Torsemide Onset Time Calculator
Estimate how quickly your torsemide begins working based on key factors
Torsemide is a potent loop diuretic used to treat fluid overload, high blood pressure, and heart‑failure symptoms. Understanding how fast it kicks in helps patients set realistic expectations and avoid unnecessary worry. Below we break down the science, the factors that speed up or slow down the effect, and what you should look for after the first dose.
How Torsemide Works in the Body
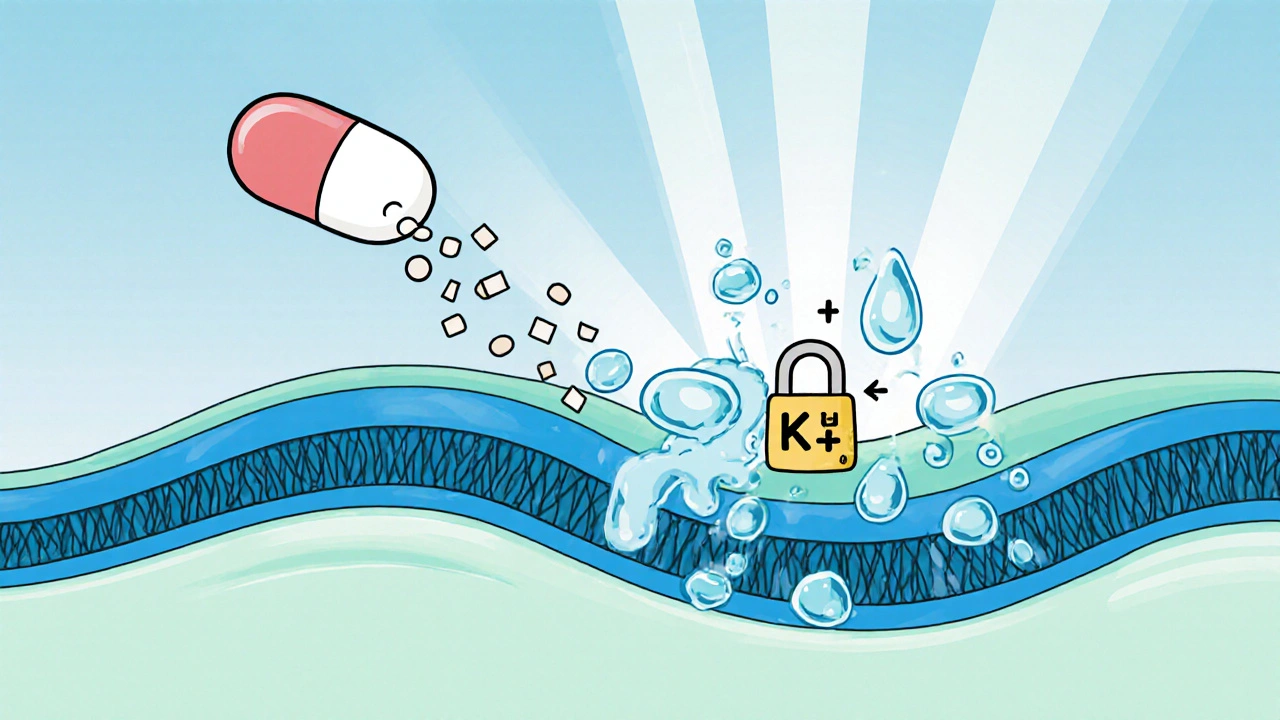
Torsemide blocks the sodium‑potassium‑chloride (Na⁺‑K⁺‑2Cl⁻) transporter in the thick ascending limb of the loop of Henle. By stopping this transporter, the kidney can’t re‑absorb sodium and chloride, so water follows the salt into the urine. The result is a rapid diuresis that reduces swelling (edema) and lowers blood volume, which in turn eases blood‑pressure and heart‑failure strain.
Pharmacokinetics: From Swallow to Effect
The journey of a pill or an IV dose can be split into four key steps:
- Absorption: Oral torsemide is well‑absorbed, reaching peak plasma concentrations in about 1‑2 hours. The drug’s bioavailability hovers around 80‑100 %.
