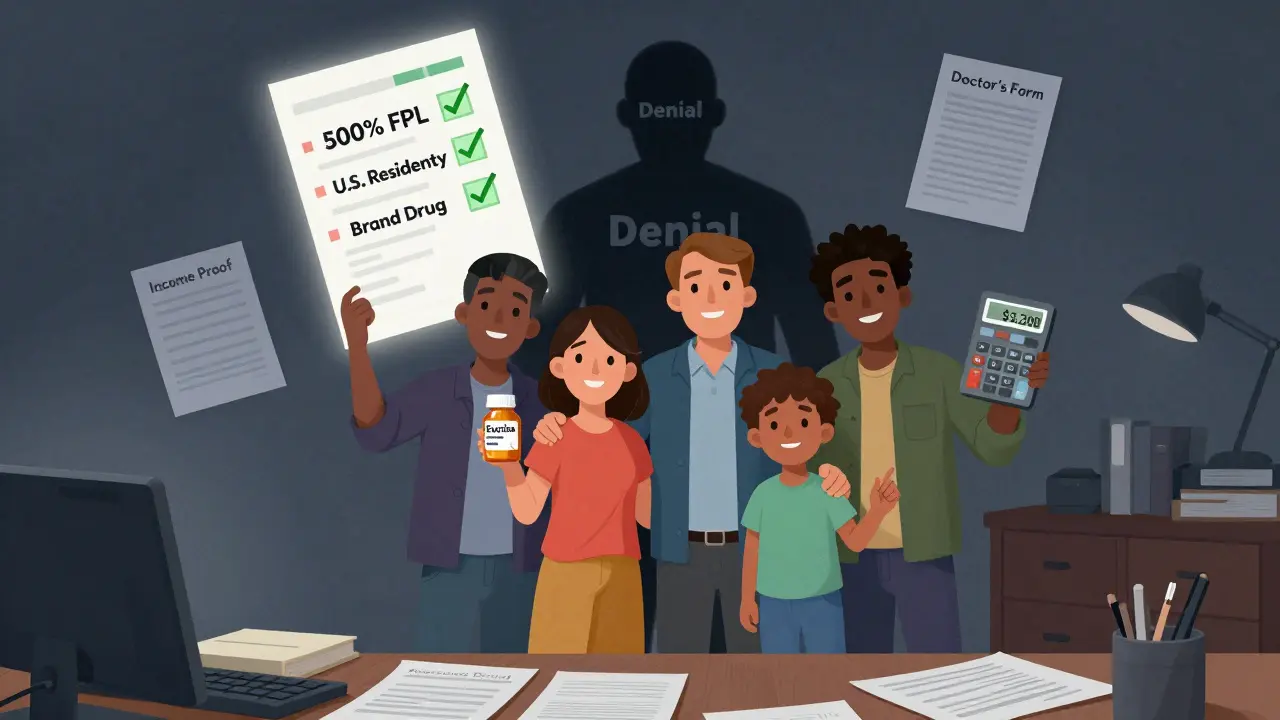
The most common requirement across all major programs is income. Nearly every drug company uses the Federal Poverty Level (FPL) as their baseline. For 2023, 500% of FPL means $75,000 a year for a single person and $153,000 for a family of four. That sounds high, but many people still fall through the cracks. Pfizer’s RxPathways program, for example, sets different income limits based on the drug. For a skin cream like Eucrisa, you must earn less than 300% FPL ($43,200 for one person). But for an expensive cancer drug, the limit jumps to 500-600% FPL ($64,800-$77,760). GSK’s program caps income at $58,650 for one person and $120,570 for a family of four. These aren’t just suggestions-they’re strict cutoffs. Miss the number by $500, and your application gets denied.Insurance Status: The Biggest Hurdle
Here’s where things get confusing: having insurance doesn’t always help. In fact, it can hurt your chances. Most manufacturer PAPs only help people who are uninsured or underinsured. That means if you have commercial insurance-like through your job-you’re often automatically disqualified. Pfizer’s program, for instance, explicitly says: “We do not assist patients with private insurance.” But there’s a twist. Some programs, like Merck’s, allow insured patients to apply if they’re facing “special financial hardship.” That sounds vague, and it is. You’ll need to prove your out-of-pocket costs are crushing you, even with insurance. Medicare beneficiaries face an even tougher maze. If you’re on Medicare Part D and your income is below 150% FPL ($20,385 for one person), you’re supposed to qualify for “Extra Help,” a government program that lowers your drug costs. But here’s the catch: most drug company PAPs won’t help you unless you’ve already been denied Extra Help. Takeda’s program requires you to submit official denial letters before they’ll even look at your application. And if you’re caught between 135% and 150% FPL? You’re in the gap. You earn too much for Extra Help but too little to afford your co-pays. That’s when you’re most likely to be turned down by both government and manufacturer programs.Residency and Treatment Location Matter
You don’t have to be a U.S. citizen, but you do have to live here. All major PAPs require proof of U.S. residency. That means a valid U.S. address, a utility bill, or a lease agreement. If you’re living abroad-even temporarily-you’re out of luck. You also need to be treated by a U.S.-licensed doctor. That’s non-negotiable. Even if you’re a U.S. citizen living overseas, if your prescriptions are written by a doctor in Canada or Mexico, you won’t qualify.Not All Drugs Are Created Equal
