Cmax: What It Means for Generic Drug Effectiveness and Safety
When you take a generic drug, you expect it to work just like the brand-name version. That’s where Cmax, the maximum concentration of a drug in the bloodstream after dosing. Also known as peak plasma concentration, it’s one of the two main numbers regulators use to decide if a generic is safe and effective. If Cmax is too low, the drug won’t work. If it’s too high, you could get serious side effects. It’s not just a lab number—it’s your safety line.
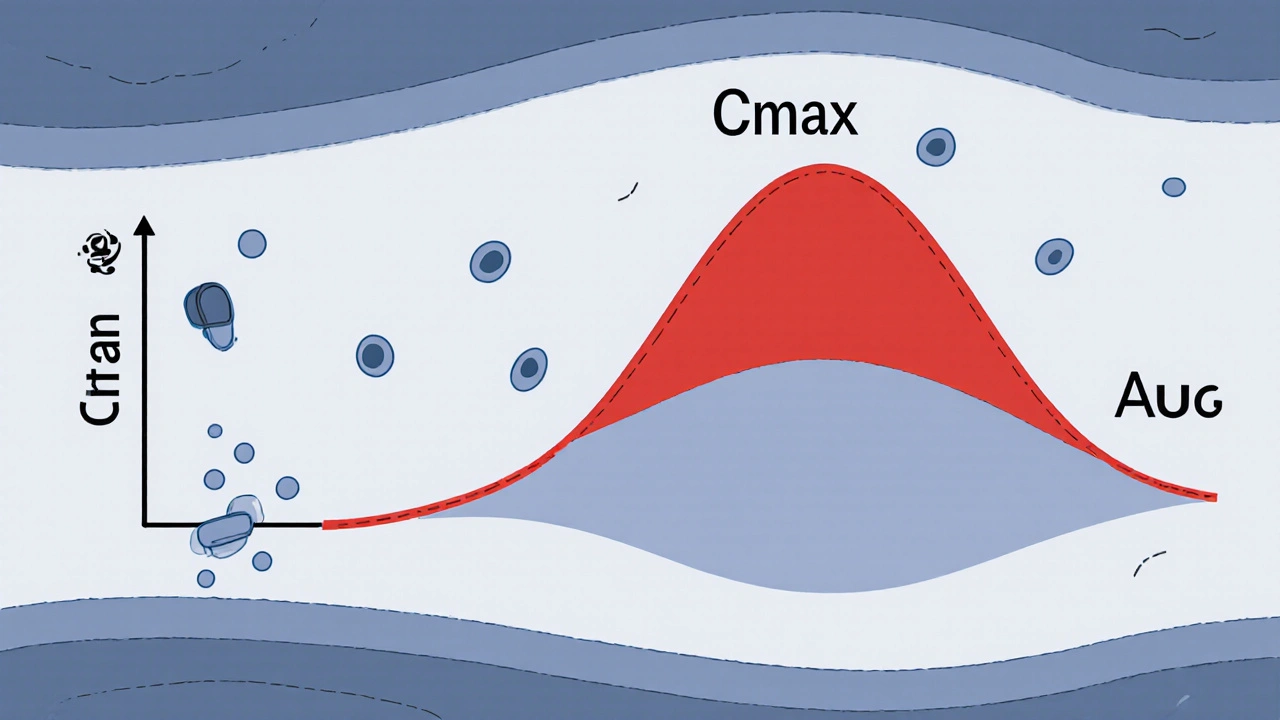
Cmax doesn’t work alone. It’s always paired with AUC, the total exposure of the drug in your body over time. Together, they tell the full story: how fast the drug gets into your blood (Cmax) and how long it stays there (AUC). The FDA, EMA, and other agencies require both to be within strict ranges for generic drugs to be approved. For example, with drugs like warfarin or levothyroxine, even a 10% difference in Cmax can cause dangerous bleeding or thyroid problems. That’s why bioequivalence studies don’t just check if the pill looks the same—they track how your body actually handles it.
These studies use healthy volunteers, give them the brand and generic versions on different days, then draw blood at regular intervals to map out the drug’s journey. The results? A curve showing when the drug peaks (Cmax) and how much it builds up (AUC). If those curves match closely enough, the generic gets the green light. But it’s not just about math—it’s about real people. A pharmacy tech in Ohio once told me a patient switched to a generic antidepressant and started having panic attacks. Turned out, the new version had a higher Cmax, and the body couldn’t adjust fast enough. That’s why these rules exist: to stop surprises before they happen.
Some drugs are more sensitive than others. Narrow therapeutic index drugs, medications where the difference between a helpful dose and a toxic one is very small, need tighter Cmax controls. That’s why generics for drugs like digoxin, cyclosporine, or phenytoin face extra scrutiny. Even small changes in absorption can shift you from safe to dangerous. And it’s not just about the pill—it’s about what’s in it. Fillers, coatings, and manufacturing methods can all affect how quickly the drug dissolves, which directly changes Cmax.
What you’ll find below are real, practical posts that break down how Cmax shapes everything from generic approval to patient safety. You’ll learn how pharmacists spot risky generics, why some drugs can’t be swapped without warning, and how the same number that saves money can also save lives—or cost them. No fluff. Just the facts that matter when your health is on the line.