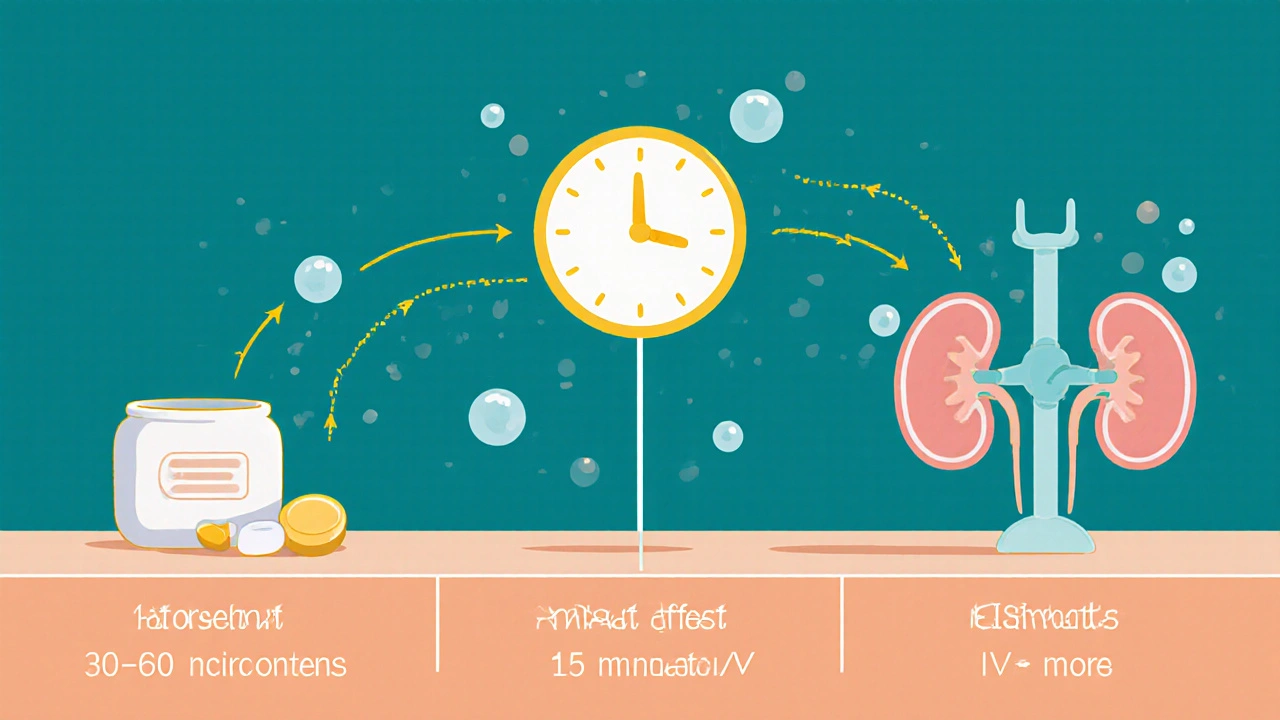
- Onset of Action: Clinically visible urine output usually begins within 30‑60 minutes for most adults; this is the point where the torsemide onset is felt.
- Peak Effect: Maximal diuretic response typically appears 2‑4 hours after an oral dose, though IV administration can bring peak response in 30‑60 minutes.
- Elimination: The drug’s half‑life is about 3‑4 hours, and it is cleared mainly by the kidneys. Residual diuretic activity can linger up to 12 hours.
These timelines are averages; individual experiences can vary.
Factors That Influence How Quickly Torsemide Starts Working
Several variables can speed up or delay the onset:
- Formulation: Tablets, extended‑release tablets, and IV injections differ. IV gives the fastest effect, while extended‑release tablets may delay onset by an extra hour.
- Food Intake: Taking torsemide with a heavy, fatty meal can slow absorption slightly, pushing the first noticeable urine increase toward the later end of the 30‑60 minute window.