PAPs don’t cover every medication. They focus on expensive, brand-name drugs-especially in oncology, autoimmune diseases, and rare conditions. A 2023 IQVIA report found that 98% of branded cancer drugs are covered by manufacturer PAPs, compared to just 76% of heart medications. AbbVie’s program doesn’t even let you apply until you’ve picked a specific drug through their online portal. The system checks eligibility based on that drug’s criteria. So if your doctor prescribes Humira, you apply under Humira’s rules. If they switch you to Skyrizi, you start over. Generic drugs? Almost never covered. PAPs are designed to help with high-cost branded drugs. That’s why so many patients end up waiting months for a brand-name prescription to be approved, even when a cheaper generic exists.
What Documents Do You Need?
The paperwork is overwhelming. Most programs require:- Completed application form signed by you and your doctor
- Proof of income: W-2s, pay stubs, tax returns, or Social Security statements
- Proof of residency: utility bill, lease, or government ID with address
- Proof of insurance status: denial letters, insurance cards, or Medicare paperwork
- Physician verification form: This is separate from the prescription and often takes weeks to get back
How Long Does It Take?
The average application takes about 27 minutes to fill out. But approval? That’s a different story. Once submitted, most programs take 10-14 days to process. Pfizer’s system, which now pulls income data directly from TurboTax, cuts that time in half. But if your doctor hasn’t returned the verification form? You’re stuck. Merck reports it takes an average of 28 days to get that form back. If you’re denied, don’t give up. A 2022 survey by the Medicare Rights Center found 42% of applicants needed three or more tries to get approved. Most denials happen because of missing documents-not because you didn’t qualify.What Happens After You’re Approved?
Getting approved is just the start. You’ll need to reapply every 6 to 12 months. GSK requires annual re-enrollment. For specialty drugs, some programs ask for income verification every quarter. Your medication will usually arrive within 72 hours of approval. That’s one of the fastest parts of the process. But if your doctor changes your prescription-even slightly-you might lose coverage. PAPs are tied to specific drugs, not conditions. Switch from one biologic to another? You start over.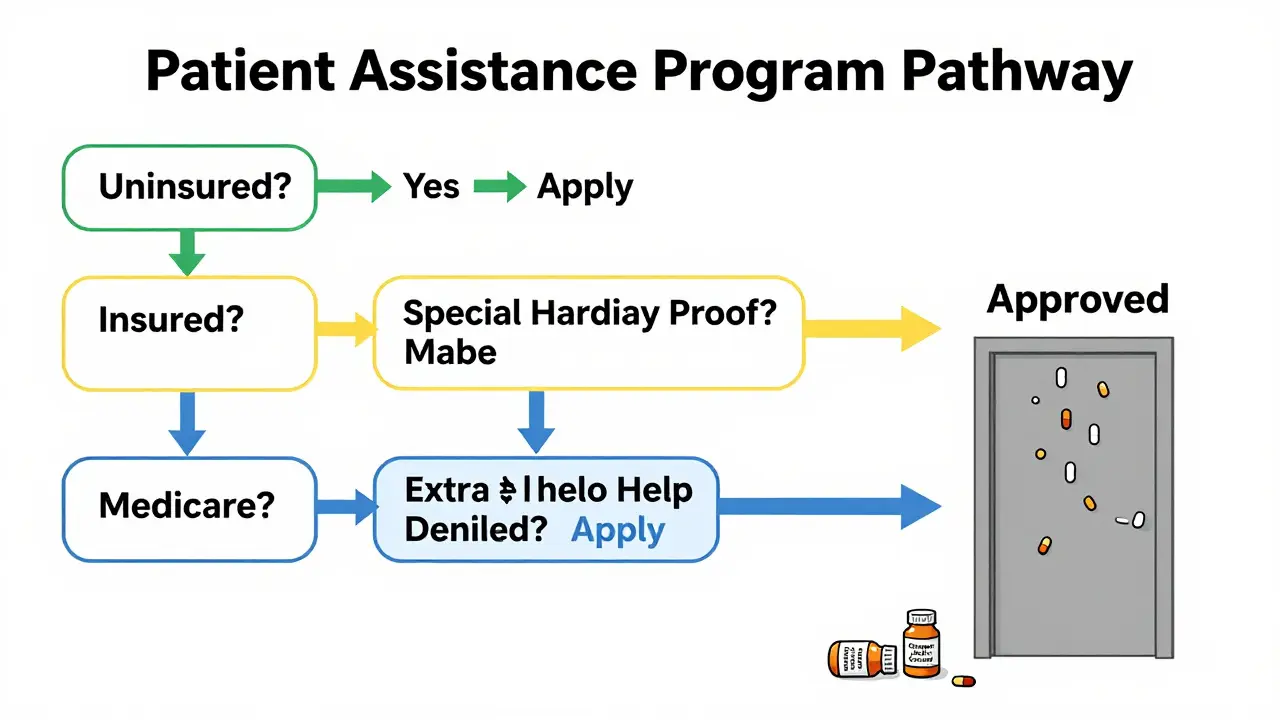
What About Independent Charity PAPs?
