Pharmacogenetic Testing: How Your Genes Affect Medication Response
When you take a pill, your body doesn’t just absorb it the same way everyone else does. Your genes decide how fast it breaks down, how strong the effect is, and whether you’ll have dangerous side effects. This is where pharmacogenetic testing, a medical test that analyzes how your DNA affects your response to drugs. Also known as genetic drug testing, it helps doctors pick the right medication and dose for you — not just based on your symptoms, but your biology. It’s not science fiction. It’s already being used for antidepressants, blood thinners, cancer drugs, and pain meds.
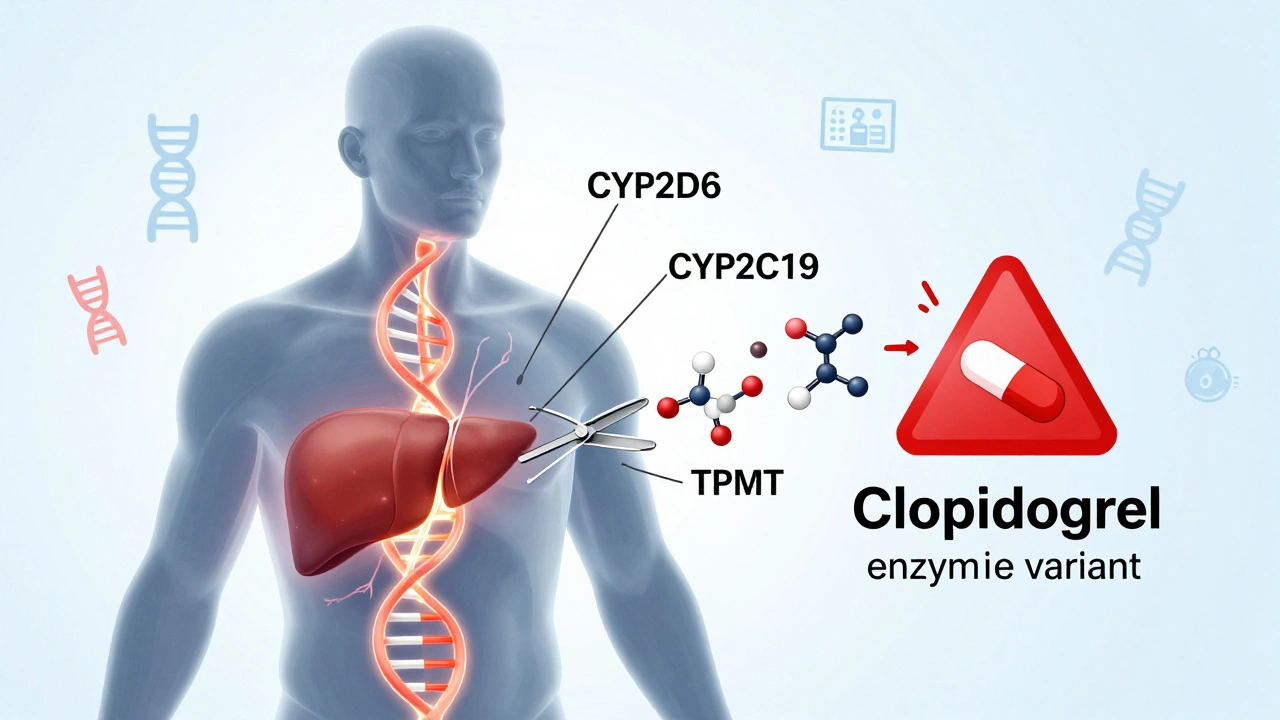
One of the biggest players in this game is the CYP450 enzyme system, a group of liver proteins that break down over 70% of all prescription drugs. Also known as cytochrome P450, these enzymes vary wildly from person to person. Some people are ultra-rapid metabolizers — they clear drugs too fast, making them useless. Others are slow metabolizers — they build up toxic levels even on normal doses. That’s why two people taking the same antidepressant can have totally different outcomes: one feels better, the other gets dizzy and nauseous. Pharmacogenetic testing spots these differences before you even swallow the first pill. It’s especially critical for drugs with a narrow therapeutic index, medications where the difference between a helpful dose and a dangerous one is very small. Also known as NTI drugs, these include blood thinners like warfarin, seizure meds like phenytoin, and chemo drugs like 5-FU. A wrong dose here isn’t just ineffective — it can kill you. That’s why hospitals and clinics are starting to test patients before prescribing them.
Pharmacogenetic testing doesn’t just help avoid bad reactions — it can save money and time. Instead of trying three different antidepressants over six months, a test might point straight to the one that works. It’s why big health systems now offer it for patients with chronic conditions, mental health issues, or those on multiple medications. And it’s not just for adults. Kids with epilepsy or teens on ADHD meds are also benefiting from this precision approach.
What you’ll find in the posts below are real-world examples of how this science plays out. From how genetic differences affect chemo safety to why some people can’t tolerate common painkillers, these articles show you the hidden link between your DNA and your medicine. You’ll see how pharmacists track drug reactions, how bioequivalence rules protect you, and why your genetic profile might be the missing piece in your treatment plan. This isn’t theory. It’s happening right now — and it’s changing how medicine is done.