- Kidney Function: Impaired renal clearance (eGFR < 30 mL/min) can reduce the drug’s effectiveness and lengthen the time to see a response.
- Dosage: Higher doses (e.g., 40 mg vs 10 mg) produce a stronger diuretic push, often making the onset feel more immediate.
- Concomitant Medications: NSAIDs, for instance, can blunt the diuretic response by reducing renal prostaglandin synthesis.
Clinical Expectations: When Should You Notice Changes?
Knowing the typical timelines helps you gauge whether the drug is doing its job:
| Route | Onset (first urine increase) | Peak Diuretic Effect | Typical Dose Range |
|---|---|---|---|
| Oral tablet | 30‑60 min | 2‑4 hr | 5‑20 mg daily |
| Extended‑release oral | 60‑90 min | 3‑5 hr | 10‑40 mg daily |
| IV injection | Within 15 min | 30‑60 min | 5‑20 mg once‑or twice‑daily |
For most patients with congestive heart failure, you’ll notice a drop in leg swelling or a reduction in shortness of breath within a few hours. Blood‑pressure reductions can be evident in 2‑4 hours, especially when higher doses are used.
How Torsemide Stacks Up Against Other Loop Diuretics
Furosemide (Lasix) and bumetanide (Bumex) are the other big names in the loop‑diuretic family. Their onset profiles differ enough to matter in certain clinical settings.
| Drug | Oral Onset | Peak Effect | Half‑Life | Typical Oral Dose |
|---|---|---|---|---|
| Torsemide | 30‑60 min | 2‑4 hr | 3‑4 hr | 5‑20 mg |
| Furosemide | 60‑120 min | 3‑6 hr | 2‑3 hr | 20‑80 mg |
| Bumetanide | 15‑30 min | 1‑2 hr | 1‑2 hr | 0.5‑2 mg |
In short, bumetanide is the fastest, furosemide is the slowest, and torsemide sits comfortably in the middle with a reliable onset and a longer duration of action, making it a favorite for chronic management.

Practical Tips for Patients Starting Torsemide
- Take it on an empty stomach if you want the quickest effect-wait at least 30 minutes before a big meal.
- Stay hydrated but avoid excessive fluids; the goal is to remove excess fluid, not to dehydrate.
- Watch your weight daily. A loss of 1‑2 kg in the first 24 hours usually signals a good response.
- Check blood pressure after 2‑4 hours; a drop of 5‑10 mmHg is typical.
- Monitor electrolytes (especially potassium and magnesium) after the first few doses, especially if you’re on high doses.
- Know when to call a doctor: if you don’t see any increase in urine output after 2 hours, or if you feel dizzy, have severe cramps, or notice sudden swelling.
Common Concerns and Myths
Myth: “If I don’t see a change in the first hour, the drug isn’t working.”
Reality: While many feel the effect within 30‑60 minutes, some patients-particularly those with chronic kidney disease-may need a bit longer. Give it up to 2 hours before deciding it’s ineffective.
Myth: “Torsemide will make me pee nonstop for a day.”
Reality: The drug creates a controlled diuresis. Most people experience a modest increase in urine volume for 6‑12 hours, then return to normal output.
Myth: “I can stop the medication once I feel better.”
Reality: Stopping abruptly can cause fluid rebound, especially in heart‑failure patients. Always taper under a doctor’s guidance.
Frequently Asked Questions
How soon after the first dose should I see a reduction in swelling?
Most people notice less leg or ankle swelling within 2‑4 hours, especially if they took a standard 20 mg oral dose on an empty stomach.
Can I take torsemide with my blood‑pressure meds?
Yes, torsemide is often prescribed together with ACE inhibitors, ARBs, or calcium‑channel blockers. Your doctor will monitor blood‑pressure and potassium levels closely.
What if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one-don’t double‑dose.
Are there foods I should avoid while on torsemide?
High‑salt meals can blunt the diuretic effect, so aim for a low‑sodium diet (under 2 g per day). Also, avoid large amounts of potassium‑rich supplements unless advised.