If you’re turned down by a drug company, don’t stop there. Independent charities like the PAN Foundation and HealthWell Foundation offer help too. They’re not run by pharmaceutical companies, so their rules are different. These charities often have lower income limits-usually 400-500% FPL-and they sometimes help people with insurance. But they cover fewer drugs and have smaller funding pools. You can only apply for one drug at a time, and waitlists are common. The good news? They’re more flexible with documentation. If you’re homeless, undocumented, or can’t get a tax return, they might still help you.Why Do These Programs Exist?
Critics say PAPs let drug companies avoid lowering prices. Harvard’s Dr. Aaron Kesselheim argues they’re a PR tool: “They make patients feel supported while letting companies keep prices high.” There’s truth to that. In 2021, drug companies gave away over $20 billion in free medications. But they also spent $32.7 billion on marketing the same drugs. And prices keep rising. Still, for many people, these programs are the only way to survive. Without them, 1 in 5 Americans would skip doses or stop taking their meds entirely.What’s Changing in 2025 and Beyond?
New laws are reshaping the landscape. The Inflation Reduction Act caps Medicare Part D out-of-pocket costs at $2,000 a year starting in 2025. That will cut PAP use among seniors by 35-40%, according to Avalere Health. Drug price negotiation is coming too. Starting in 2026, Medicare will negotiate prices for 10 high-cost drugs. That could reduce the need for PAPs by 15-20%. But here’s the catch: even with price caps, many people will still be underinsured. Over 27 million Americans have insurance but pay so much in co-pays and deductibles that they can’t afford their meds. That’s where PAPs will still matter.What Should You Do Next?
If you’re struggling to pay for medication:- Find your drug’s manufacturer website. Search “[Drug Name] patient assistance program.”
- Check your income against 500% FPL. Use the HHS calculator to confirm.
- Confirm your insurance status. Are you uninsured? On Medicare? Private insurance?
- Gather your documents: ID, income proof, doctor’s contact info.
- Call the program’s help line. Most have patient navigators.
- If denied, ask why. Fix the error. Reapply.
- Check independent charities like PAN Foundation or HealthWell Foundation.
Can I get free medicine if I have Medicare?
Yes, but only under specific conditions. Most drug company PAPs won’t help if you’re on Medicare Part D unless you’ve been denied Extra Help first. You must prove your income is below 150% FPL and submit official denial letters. Some programs, like Takeda’s, require this step before even reviewing your application. Medicare Part D itself has a cap on out-of-pocket costs starting in 2025, which may reduce the need for PAPs, but gaps still exist for those with higher incomes.
Do I need to be a U.S. citizen to qualify?
No, citizenship isn’t required. But you must live in the United States and be treated by a U.S.-licensed doctor. Proof of U.S. residency-like a lease, utility bill, or state ID-is mandatory. If you’re a legal resident, refugee, or asylum seeker with a valid U.S. address, you can apply. The programs don’t ask for Social Security numbers, only your income and treatment details.
Why was my application denied even though my income is low?
The most common reason is incomplete or incorrect documentation. Over 68% of denials happen because of missing forms, unsigned doctor letters, or mismatched income proof. Another 22% are due to errors in calculating household size or income type. Many applicants use gross income instead of Modified Adjusted Gross Income (MAGI), which can disqualify them. Double-check your math, make sure your doctor signed everything, and confirm your address matches your ID.
