IBS Treatment: What Actually Works
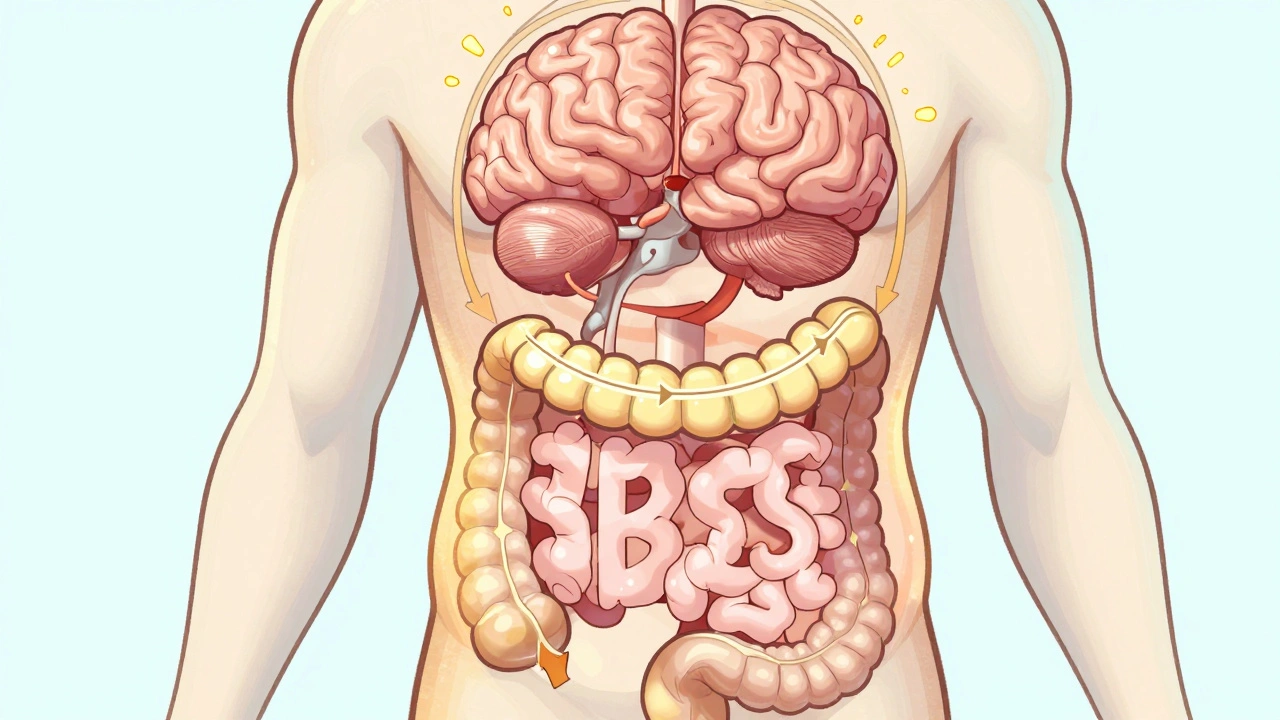
When you have irritable bowel syndrome, a chronic condition causing abdominal pain, bloating, and changes in bowel habits without visible damage to the digestive tract. Also known as spastic colon, it affects nearly 1 in 5 adults and isn’t just "bad digestion"—it’s a real disruption to daily life. Many people try everything from elimination diets to expensive supplements, only to feel worse. The truth? IBS treatment isn’t about one magic pill or cure. It’s about matching your triggers to proven, science-backed strategies.
What you eat plays a huge role. A low-FODMAP diet isn’t a fad—it’s backed by clinical trials showing symptom reduction in up to 70% of people. Foods like onions, garlic, wheat, and certain fruits can ferment in the gut and trigger bloating and cramps. Cutting them out temporarily, then slowly reintroducing them, helps you find your personal triggers. Probiotics, live bacteria that help balance gut flora can also help, but not all are equal. Strains like Bifidobacterium infantis and Lactobacillus plantarum have shown real results in reducing pain and gas. Then there’s gut health, the overall balance of microbes and function in your digestive system. Stress, sleep, and even how fast you eat affect it. You can’t fix your gut if you’re rushing meals while scrolling on your phone.
Medications like antispasmodics or low-dose antidepressants aren’t just for anxiety—they help calm overactive nerves in the gut. But they work best when paired with lifestyle changes. There’s no point taking a pill if you’re still eating trigger foods or skipping sleep. And forget the idea that IBS is "all in your head." It’s real, measurable, and treatable. What you’ll find below are clear, no-fluff guides on what to eat, what to avoid, how to track symptoms, and which meds actually help without side effects. No guesswork. No hype. Just what works.