Can torsemide be used during pregnancy?
It’s classified as Category C. Doctors may prescribe it if the benefits outweigh risks, but it’s not the first‑line choice for pregnant women.
Understanding the timeline of torsemide helps you stay confident, catch any unexpected side effects early, and work with your healthcare provider for the best outcome.






14 Comments
Harry Bhullar
Torsemide’s pharmacokinetic profile makes it a solid choice when you need a predictable diuretic onset, especially compared to furosemide’s variable absorption.
After you swallow the tablet, the drug is rapidly absorbed from the GI tract, hitting peak plasma levels usually within one to two hours.
This rapid rise translates clinically into an increase in urine output as early as 30 minutes, although many patients notice the change a little later, around the one‑hour mark.
When the drug is given intravenously, the timeline compresses dramatically, with measurable diuresis often starting within 15 minutes and peaking in the next half hour.
The reason for this speed is torsemide’s high bioavailability, which hovers between 80 and 100 percent, meaning almost the entire dose reaches systemic circulation.
Kidney function plays a pivotal role; patients with an eGFR below 30 mL/min may experience delayed onset because the drug relies on renal excretion to clear the plasma surge.
Conversely, a higher dose-say 40 mg versus the typical 10 mg-can produce a more pronounced diuretic push, making the onset feel almost immediate to the patient.
Food intake is another modifiable factor; a heavy, fatty meal can slow gastric emptying, nudging the first noticeable urine increase toward the latter end of the 30‑to‑60‑minute window.
Co‑administration with NSAIDs can blunt the effect, as these drugs reduce renal prostaglandin synthesis, which is part of the diuretic’s mechanism of action.
In practice, clinicians often advise taking torsemide on an empty stomach to maximize the speed of onset, and they monitor weight loss of about one to two kilograms in the first 24 hours as a practical gauge of efficacy.
Blood pressure typically drops by five to ten millimeters of mercury within two to four hours, aligning with the peak diuretic effect.
The half‑life of tormodine, around three to four hours, ensures that the effect tapers off gently, providing a smoother fluid balance compared with the sharper peaks and troughs seen with other loop diuretics.
For patients with congestive heart failure, the combination of a reliable onset and a longer duration of action helps prevent the rebound fluid accumulation that can occur with shorter‑acting agents.
It’s also worth noting that torsemide has a lower propensity for causing ototoxicity, a side effect sometimes associated with high‑dose furosemide therapy.
Overall, the predictable pharmacokinetics and manageable side‑effect profile make torsemide a go‑to option when clinicians need both speed and stability in fluid removal.
Giusto Madison
Listen up, if you’re not seeing that urine surge within the first hour, you’re either under‑dosing or you’ve got a hidden renal bottleneck you need to expose.
Don’t blame the drug; check your eGFR, your diet, and any NSAID usage that might be muting the effect.
Take it on an empty stomach and you’ll shave minutes off the onset, which matters when you’re battling acute pulmonary edema.
If IV access is available, push the dose-this cuts the latency to under 15 minutes, giving you the rapid off‑load you demand.
Remember, torsemide’s bioavailability is stellar, so the oral route is still reliable when you follow the protocol.
Stop second‑guessing the timeline and start tweaking the variables that you control.
erica fenty
Torsemide exhibits a high bioavailability (≈ 85‑100%); absorption peaks at 1‑2 h, leading to diuresis in 30‑60 min.
Renal clearance dictates half‑life (3‑4 h), influencing duration of action.
Monitor electrolytes-hypokalemia, hyponatremia can emerge swiftly.
Xavier Lusky
The pharma giants push torsemide as “fast‑acting” to keep patients dependent on prescriptions, while suppressing data on long‑term renal strain.
Ashok Kumar
Oh sure, just pop a pill and expect the swelling to disappear like magic-if you ignore the fact that your kidneys might be too tired to filter it properly.
