Pharmacokinetics: How Your Body Absorbs, Uses, and Gets Rid of Drugs
When you take a pill, it doesn’t just sit there and work. Pharmacokinetics, the study of how drugs move through the body over time. Also known as ADME, it stands for Absorption, Distribution, Metabolism, and Excretion—the four stages that decide if a drug will help you, hurt you, or do nothing at all. This isn’t just lab jargon. It’s the reason your generic blood pressure pill works just like the brand-name version—and why some drugs need strict rules to stay safe.
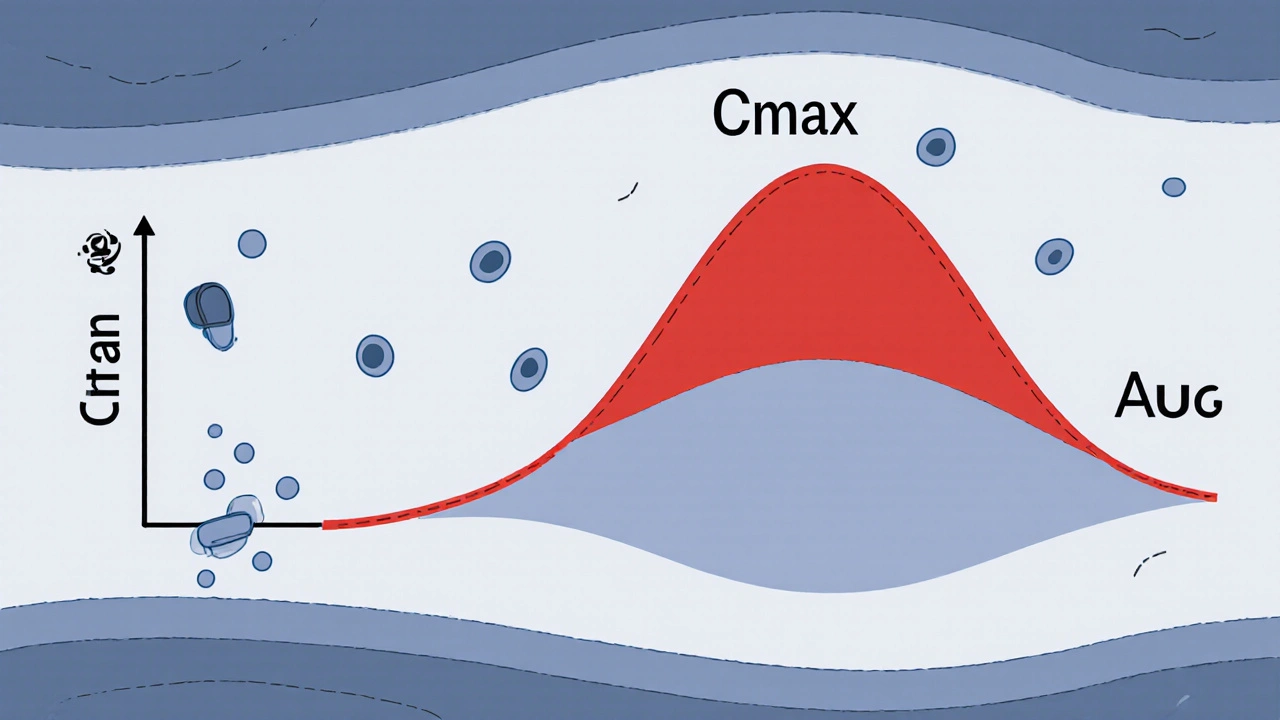
Take bioequivalence, the process of proving two drugs behave the same way in the body. If a generic version doesn’t match the original in how fast and how much it enters your bloodstream, you could get too little (and the drug won’t work) or too much (and you risk side effects). That’s why regulators like the FDA look at Cmax and AUC, two key measurements that track peak drug levels and total exposure over time. These numbers aren’t guesses—they’re based on real data from volunteers who take the drug and have their blood tested at set intervals. If Cmax and AUC fall within 80–125% of the brand drug’s values, the generic is approved. This is how your $5 pill ends up just as effective as the $50 one.
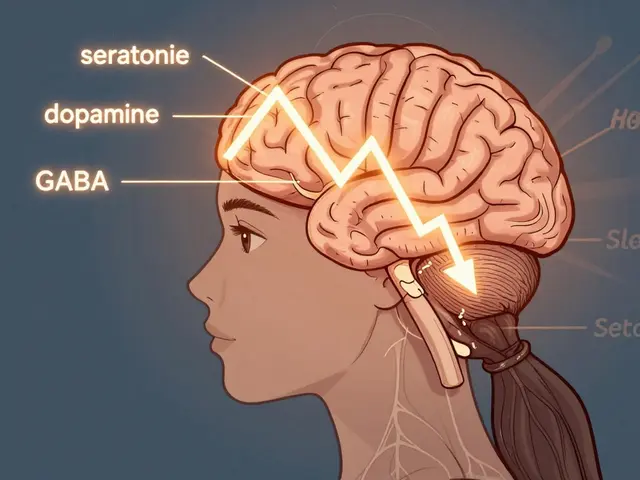
But pharmacokinetics doesn’t stop at generics. It explains why grapefruit ruins your statin, why some antibiotics need to be taken on an empty stomach, and why liver disease can turn a safe dose into a dangerous one. Your body breaks down drugs in the liver, filters them through the kidneys, and stores some in fat tissue. If any of those systems are off, the drug’s journey changes—and so does your risk. That’s why doctors adjust doses for older adults, people with kidney problems, or those on multiple meds. Even something as simple as timing matters: a drug taken with food might absorb slower, delaying its effect. That’s pharmacokinetics in action.
Behind every safe, effective medication is a mountain of pharmacokinetic data. It’s why chemotherapy doses are so precise, why blood thinners need regular checks, and why some drugs carry black box warnings. The posts below dig into real-world cases where this science makes a difference—whether it’s how bioequivalence studies keep generics safe, why certain drugs interact dangerously with others, or how liver health changes how your body handles medication. You’ll find practical insights from pharmacists, patients, and researchers who see this science every day. No theory without results. Just clear, useful facts about how your body deals with drugs—and what that means for you.