Can I use a patient assistance program if I have private insurance?
Usually not. Most manufacturer PAPs exclude people with private insurance. But exceptions exist. Merck allows applications from insured patients who can prove “special financial hardship”-like high co-pays that exceed 10% of their income. Some newer programs, launched in 2022-2023, are designed specifically for insured patients with high out-of-pocket costs. These are called “commercial PAPs.” Check your drug’s manufacturer website for details.
How often do I have to reapply?
It depends on the drug and the program. For primary care medications like blood pressure pills, you’ll typically reapply once a year. For specialty drugs like cancer treatments or biologics, you may need to re-verify every 3 to 6 months. GSK requires annual re-enrollment for all drugs. Always ask your program’s representative when your next deadline is. Missing a re-application can mean losing your medication.
Is there help filling out the forms?
Yes. Most major PAPs have patient navigators-trained staff who help you complete applications, understand income rules, and contact your doctor’s office. Call the program directly; they’ll connect you. The PAN Foundation and HealthWell Foundation also offer free counseling. Wait times average 11 minutes, but for Medicare patients, it can be up to 19 minutes. Don’t hesitate to ask for help. Many people get approved only after getting guidance from a navigator.





11 Comments
Nicholas Urmaza
Stop waiting for handouts and get a better job. These programs are a bandaid on a gunshot wound. If you can’t afford your meds, maybe you shouldn’t be living like you’re rich. I’ve seen people on PAPs driving new trucks and eating out every night. Wake up.
RUTH DE OLIVEIRA ALVES
It is imperative to acknowledge the structural inequities that render patient assistance programs not merely helpful, but indispensably life-sustaining for a significant segment of the American populace. The bureaucratic labyrinth inherent in these programs reflects a systemic failure to ensure equitable access to essential therapeutics. One must not conflate eligibility criteria with moral worthiness.
Nilesh Khedekar
Ohhhhh, so now we’re supposed to be grateful that Big Pharma lets us beg for our own medicine??? And they get tax breaks for it??? Hahahaha. You think this is charity? No. This is PR with a side of extortion. They charge $100,000 for a drug, then ‘help’ you get it for free if you jump through 17 hoops. Genius. Just genius.
Jami Reynolds
Did you know that the IRS and pharmaceutical companies share data under a secret agreement called Project HARMONY? That’s how they know who’s lying about income. Your TurboTax submission? It’s being monitored. If you’re even $1 over the limit, your name goes into a database flagged for ‘medication noncompliance risk.’ They’re not helping you-they’re profiling you.
Crystel Ann
I know someone who spent six months trying to get insulin through a PAP. She had to call her doctor’s office three times a week just to get the form signed. Finally got approved. Then they changed her dosage and she had to start over. It’s exhausting. People shouldn’t have to fight this hard to stay alive.
Nat Young
Let’s be real-these programs are designed to fail. The income thresholds? Arbitrary. The documentation? Deliberately confusing. The turnaround time? Engineered to make people give up. And guess who benefits? The same companies that lobby against price caps. This isn’t a safety net. It’s a trapdoor with a pretty sign on it.
Niki Van den Bossche
The very architecture of these programs is a grotesque ballet of performative benevolence-each form a sonnet of bureaucratic despair, each denial letter a haiku of capitalist indifference. We have commodified compassion to such a degree that the act of surviving has become a performance art piece titled ‘The Cost of Breath.’ And yet, we applaud the actors for their grace under duress. How profoundly, devastatingly, elegantly cruel.
Jan Hess
My cousin got approved for her rheumatoid arthritis med last year after three tries. She said the patient navigator saved her life. Seriously, if you’re struggling, call the number. Don’t try to do it alone. They’re there to help. I wish I’d known sooner.
Haley Graves
You don’t have to be perfect to qualify. You just have to be persistent. I’ve helped three friends get through this process. The hardest part isn’t the income limit-it’s believing you deserve help. You do. Start with the manufacturer’s website. Don’t wait until you’re out of pills.
Diane Hendriks
This country is falling apart because we let corporations run healthcare. We used to be a nation that valued hard work and self-reliance. Now we’re begging Big Pharma for scraps like beggars. Shame on us. And shame on the politicians who let this happen. We need to take back our health system-not rely on charity from the same companies that price-gouge us.
ellen adamina
My mom got denied because they said her household size was wrong. She lives with her sister’s kid who helps pay rent. The form didn’t say if that counted. She cried. I called the help line. They said ‘it depends.’ That’s not a policy. That’s a joke.