Personalized Medicine: Tailored Treatments Based on Your Genetics and Health
When you take a drug, it doesn’t work the same for everyone. That’s where personalized medicine, a healthcare approach that customizes treatment based on individual differences in genes, environment, and lifestyle. Also known as precision medicine, it moves away from the one-size-fits-all model and asks: What works for you? This isn’t science fiction—it’s happening right now in clinics, pharmacies, and research labs. Doctors are starting to use your DNA to pick the right drug, at the right dose, before you even start treatment.
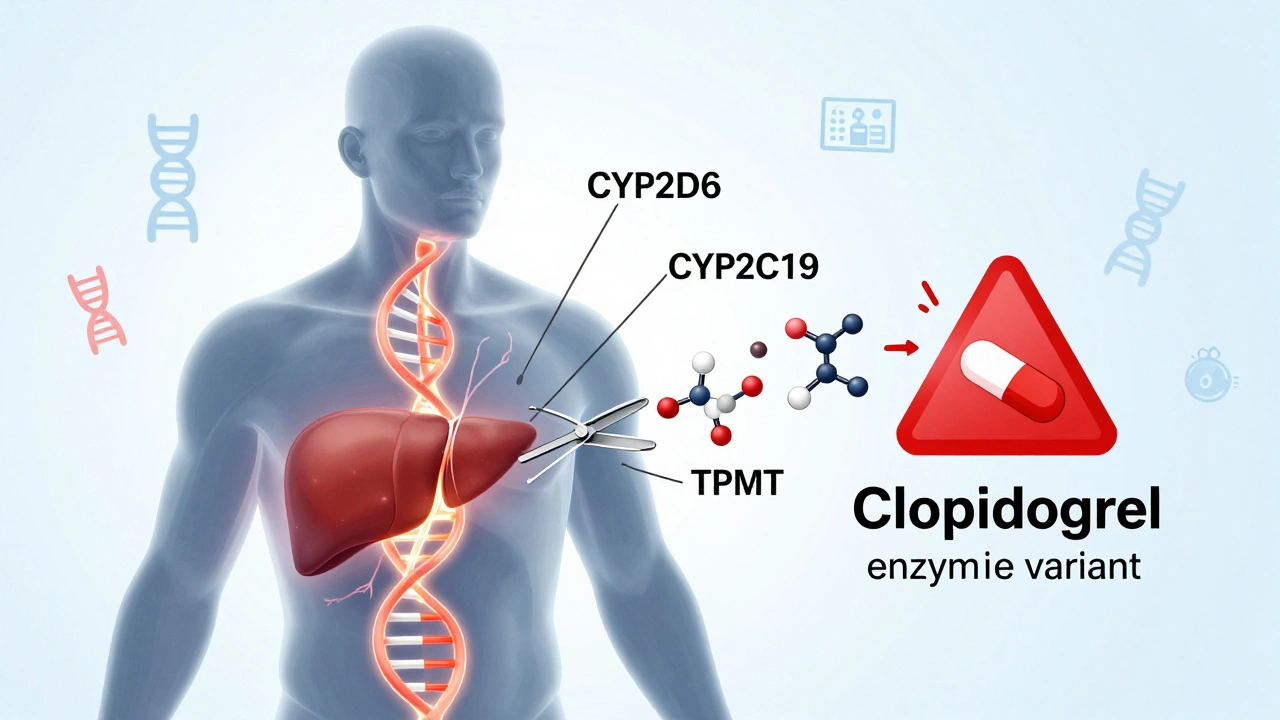
At the heart of this shift is pharmacogenomics, the study of how genes affect how your body responds to medications. For example, some people metabolize blood thinners like warfarin too fast—so they need a higher dose. Others process them too slow, making even a normal dose dangerous. Genetic tests can spot these differences before a prescription is written. It’s not just about avoiding side effects; it’s about making sure the drug actually works. This same logic applies to cancer drugs. Instead of giving everyone the same chemo, oncologists now test tumors for specific mutations and match them to drugs that target those exact changes. That’s targeted therapy, a treatment designed to attack specific molecules involved in disease progression—and it’s why some patients see dramatic improvements while others don’t respond at all.
Personalized medicine doesn’t stop at genes. It also looks at your lifestyle, age, other conditions, and even your gut bacteria. That’s why posts here cover everything from how liver health affects drug metabolism to why bioequivalence rules matter for generics. If you’ve ever wondered why your friend’s medication worked while yours didn’t, or why your doctor ordered a genetic test before prescribing something, this collection answers those questions. You’ll find real examples: how narrow therapeutic index drugs need tighter controls, how adverse event reporting helps improve safety for everyone, and how tools like Cmax and AUC measurements prove a generic version behaves the same as the brand. These aren’t abstract ideas—they’re the building blocks of the next era in healthcare.
What you’ll see below isn’t just a list of articles. It’s a roadmap showing how personalized medicine touches real people—whether they’re managing IBS, fighting liver disease, or taking ED meds like Avana. Each post connects back to one core idea: treatment should fit the patient, not the other way around.