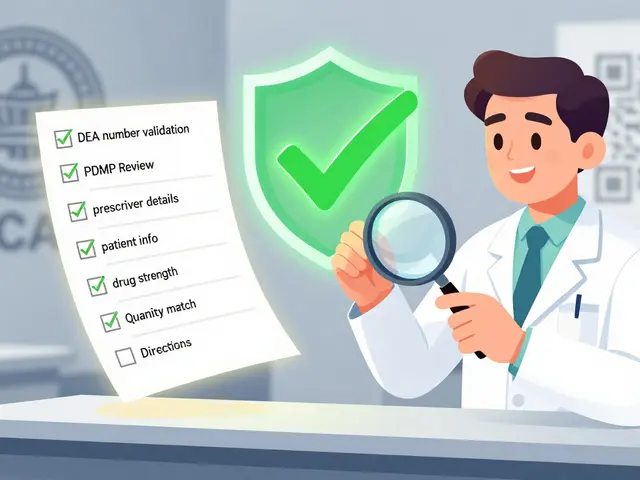
Patient Checklist: Essential Steps for Safer Medication Use
When you’re on medication, a patient checklist, a simple, personalized list of actions to reduce medication errors and improve safety. Also known as a medication action plan, it’s not just a reminder—it’s your shield against preventable harm. Too many people assume their doctor or pharmacist has everything under control. But studies show over 70% of serious drug errors happen because critical details were missed by the patient—like not knowing a new pill interacts with their blood thinner, or ignoring a weird rash because they thought it was "just allergies."
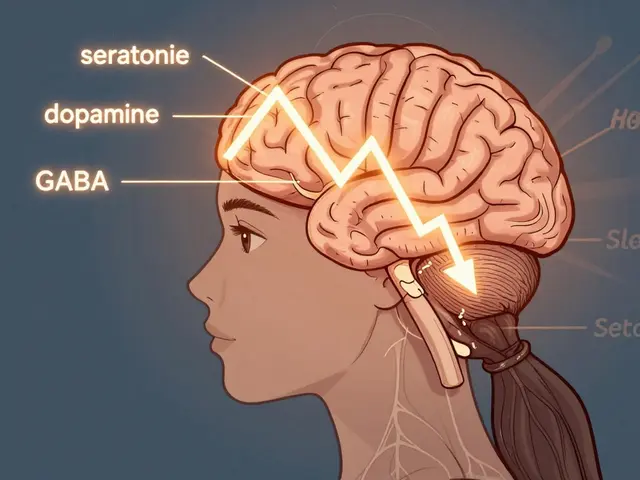
A real patient checklist starts with three things: knowing what you’re taking, understanding why, and spotting when something’s wrong. That means writing down every drug—even the over-the-counter ones and supplements. It means asking your pharmacist: "Is this a generic? Does it have different fillers than what I used before?" Because that’s where side effects sometimes hide. If you’re on a drug with a narrow therapeutic index—like warfarin or lithium—your checklist should include daily symptom tracking and regular blood tests. And if you’ve had strange reactions to meds before, ask about pharmacogenetic testing, a blood test that shows how your genes affect how your body processes drugs. It’s not sci-fi—it’s now covered by some insurers and can stop a dangerous reaction before it starts.
Don’t forget the basics: check expiration dates, store pills away from heat and humidity, and never skip doses just because you feel fine. Many people stop their antibiotics early or skip their blood pressure med when their numbers look good. That’s how resistance and relapse happen. And if you’re switching from a brand-name drug to a generic drug, a chemically identical, lower-cost version of a brand-name medication, watch for changes in how you feel. Not because generics are unsafe—most are perfect—but because the fillers, coatings, or manufacturing can trigger reactions in sensitive people. That’s why reporting side effects to your pharmacist matters. Your report helps others.
And if you’re managing a chronic condition—like liver disease, autoimmune issues, or IBS—your checklist should include diet, sleep, and stress habits. A liver-healthy diet isn’t just a suggestion; it’s part of your treatment plan. Stress can trigger IBS flare-ups. Poor sleep messes with how your body metabolizes meds. These aren’t side notes—they’re core parts of your care. The posts below cover everything from how to read a boxed warning on your prescription label, to why bioequivalence studies matter for your safety, to what to do if you bleed on a blood thinner. This isn’t theory. It’s what real people use to stay out of the ER. Use the checklist. Track your changes. Speak up. Your life depends on it.