Adverse Reactions: What They Are, Why They Happen, and How to Stay Safe
When you take a pill, you expect it to help—not hurt. But adverse reactions, unexpected and harmful responses to medications that aren’t part of the intended effect. Also known as adverse drug reactions, these events range from mild rashes to life-threatening organ damage. They’re not rare. In fact, one in five hospital admissions in the U.S. is linked to a bad reaction to a drug someone was taking as prescribed. And it’s not always about dosage or mistakes—it’s often about your body’s unique biology.
That’s where pharmacogenetic testing, a way to see how your genes affect how your body processes drugs comes in. Some people metabolize drugs too fast, making them useless. Others metabolize too slow, causing toxic buildup. Studies like PREPARE have shown that testing for these genetic differences cuts serious adverse reactions by nearly half. It’s not science fiction—it’s already being used in clinics to avoid dangerous interactions with blood thinners, antidepressants, and chemo drugs.
But testing isn’t the whole story. Even when you’re genetically low-risk, adverse reactions still happen because of other drugs you’re taking, what you eat, or even how old you are. That’s why adverse event reporting, the system where doctors and pharmacists flag unexpected side effects is so critical. Every report adds to a growing database that helps regulators spot patterns—like a new drug causing liver damage in older adults, or a generic version triggering seizures in a small group of patients. These reports don’t just help the next person—they save lives.
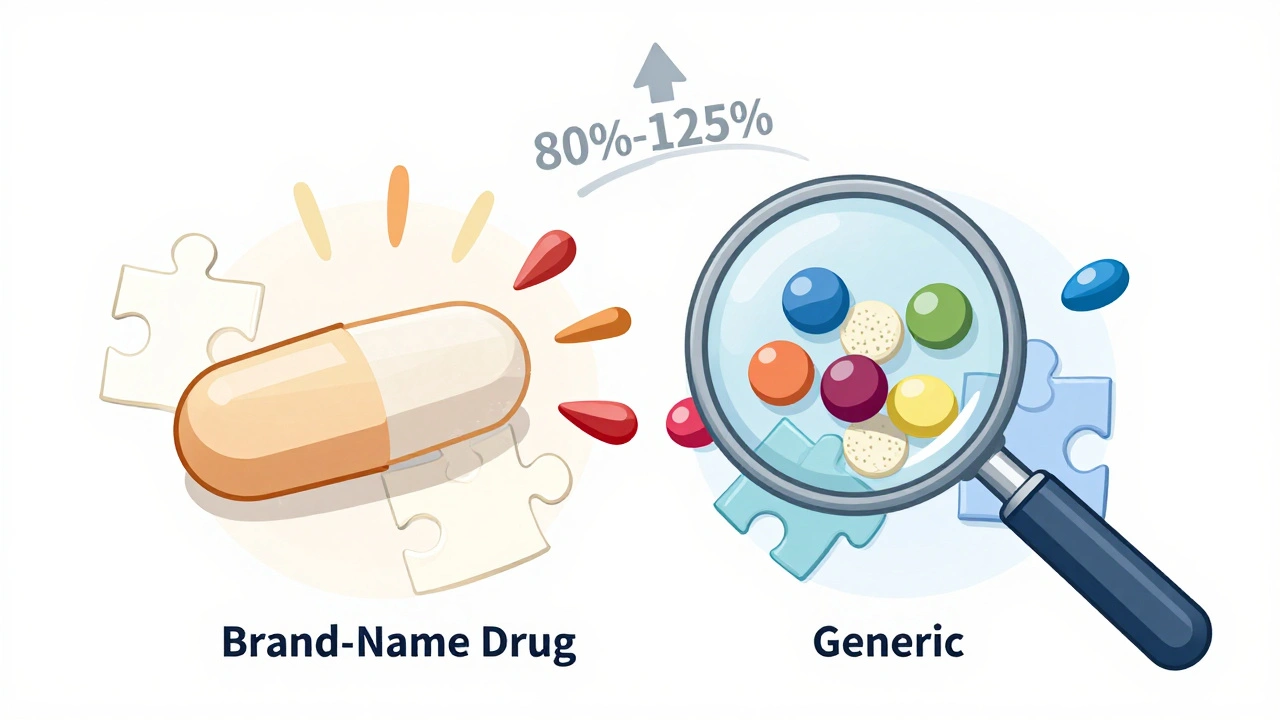
And it’s not just about the drug itself. Sometimes, the problem is how it’s made. For drugs with a narrow therapeutic index, even tiny differences in how a generic version is absorbed can mean the difference between healing and harm. That’s why the FDA and EMA require stricter bioequivalence rules for these drugs—measuring Cmax and AUC to make sure the peak levels and total exposure match the brand. One percent off might sound small, but for drugs like warfarin or lithium, it’s enough to cause a bleed or a seizure.
What you’ll find here isn’t theory. It’s real cases. Real data. Real stories from people who’ve been affected—and from the pharmacists, researchers, and doctors working to stop it before it happens. You’ll learn how to spot warning signs before they turn dangerous, why some people react badly to common meds while others don’t, and how simple changes in how you take your pills can make all the difference. This isn’t about fear. It’s about control. Knowing what to watch for, who to tell, and when to ask for help turns you from a passive patient into an active guardian of your own health.