HVPG: What It Is, Why It Matters, and How It’s Used in Liver Disease
When doctors need to know how much pressure is building up in the liver’s blood vessels, they turn to HVPG, hepatic venous pressure gradient, a direct measurement of pressure differences in the liver’s veins. Also known as hepatic venous pressure gradient, it’s not just a number—it’s a lifeline for people with advanced liver disease. This test tells clinicians whether blood is struggling to flow through a scarred liver, which is the root cause of dangerous complications like bleeding varices and fluid buildup in the belly.
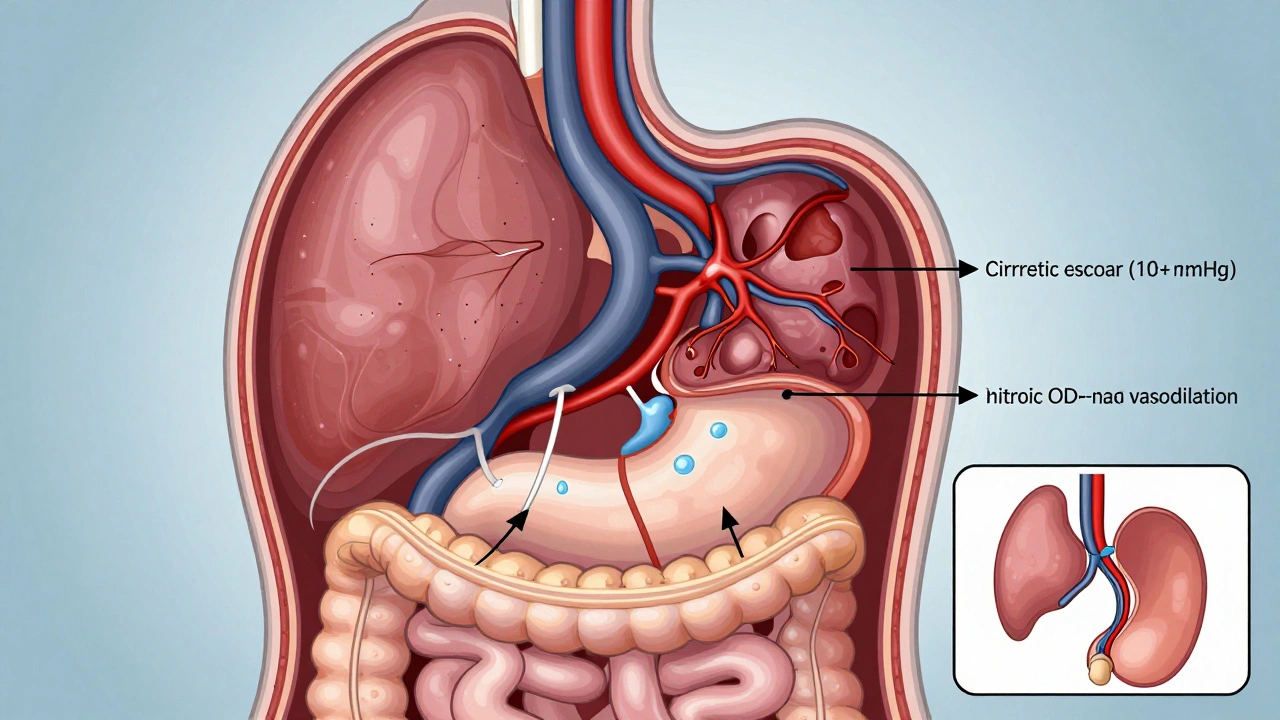
HVPG is closely tied to portal hypertension, elevated blood pressure in the portal vein that carries blood from the intestines to the liver. When the liver gets damaged—say, from long-term alcohol use, hepatitis, or fatty liver disease—it stiffens. Blood can’t flow through easily. That’s when pressure rises. An HVPG reading above 10 mmHg means portal hypertension is present. Above 12 mmHg, the risk of bleeding from swollen veins in the esophagus jumps sharply. Above 16 mmHg? That’s a red flag for life-threatening complications. This isn’t guesswork. It’s backed by decades of clinical data and used in hospitals worldwide to decide who needs treatment, who needs a transplant, and who can be monitored.
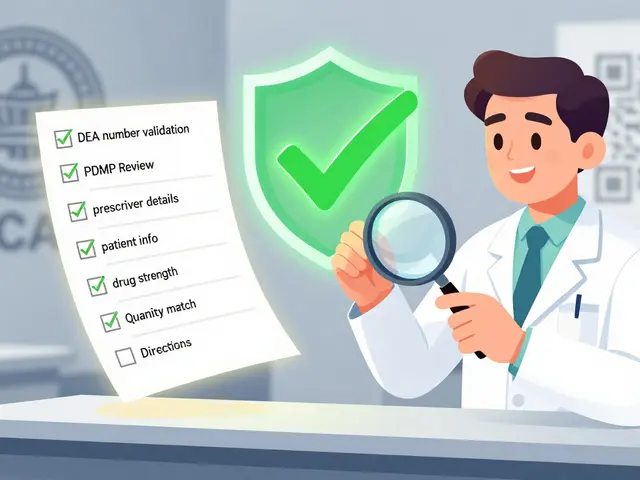
HVPG doesn’t work alone. It’s paired with other tools like ultrasound, endoscopy, and liver function tests. But unlike blood tests that show liver enzymes are high, HVPG shows the actual mechanical stress inside the organ. It’s why doctors use it to track how well a treatment is working. If a patient takes a drug like propranolol to lower pressure, and their HVPG drops by 20% or more, their chance of surviving without a major bleed improves dramatically. It’s also used to evaluate new drugs for cirrhosis—researchers measure HVPG before and after treatment to see if a therapy actually reduces liver pressure.
For patients with liver cirrhosis, the final stage of chronic liver damage where healthy tissue is replaced by scar tissue, HVPG is often the deciding factor in whether they get a transplant. If their HVPG stays high despite treatment, their risk of death within a year climbs. That’s why it’s not just a diagnostic tool—it’s a prognostic one. And for those with liver disease, a broad term covering everything from fatty liver to hepatitis to cancer, understanding HVPG helps make sense of why certain medications are prescribed, why endoscopies are scheduled, and why lifestyle changes aren’t optional.
What you’ll find in the posts below are real-world connections to HVPG—not just theory. From how it relates to drug safety in patients with liver damage, to how treatments for cirrhosis are tested using HVPG as a benchmark, to how managing portal hypertension affects everything from diet to medication choices. These aren’t abstract concepts. They’re the measurable, life-changing numbers doctors use every day to keep people alive.