IBS Symptoms: What They Are, How They Feel, and What Actually Helps
When you have irritable bowel syndrome, a common functional gut disorder that causes chronic digestive discomfort without visible damage to the intestines. Also known as spastic colon, it doesn’t show up on scans or blood tests—but the pain, bloating, and bathroom chaos feel very real. If you’ve ever been stuck in a restaurant bathroom, canceled plans because your stomach was acting up, or spent hours Googling "why does my gut hurt after coffee?"—you’re not alone. IBS affects about 1 in 7 people worldwide, and most of them don’t know what’s really going on inside their gut.
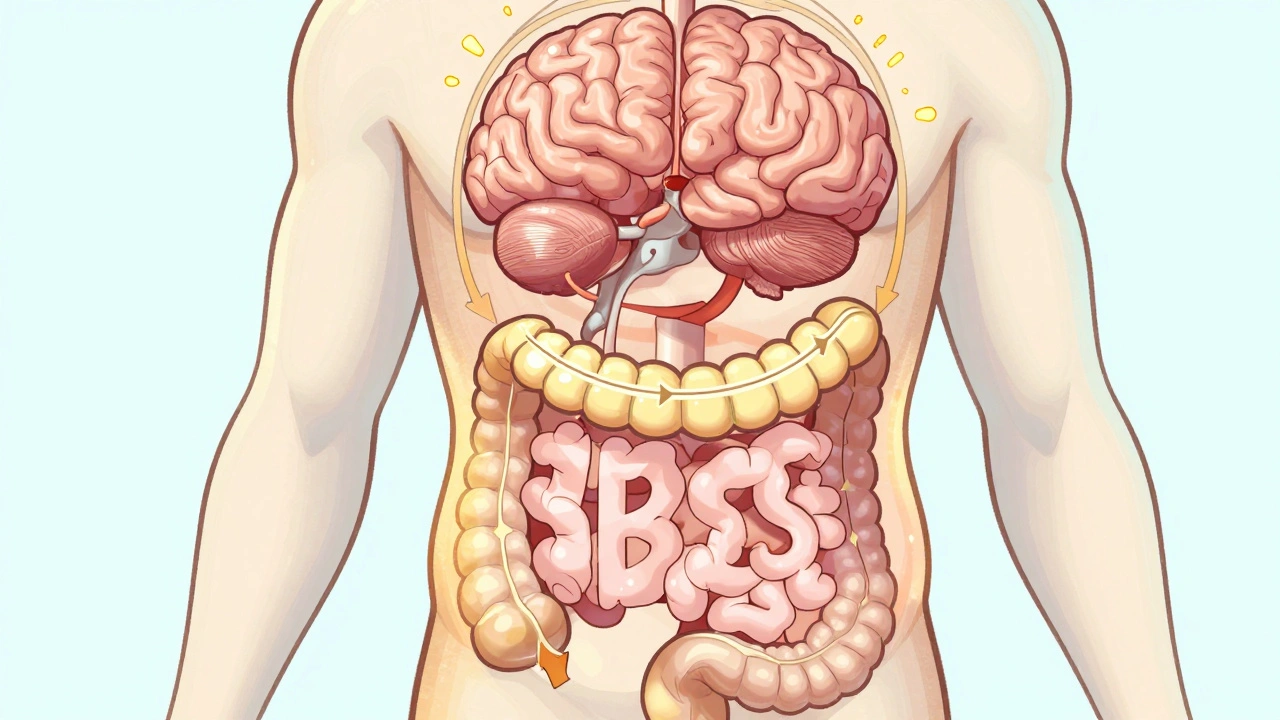
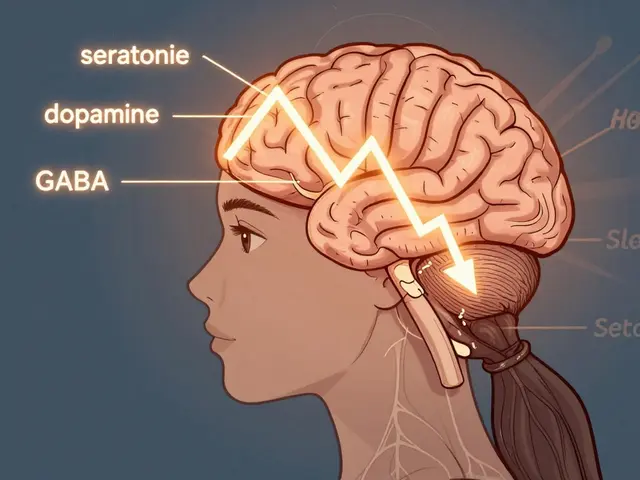
The IBS symptoms, the hallmark signs that define this condition. Also known as bowel dysfunction, they come in patterns: some people get constant diarrhea, others are stuck in constipation mode, and many swing between both. Cramping that eases after a bowel movement? Classic. Bloating so bad your clothes feel tight by noon? Common. The gut doesn’t just hurt—it feels alive, unpredictable, and sometimes cruel. And while stress doesn’t cause IBS, it sure makes it worse. Your gut and brain are wired together, and when anxiety spikes, so do the cramps. You might also notice mucus in your stool, a feeling that you haven’t fully emptied your bowels, or sudden urges that feel impossible to ignore. These aren’t "just nerves." They’re biological signals your body sends when its gut-brain axis is out of sync.
What makes IBS so frustrating is that it looks normal on tests but feels anything but. No tumors, no infections, no inflammation—just a gut that’s overly sensitive and reacts strongly to things most people ignore: dairy, onions, artificial sweeteners, or even a big meal. The digestive discomfort, the daily reality for millions living with IBS. Also known as functional gut pain, it’s not in your head—it’s in your nerves, your gut microbes, and your body’s response to food and stress. There’s no magic pill, but people find relief by tracking triggers, adjusting fiber, trying low-FODMAP diets, and learning how to calm their nervous system. Some find help with peppermint oil, probiotics, or even hypnotherapy. It’s not one-size-fits-all, but it’s manageable.
Below, you’ll find real stories and science-backed tips from people who’ve been where you are—struggling with bloating, rushing to the bathroom, and wondering if they’ll ever feel normal again. These aren’t generic lists. They’re practical, tested strategies that actually work for real lives.