Jasmina Redzepovic
Let’s set the record straight: torsemide isn’t some experimental fad, it’s a well‑established loop diuretic with pharmacodynamics that outperform many domestic alternatives.
Its natriuretic efficiency, quantified by a fractional excretion of sodium upwards of 30%, eclipses the typical 15‑20% seen with older agents.
Moreover, the drug’s plasma protein binding (≈ 99%) ensures a sustained therapeutic window, crucial for patients with fluctuating volume status.
Ignoring these data points in favor of anecdotal “quick fixes” reflects a misunderstanding of renal physiology.
Anyone serious about cardiovascular care should prioritize evidence‑based dosing schedules over headline‑driven hype.
Esther Olabisi
Wow, looks like you’ve got the whole torsemide timeline down to a science! 😅
Just remember to stay hydrated-though not like you’re training for a marathon-so you don’t swing from “pee‑party” to dehydration.
And if you’re ever feeling dizzy, that’s your body saying “hey, maybe ease off the diuretic dose a tad.” 🤔
Keep an eye on those electrolytes; a quick potassium check can save you a lot of hassle later.
All in all, you’re on the right track-just don’t forget to enjoy the little victories like shedding a kilogram of water weight! 💪
Ivan Laney
Allow me to elaborate on why torsemide should be the cornerstone of our national therapeutic arsenal, especially when confronting the pervasive challenge of fluid overload in heart‑failure patients across the country.
First, the drug’s pharmacokinetic consistency-characterized by its near‑complete oral bioavailability and predictable half‑life-offers clinicians a reliable tool, eliminating the guesswork that plagues less stable diuretics.
Second, the comparative studies consistently demonstrate that torsemide reduces rehospitalization rates more effectively than its counterparts, a metric that directly translates to reduced healthcare expenditures for our public systems.
Third, the safety profile is markedly superior; incidences of ototoxicity and severe electrolyte disturbances are lower, which aligns with our national goal of minimizing iatrogenic complications.
Furthermore, the drug’s versatility-available in oral, extended‑release, and intravenous formulations-allows seamless transition from acute care settings to outpatient management without sacrificing efficacy.
Critics may argue that cost is a barrier, but when you factor in the downstream savings from fewer readmissions and shorter ICU stays, torsemide actually proves to be cost‑effective in the long run.
In addition, its synergistic compatibility with ACE inhibitors and ARBs enhances blood‑pressure control, reinforcing the multimodal approach advocated by our leading cardiology societies.
Let’s not overlook the pharmacodynamic advantage: its stronger blockade of the Na⁺‑K⁺‑2Cl⁻ transporter translates into a more potent natriuretic response, crucial for patients with refractory edema.
By standardizing torsemide usage across our hospitals, we can also streamline pharmacy inventories, reducing logistical complexities inherent in managing multiple diuretic agents.
Ultimately, embracing torsemide is not merely a clinical decision but a strategic move that supports the health of our nation’s citizens and the sustainability of our medical infrastructure.
Kimberly Lloyd
When we view torsemide not just as a medication but as a bridge between the body’s fluid equilibrium and the mind’s sense of relief, its onset time becomes a metaphor for how swiftly change can begin when the right conditions are met.
Patience and mindfulness in monitoring weight and blood pressure allow the subtle early signs of diuresis to be appreciated without panic.
In this way, the drug teaches us that even gradual shifts can culminate in profound improvement.
John Price
Exactly, tracking daily weight is a simple yet powerful indicator of torsemide’s effectiveness.
Nick M
Torsemide’s quick action is just another pharma trick.
Brandy Eichberger
While the exposition is thorough, I would suggest a more nuanced discussion of torsemide’s comparative pharmacodynamics, perhaps integrating recent meta‑analyses that delve into its impact on morbidity beyond mere diuresis.
Eli Soler Caralt
i guess torsemide’s onset is like a quiet whisper of change, subtle but undeniable 🌟.
Eryn Wells
Great summary! 🩺 Remember, staying informed and sharing experiences helps everyone navigate their treatment journeys more confidently. 🙌